Direct risk factors
Trauma – fracture, dislocation
Sickle cell disease
Human immunodeficiency virus infection
Chemotherapy
Radiation
Indirect risk factors
Corticosteroids
Alcohol abuse
Tobacco use
Systemic lupus erythematosus
Myeloproliferative disorders
Gaucher’s disease
Organ transplant
Renal failure
Coagulation abnormalities
Pregnancy
Genetic factors
Table 38.2
Ficat and Arlet staging
Ficat and Arlet | Association Research Circulation Osseous (ARCO) | Japanese Orthopaedic Association | |||
|---|---|---|---|---|---|
Stage | Findings | Stage | Findings | Stage | Findings |
I | Normal X-ray | 0 | Normal hip | 1 | Demarcation line |
II | Diffuse cystic/sclerotic lesions | 1 | MRI findings only | 2 | Early femoral head flattening |
III | Crescent sign (subchondral fracture) | 2 | Focal osteoporosis, cystic lesions, sclerosis | 3 | Cystic lesions |
IV | Femoral head collapse, acetabular involvement | 3 | Crescent sign (subchondral fracture) | ||
4 | Acetabular involvement | ||||
The goal of management is early diagnosis in the precollapse stage and to prevent progression to collapse. Although various pharmacological and biophysical treatment strategies have been suggested for the prevention and treatment of disease progression, the management of osteonecrosis continues to be challenging [2]. Additionally, bone-preserving procedures such as bone grafting, osteotomies, and core decompression have been proposed to avoid the need for total joint arthroplasty.
Core decompression has been used commonly for the treatment of smaller-sized precollapse lesions [10–12]. This technique was initially developed by Ficat and Arlet [13]. The procedure was postulated to be effective because it was believed that the pathogenetic mechanism of osteonecrosis was an elevated intraosseous pressure causing extravascular compression of the blood vessels within the femoral head. It was therefore postulated that early treatment with decompression would relieve intraosseous pressure of the femoral head, thereby restoring normal vascular flow [14]. The general pathophysiology of osteonecrosis of the hip is proposed to be disruption of the microcirculation to the femoral head. The additional mechanisms leading to vascular disruption are postulated to be due to direct vascular interruption from trauma or from intravascular occlusion by thromboembolic events or fat emboli [15–17]. The following sections address preoperative planning, indications, surgical techniques, rehabilitation, and the outcomes reported in literature for core decompression.
38.2 Preoperative Planning and Indications for Core Decompression
Formulating a treatment plan should be based on clinical factors. Patients generally present with groin pain, trochanteric symptoms, or nonspecific hip pain. The treatment plan should be tailored to the patients’ age, the presence of medical comorbidities, and the activity level.
Radiographic factors should also be taken into consideration, as core decompression is generally recommended for patients without advanced arthritis or subchondral collapse. Early stage (Ficat and Arlet Stage I and II), smaller-sized lesions with a combined necrotic angle of less than 200° have been demonstrated to have more favorable results with this procedure [18–20]. Since the disease is often bilateral, a thorough evaluation for contralateral joint involvement should be conducted as well [14, 21–23] (Fig. 38.1).
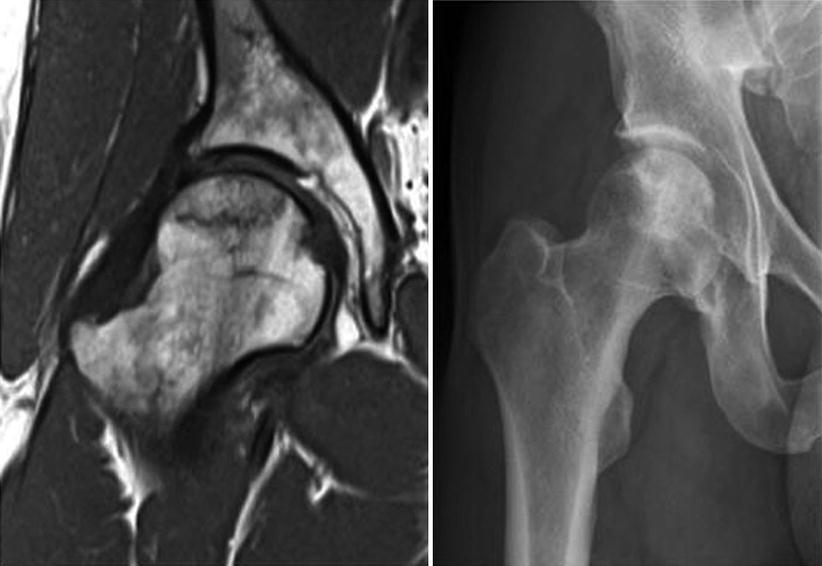
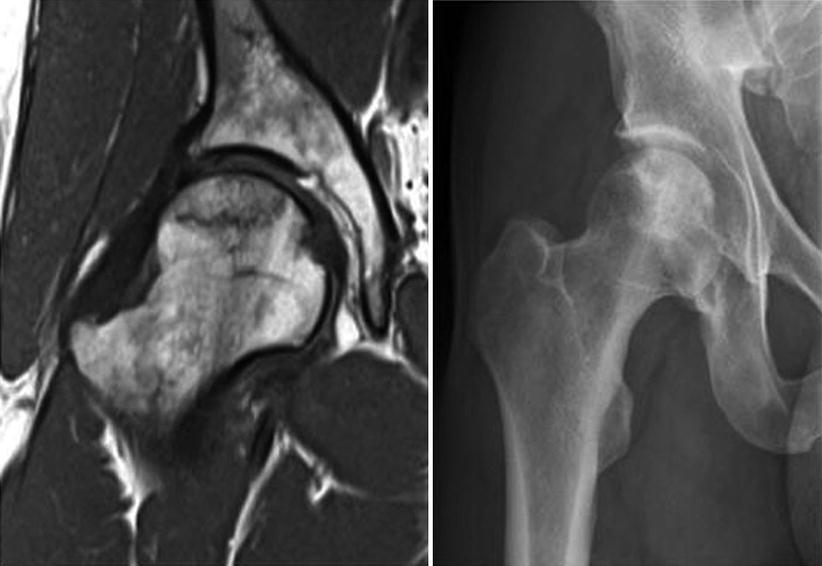
Fig. 38.1
MRI and X-ray features of osteonecrosis
38.3 Surgical Technique (Authors’ Experience)
Currently, all of these procedures are performed using fluoroscopic guidance. The conventional core decompression involves one to three large diameter drilling. The area of the lesion should be identified on radiographs or magnetic resonance imaging (MRI) scans to identify stage 1 Ficat and Arlet disease. The position of the femoral head should be identified prior to preparing and draping the hip. The initial tract made for the core decompression should be above the superior level of the lesser trochanter, which minimizes the risk of developing a stress fracture of the femur. With the guide wire in place, an 8–10-mm wide cannulated trephine is generally used (Fig. 38.2). Subsequently, the necrotic bone is removed with a burr (Fig. 38.3). The Steinberg modification to the traditional core decompression involves the removal of three bone cores from the single initial hole made for the procedure. Through a lateral approach a trephine is used to remove an 8-mm core of bone from the center of the lesion. Subsequently, two 6-mm bone cores are removed from the lesion’s periphery through the same entry site. Then, viable bone is grafted into the central core region of the femur.
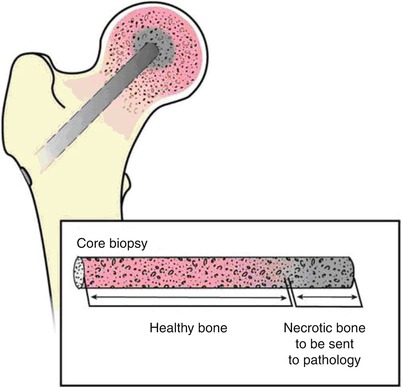
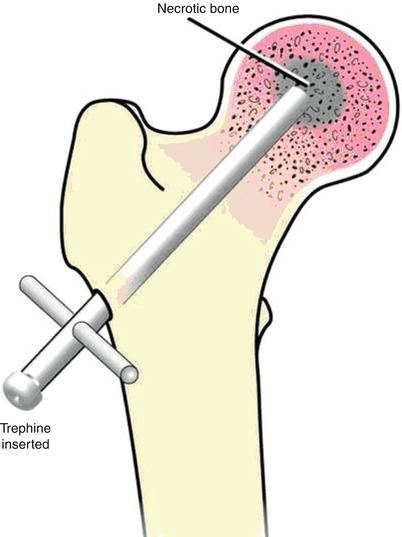
Fig. 38.2
Core decompression
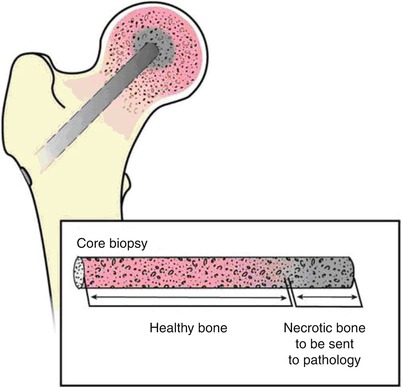
Fig. 38.3
Eight to ten millimeter of tissue removed after core
An alternative to the conventional core decompression is multiple drilling , which consists of small diameter core tracts. Under fluoroscopic guidance the pin is slowly advanced until it comes in contact with the lateral cortex above the lesser trochanter and is subsequently passed through the femoral neck and into the femoral head to the site of the lesion.
38.4 Rehabilitation
Protective 50 % weight-bearing is recommended for 4–6 weeks postoperatively with the use of a cane or other ambulatory aids. After this period, the patient can be advanced to full weight-bearing without the use of aids as tolerated. Standard rehabilitation should include hip abductor strengthening and range of motion exercises. Patients are discouraged from engaging in high-impact activities for a minimum of 10–12 months postoperatively. However, if after this time there is no radiographic evidence of collapse, the patients are allowed to resume all prior activities.
38.5 Outcomes of Core Decompression
38.5.1 Core Decompression
In 1985 Ficat et al. reported favorable outcomes in 133 patients who were treated with core decompression for early stage lesions. The survivorship was 94 % for patients who had stage I disease and 82 % for patients who had stage II disease [24]. Fairbank et al. reported similar outcomes in 128 hips (90 patients) undergoing core decompression for Ficat and Arlet stage I, II, and III disease. At a mean follow-up of 11 years, the survivorship was reported to be 88 % for stage I, 72 % for stage II, and 26 % for stage III disease [25]. A study by Steinberg et al. reviewed the outcomes of core decompression with bone grafting in 406 hips for osteonecrosis of the femoral head. At a mean follow-up of 29 months, 18 of 65 hips (28 %) with stage I disease, 45 of 133 hips (34 %) with stage II disease, 3 of 13 hips (23 %) with stage III disease, and 45 of 92 hips (49 %) with stage IV disease required a hip replacement [26]. However, a study by Markel et al. reported poorer outcomes in 53 hips with the use of core decompression. At a mean follow-up of 4 years, the survivorship was reported to be 45 % for stage I, 38 % for stage IIa, 14 % for stage IIb, and 25 % for stage III disease [22]. See Table 38.3 for a summary of results.
Table 38.3
Outcomes of core decompression
Author (year) | Level of evidence | Hips | Mean age (years) | Follow-up (years) | Survivorship (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Stage 1 | Stage 2a | Stage 2b | Stage 3 | Stage 1 | Stage 2a | Stage 2b | Stage 3 | ||||
Al Omran (2013) [23] | III | 13 | 25 | 23 | – | 26 | 6.1 | 100 | 80 | 52 | – |
Lieberman et al. (2004) [27] | IV | – | 15 | 1 | 1 | 47 | 4.4 | – | 93 | 0 | 0 |
Aigner et al. (2002) [28] | IV | 30 | 9 | – | 6 | 41 | 5.7 | 97 | 44 | – | 33 |
Steinberg et al. (2001)a [26] | III | 65 | 45b | – | 13 | 37 | 48 | 72 | 66b | – | 77 |
Lavernia and Sierra (2000) [29] | IV | 15 | 30b | – | 22 | 40.2 | 3.4 | 100 | 83b | – | 44 |
Maniwa et al. (2000) [30]
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||||||||||