Nuclide
Radiation type
T1/2
Eβ.max
p
Eγ
p
Dose rate [mSv/h GBq]
[keV]
[%]
[keV]
[%]
in 30 cm from point sourcea
in contact with 5 ml syringe
P-32
β-
14.3 d
1710
100
–
–
120
–
23900
Sr-89
β-
5.05 d
1495
100
–
–
120
–
16400
Y-90
β-
2.67 d
2284
100
–
–
108
–
43500
J-131
β-/γ
8.04 d
606/334
90/7
365/637
82/7
86
(0.73)
1130
Sm-153
β-/γ
1.95 d
703/634
44/35
41/103
49/28
103
(0.19)
241
Ho-166
β-/γ
1.12 d
1857/1776
51/48
81
6
≈130 b
(0.32)
?
Er-169
β-
9.40 d
352/344
58/42
–
–
9.2
–
≪
Lu-177
β-/γ
6.71 d
497/176
79/12
208/113
11/6
≈ 90 b
(0.15)
?
Re-186
β-/γ
3.78 d
1077/939
72/22
137/59
9/3
120
(0.04)
380
Re-188
β-/γ
16.9 h
2118/1962
72/25
155/633
15/1
110
(0.11)
28800
Tc-99m
γ
6.01 h
–
–
141
89
–
(0.26)
354
There are several reasons for the fact that the use of unsealed radiation sources for therapy is a matter of concern regarding radiation exposure to staff:
the high activities of some 10 MBq up to some GBq per patient that are needed to obtain the therapeutic effect,
the use of beta emitters having a considerably higher dose factor (dose rate per activity unit) than gamma radionuclides,
the fact that some practices require handling of radionuclides close to the skin on the hands and
the additional risk of contamination when handling unsealed nuclides.
The second feature is underlined with the parameters given in Table 1, summarising physical and radiological data of the most important radionuclides. For comparative purposes, the characteristics of Tc-99m were also included. When comparing, for instance, the dose factors for the most widespread nuclides in nuclear medical diagnostics and therapy, Tc-99m or Y-90, it becomes obvious that the dose due to the high-energy betas from Y-90 is more than two orders of magnitude higher than that from a Tc-99m source of the same activity. It should be emphasised that this feature also applies to positron (β+) emitting nuclides, especially to those with high particle energy. These nuclides, such as Ga-68 (Eβ,max = 1.9 MeV) and F-18 (Eβ,max = 0.6 MeV), are relevant to radiation protection as well, but are not focussed in this article since they are used in PET imaging.
Consequently, in situations where the radiation protection standard is low, the medical staff in nuclear medical therapy facilities may receive high exposures, mainly to the skin on the hands that can exceed the annual dose limit of 500 mSv. Therefore, appropriate safety standards are to be strictly kept. Moreover, some advice is needed to particular groups of the public, i.e. family members of therapy patients and nursing staff who are not classified as radiation workers.
2 Occupational Exposure of Medical Staff
2.1 General Radiation Protection Principles
Radiation protection is founded on three basic principles: justification, limitation and optimisation. These principles are defined and elucidated in numerous international recommendations (IAEA 1996; ICRP 1997) and national regulations. Namely, the International Commission on Radiological Protection (ICRP) has addressed the nuclear medical community with several publications focussed on radiation protection of staff and patients in medicine and nuclear medicine (ICRP 1996, 1998, 2000, 2004, 2007). Also, the International Atomic Energy Association (IAEA) has issued some comprehensive publications on this topic (IAEA 2005, 2006, 2009).
In the context of this article, the justification i.e. the medical indication of the radionuclide therapy procedure is taken for granted and not to be further discussed.
The central part of the limitation principle of radiation exposures is the definition of dose limits. The most important annual dose limits for radiation workers recommended by ICRP (1997) and implemented in most countries are listed in Table 2. The effective dose limit of 20 mSv per year is an average over defined periods of 5 years, whereas the dose should not exceed 50 mSv in any single year. Moreover, the limit applies to the sum of external exposure and the dose committed in 50 years from incorporation of nuclides.
Table 2
Selected annual dose limits of occupationally exposed persons
Effective dose | 20 mSv |
|---|---|
Equivalent dose to the: eye lens skin hands and feet | 150 mSva 500 mSv 500 mSv |
To assure that a worker does not receive or exceed the dose limits, all procedures that may cause exposures of staff have to be optimised related to radiation protection. The most common rule of optimisation in radiation protection is the ALARA principle. The phrase refers to the principle of keeping radiation doses ‘As Low as Reasonably Achievable’, whereas economic aspects, i.e. the costs of protection measures, should be taken into account. Of course, this principle has also to be applied for nuclear medicine.
It is an important pre-condition for an optimised radiation protection regime in nuclear medicine that all personnel involved in the procedures must have appropriate training in the safe handling of the radiation sources. This is of special importance when procedures for preparing or administering radiopharmaceuticals are more sophisticated and more hazardous than usual, as is the case when labelling antibodies or peptides for radioimmunotherapy (RIT) or radiopeptide therapy (PRRT). Such practices and working steps should be exercised without the radionuclide to minimise external exposure by reducing the exposure time. However, even experienced medical and technical staff is often unaware of the enhanced risk of exposure, when operating with beta emitters in comparison to common gamma sources at the same activity level.
2.2 Radiation Protection Measures
2.2.1 Shielding
Shielding is a very effective precautionary measure and it should go without saying that appropriate shielding, e.g. for vials and syringes, is used in the daily nuclear medicine and radiopharmacy practice. Materials with high atomic number Z, i.e. with high density, such as lead or tungsten are most common to protect against gamma radiation. Syringe shields usually have an additional lead glass window. These shields are also sufficient for most of the mixed beta-/gamma emitters which have beta emission with low or moderate energy like I-131, Sm-153 and Lu-177. When selecting the shielding material and thickness that is necessary for a particular radionuclide, the gamma emission with the highest energy and its abundance must be considered first of all.
For high-energy beta-emitting radionuclides such as Y-90 and Re-188, shields from low-Z materials, usually transparent plastic such as acrylic glass or polycarbonate are preferred in order to minimise secondary bremsstrahlung. A set of such shields as used in RIT with Y-90/Zevalin® is shown in Fig. 1. Sometimes, plastic shields are combined with an outer lead layer to additionally degrade the bremsstrahlung. These sandwich shields are also useful for nuclides having a non-negligible gamma emission. The contribution of bremsstrahlung to the exposure is often overestimated. Effective shielding of the betas has absolute priority. The required shielding material and its thickness depend on the type and activity of the nuclide. Beta particles are completely absorbed if the thickness exceeds the maximum range. For Y-90 (Eβ,max = 2.3 MeV), the beta emitter with the highest energy used in nuclear medicine, the range in plastic is about 9 mm. In other words, 9 mm is the maximum thickness of any plastic shielding material that is needed to cope with the betas of all radiopharmaceuticals used in nuclear medicine. If low-Z shieldings are not on hand when handling high-energy beta emitters, it is better to use suitable high-Z shields than nothing. The range of the beta particles is much smaller, e.g. 1 mm in lead for betas from Y-90. Thus, a common lead or tungsten shield which is a few millimetres thick will absorb all betas and will additionally provide an effective attenuation of the enhanced bremsstrahlung.


Fig. 1
Acrylic shields for vials and syringes for Y-90/Zevalin® therapy
There are several shields for vials, syringes and containers available that were specially designed for therapeutic radiopharmaceuticals, mainly for those containing beta emitters. Besides, even common shielding equipment that is used in diagnostic nuclear medicine can and should also be utilised for therapy procedures. The exposure of staff during preparation and dispensing can be reduced significantly, when working behind conventional bench-top shields such as lead walls or castles or lead glass windows. Some manufacturers provide special acrylic bench-top shields to protect against beta radiation. For the administration of radiopharmaceuticals to patients, moveable and preferably transparent shields are useful. As an example, a working area that is used for labelling radiopharmaceuticals with Y-90 is shown in Fig. 2, consisting of a fume hood and a moveable acrylic shield with a lead reinforcement.
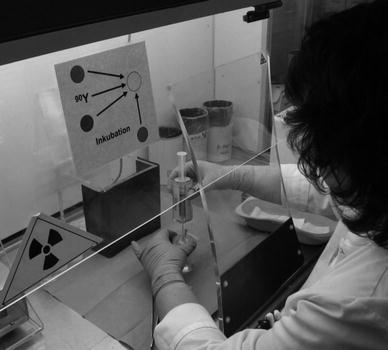
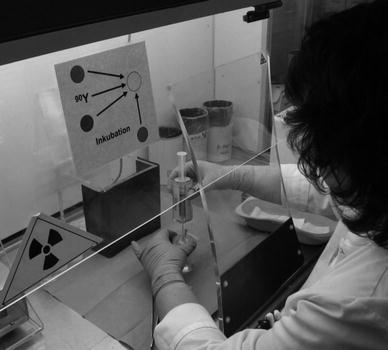
Fig. 2
Adequately shielded workplace for Y-90 labelling
Of course, shields often hamper handling, such as when injecting a radiopharmaceutical into the patient. It is a mistake to believe, however, that omitting the shielding can be compensated by working faster.
Use of suitable shielding is not a guarantee but a prerequisite for low radiation exposures. For example, even when applying a syringe shield there is still an unshielded area of high dose rates at its base. Therefore, needles or tubes should be connected and disconnected using tools rather than the fingers. How this can be done in a safe way is demonstrated in Fig. 3.









