Psychiatric Disorders
Perry F. Renshaw
Jieun E. Kim
In Kyoon Lyoo
General Explanation on Magnetic Resonance Techniques
The advancement of neuroimaging technology has left its mark on psychiatry research by noninvasively assessing the brain anatomy, function, and chemistry in human. In psychiatry, neuroimaging has been used clinically to illustrate the underlying pathology of psychiatric disorders, and thus to aid in their accurate diagnosis (1). Therefore, it is essential to connect clinical pathology with anatomic and functional findings brought by neuroimaging (2). In the future, neuroimaging techniques may be potentially used not only to confirm diagnosis but also to predict the vulnerability, progress, and treatment response of psychiatric disorders. This predictive aspect of neuroimaging will be cost-effective by targeting those who are at risk in advance and providing preventive interventions, or treatment to them. Moreover, monitoring the treatment response through neuroimaging will ensure any possible side effect present before clinical symptoms occur. In this chapter, we review the use of magnetic resonance imaging (MRI) in psychiatric disorders in the three domains of structural neuroimaging (i.e., structural and diffusion MRI), functional neuroimaging (i.e., functional MRI [fMRI]), and metabolic imaging of underlying neurochemistry (i.e., magnetic resonance spectroscopy, or MRS).
Psychotic Disorder—Schizophrenia
Schizophrenia is perhaps the most severe psychiatric disorder which begins in late adolescence or early adulthood, affecting 1% of the population with no significant difference between men and women (3). The illness is lifelong with significant morbidity and disability (4). The main positive symptoms include delusions, hallucinations, disorganized speech, and behaviors that cause social dysfunction, and negative symptoms include significant impairment of normal psychological functions (5). Cognitive symptoms such as impairments in executive function and working memory (6) are also included. Schizophrenia is comorbid with major depression disorders (MDDs), anxiety disorders, and substance use disorders (7).
Structural Neuroimaging
Using structural MRI, several studies have shown both gray matter (GM) and white matter (WM) abnormalities in individuals with schizophrenia compared to healthy controls. Most consistently, individuals with both first-episode schizophrenia (FES) and chronic schizophrenia (CS) have shown GM atrophy in the frontal lobes, hippocampus, and temporal lobes (8,9,10). Some studies using region of interest have indicated specific brain regions directly related to schizophrenia symptoms (11,12). Specifically, reduced anterior cingulate volumes observed in individuals with schizophrenia were associated with problems regulating emotional stimuli and disorganizing higher cognitive functions as this area has extensive connections with other areas involved in emotional processing (11). Altered superior temporal gyrus (STG) volume, which is connected to temporal limbic brain regions and involved in self-monitoring and language interpretation, additionally illustrates auditory hallucinations and thought disorders in individuals with schizophrenia (12). Other studies using voxel-based morphometry (VBM) have demonstrated whole-brain analysis of GM reduction related to schizophrenia (13). Diminished GM in the bilateral insula, inferior frontal cortex (IFC), STG, anterior cingulate gyrus, medial frontal cortex (MFC), thalamus, and left amygdala was observed, contributing to negative symptoms and cognitive deficits of schizophrenia (13).
Not only GM volumes but also reduced WM volume in the frontal lobe and bilateral internal capsule were also shown in individuals with schizophrenia (14). In addition, changes in WM continuously have affected the frontal, temporal, and parietal lobe in CS individuals (15). Additionally, studies on structural WM integrity in schizophrenia have supported the deficits of WM in the course of schizophrenia, beginning in the prodromal stage (16). Lower FA was observed throughout the brain including subcortical regions in the individuals with schizophrenia as compared to the healthy controls. Decreased FA values were observed in the left fronto-occipital fasciculus (FOF) and the left inferior longitudinal fasciculus (ILF), in which connectivity was also positively associated with cortical thickness in the left lateral orbitofrontal cortex (OFC), STG, and lingual gyrus of male brain and with GM volume in the left OFC of female brain (17,18). Splenium, not genu, of corpus callosum (CC) also had lower FA in the individuals with schizophrenia indicating disconnection and abnormalities in fiber coherence, myelination, and even membrane density (17,19). FA values, also related with positive symptoms, had positive correlation with WM in the right frontal lobe and left STG (20). DTI studies, therefore, showed widespread and extensive structural disconnections associated with schizophrenia.
Functional Neuroimaging
Working Memory
As a part of neurocognitive deficits in schizophrenia, working memory is severely impaired in both CS and FES individuals (21). In CS, widespread network including the anterior
cingulate cortex (ACC), prefrontal, temporal, and parietal areas is affected. The ACC, left prefrontal cortex (PFC), left inferior parietal cortex (IPC), superior and medial frontal cortex, parahippocampal cortex, and temporal areas differed compared to healthy controls (22,23) during the item recognition task. Reduced functional connectivity of the left sylvian–parietal–temporal area and the left anterior insula during auditory working memory was also observed, explaining the core schizophrenic symptoms (24). In the FES, abnormal neural activations in the insula, precuneus, and bilateral PFC were shown during n-back tasks (25). Lower activity in the middle frontal gyrus (MFG) and greater activation in the bilateral inferior frontal gyrus (IFG) during verbal working memory tasks (26), showing behavioral deficits in working memory from the very early stage of disorder.
cingulate cortex (ACC), prefrontal, temporal, and parietal areas is affected. The ACC, left prefrontal cortex (PFC), left inferior parietal cortex (IPC), superior and medial frontal cortex, parahippocampal cortex, and temporal areas differed compared to healthy controls (22,23) during the item recognition task. Reduced functional connectivity of the left sylvian–parietal–temporal area and the left anterior insula during auditory working memory was also observed, explaining the core schizophrenic symptoms (24). In the FES, abnormal neural activations in the insula, precuneus, and bilateral PFC were shown during n-back tasks (25). Lower activity in the middle frontal gyrus (MFG) and greater activation in the bilateral inferior frontal gyrus (IFG) during verbal working memory tasks (26), showing behavioral deficits in working memory from the very early stage of disorder.
Executive Function
Executive functions including impairments in cognition, problem solving, and task switching are most widely observed in both CS and FES individuals (27). Hypoactivations in the anterior cingulate and prefrontal areas were shown during the discrimination of novel or old visual stimuli tasks in both CS and FES compared to healthy controls (28). During the “Tower of London” task which requires planning, individuals with FES exhibited altered right prefrontal and temporal activation pattern even though there were no deficits in the actual performance (29).
Social Cognition
Social cognition, directly related to the general social outcome, may be associated with the social brain network, causing impairments in individuals with schizophrenia (30). In individuals with CS, fusiform gyrus, which is related to the face recognition, and parahippocampal gyrus, which retrieves and encodes memory, were hyperactivated during the process of neutral faces compared to healthy controls (31). Hyperactivation of the MFG, superior frontal gyrus (SFG), and precuneus were shown with reduced connectivity between the amygdala and the insula during approachability judgments in individuals with schizophrenia compared to healthy controls. Increased activity in the frontal brain regions may indicate compensation for impaired social brain connectivity with the amygdala, which was normally shown in healthy controls (30).
Neurochemistry
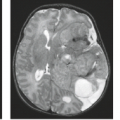
Various MRS studies have investigated the alterations of various neurometabolites including NAA, Cr, Cho, Glu, and myo-inositol (mI) and their ratio in individuals with schizophrenia (Table 29.1) (Fig. 29.1) (32). Decreased NAA levels in the hippocampus, frontal, temporal lobe, and thalamus were shown in individuals with schizophrenia compared to controls, indicating executive dysfunctions (33,34). Reduced NAA level in the thalamus was noted not in individuals with FES but also in individuals with CS, implying the effect of NAA on persisting schizophrenic symptoms to be a chronic psychiatric disorder (33).
Lower Glu levels, higher Gln levels, and increased Gln/Glu ratio were observed in the frontal brain region (49). These levels were associated with the individuals’ age, supporting progressive loss of synaptic activity with aging. Increased levels of glutamatergic indices in the medial PFC and basal ganglia, which might have association with elevated Glx in hippocampus, were also examined (50).
Neurodevelopmental Disorders
Autism Spectrum Disorders
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by significant impairments in social interactions, both verbal and nonverbal communication, and behaviors from the early childhood (5). ASD, affecting approximately 1% of the general population, includes autism, Asperger syndrome, pervasive developmental disorder not otherwise specified (PDD-NOS), childhood disintegrative disorder, and Rett syndrome. The Centers for Disease Control and Prevention (CDC)’s Autism and Developmental Disabilities Monitoring (ADDM) Network (2014) identified that approximately 1.5% of children in the United States are to be diagnosed with ASD, more commonly in boys than in girls. Prevalence of ASD, however, would likely be lower after future adaptation and documentation of the Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) in the clinical settings (51). ASD might be associated with epilepsy, obsessive–compulsive disorder (OCD), attention-deficit/hyperactivity disorder (ADHD), and anxiety disorders (52,53).
Structural Neuroimaging
Unfortunately, the findings of various structural MRI studies on ASD have shown inconsistent results—both enlargement and reduction in various brain areas associated with higher cognitive functions including the frontal lobe, temporal lobe, limbic system, and CC (Table 29.2) (54). In ASD children, different structural changes have taken place depending on each developmental stage; from birth through 2 years of age, enlarged cerebral volume accelerated brain overgrowth (55). Then during adolescence, their brain growth gets abnormal and reaches a plateau within the normal range by adulthood (56,57). Increased GM volume and decreased GM density in the frontal and temporal lobes were shown in ASD individuals, indicating abnormalities in social cognition, executive functions, and languages (58). Increased frontal lobe volumes including the dorsolateral prefrontal cortex (DLPFC) and medial prefrontal cortex (MPFC) were also found related to these functional impairments (59).
Contrary to the overall increase in cerebral volume, smaller average size of CC was observed in 3 to 4 years of age children with ASD (76). Also, reduced total area and regions of the CC were shown in the individuals with ASD indicating disorder-related differences in the inter-hemispheric connections (77). In addition, increased amygdala volume and faster amygdala growth have been observed in children with ASD less than 10 years of age, which might be associated with deficits in emotional and social behaviors including joint attention, gaze avoidance, and eye fixation (78,79). In adolescence and adults with ASD, similar or smaller amygdala volumes have been reported compared to healthy controls (80).
DTI studies on altered brain connectivity have pointed out broad WM impairments in individuals with ASD. The uncinate fasciculus (UF) has been suggested to be associated with impaired social–emotional processing and functions in ASD (81,82). Kumar et al. (83) reported lower FA in the right UF, right arcuate fasciculus (AF), right cingulum, and CC in children with ASD. Poutska et al. (35) showed decreased FA in the bilateral UF, CC, and the right superior longitudinal fasciculus (SLF). Abnormal WM microstructure of frontotemporal cortical networks in ASD, therefore, is related with core symptoms of the disorder as there also has been an association between these regions and social symptoms in ASD (81). Abnormal macro- and microstructural properties of the CC were also related to socio-communicative deficits in children with ASD (36). Longer average fiber length (AFL) and AFL difference of the forceps major were observed (83). The strong correlation between communication functions and the FA of the forceps major were also shown in the individuals with ASD (36).
Functional Neuroimaging
Social Cognition
Face perception and theory of mind are distinct social impairments shown in individuals with ASD with most abnormalities
in the amygdala and fusiform face area (FFA) activation (37). Attenuated FFA–amygdala connectivity and strengthened amygdala–right IFG connectivity indicate greater social impairments in individuals with ASD during neutral face processing tasks, suggesting the involvements of the limbic system in the social deficits (38). During emotional face tasks, reduced FFA and amygdala activation was also observed, and these activation was positively associated with time spent fixating the eyes on the face in the children with ASD (39,40).
in the amygdala and fusiform face area (FFA) activation (37). Attenuated FFA–amygdala connectivity and strengthened amygdala–right IFG connectivity indicate greater social impairments in individuals with ASD during neutral face processing tasks, suggesting the involvements of the limbic system in the social deficits (38). During emotional face tasks, reduced FFA and amygdala activation was also observed, and these activation was positively associated with time spent fixating the eyes on the face in the children with ASD (39,40).
TABLE 29.1 Magnetic Resonance Spectroscopy Findings in Individuals with Schizophrenia | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 29.2 Structural Magnetic Resonance Imaging Findings in Individuals with Autism Spectrum Disorder | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Deficits in the theory of mind, which is important for understanding others and other social cognition skills, may be associated with mirror neuron system (MNS). Children with ASD showed no MNS activity when they imitate and observe emotional facial expressions of others (41).
Language and Communication
Language and communication impairments are common in individuals with ASD, especially in young children. Abnormal right-lateralized temporal cortex activities to language and reduced left hemisphere responses to speech sounds were observed in both children with ASD and children at risk for ASD under 4 years of age (42,43). In various language-related tasks including sentence comprehension, semantic judgments, verbal fluency, and language comprehension, children with ASD had decreased function in brain regions processing language and activated function in brain regions that are not typically related to language processing (44).
Individuals with ASD depend on visualization for language processing, using different regions of the brain compared to healthy controls. Occipitoparietal and ventral temporal regions got activated in individuals with high-functioning autism, whereas frontal and temporal language regions got activated in controls during a pictorial reasoning paradigm (45). Parietal and occipital lobes were associated with imagery in comprehending imagery sentencing (46), and bilateral extrastriate visual cortex was related to visual imagery in semantic processing (47). These findings suggest that individuals with ASD rely more on visualization to support language comprehension than in healthy controls.
Executive Function
Deficits in executive functions, including inhibition and planning, may lead to behavioral control problems and repetitive symptoms frequently observed in individuals with ASD (48). Increased activation of the putamen and decreased activation of inferior parietal lobe (IPL) on the anti-saccade task, a measurement of inhibitory control, was shown in adolescents and adults with ASD (84), showing developmental differences of inhibitory control system related to the brain circuit. Reduced ACC reactivity during response inhibition tasks and weakened functional connectivity between inhibition network including ACC and the right middle and inferior frontal and right parietal regions were observed in adults with ASD compared to healthy controls, indicating atypical and less synchronized inhibition circuitry (85).
Reduced connectivity between frontal and parietal areas were observed during the “Tower of London” task in adults with ASD, indicating possible association between abnormalities in integration of information and problems in executive functions (86).
Neurochemistry
MRS studies of ASD have generally measured metabolites including NAA, Cr, and Glx in various brain regions (87,88). Decreased NAA levels in the parietal regions and cerebellum were observed in individuals with ASD and in ACC for both adults and children with ASD, with lower values in adults than in children, indicating the age effects of metabolite levels and the regions (87). Decreased level of NAA indicates abnormalities in neurogenesis and in neuronal metabolites, bringing up the major symptoms of the disease (89). Both increase and decrease levels of Cr depending on the age and the brain
regions were shown. Cr concentrations were more detected in the temporal lobes in adults, but were less detected in the occipital lobes in children with ASD (87). As Cr plays an important role in energy storage in the brain, abnormalities in Cr may lead to language problems or mental retardation (90).
regions were shown. Cr concentrations were more detected in the temporal lobes in adults, but were less detected in the occipital lobes in children with ASD (87). As Cr plays an important role in energy storage in the brain, abnormalities in Cr may lead to language problems or mental retardation (90).
Decreased Glx levels in the basal ganglia were also observed in adults with ASD, which were also correlated with increased deficits in social communication, indicating an association between Glx transmission and social development (88). NAA and Cr levels were also reduced in this region in addition to in DLPFC (88).
Attention-Deficit/Hyperactivity Disorder
ADHD is one of the most common neurodevelopmental disorders, which affects 5% of children worldwide and 11% of children 4 to 17 years of age in the United States (5,91). The percentage of children diagnosed with ADHD continues to increase, which reflects the increasing awareness of the disorder (60,91). It is more commonly diagnosed in boys than in girls, and a significant number of children diagnosed with ADHD continue to experience the disorder as adults (61). The main symptoms include inattention, having difficulty organizing tasks or failing to pay close attention in details, or hyperactivity and impulsivity, talking excessively or having difficulty remaining steadily in appropriate situations (5). These characteristics of the disorder lead to various degrees of functional impairment in individuals, which may be associated with oppositional defiant disorder, learning disabilities, conduct disorder, depression, mood disorders, anxiety disorders, and substance use disorders (62,63).
Structural Neuroimaging
Studies using VBM aim to identify neuroanatomical correlates of ADHD. Several MRI findings have reported structural abnormalities in different areas of the brain in children and adults with ADHD. The most consistently reported abnormalities in individuals with ADHD include reduced volumes of the frontal lobes, basal ganglia, and cerebellum (64). Specifically in children with ADHD, studies have shown volume and GM reduction in the right globus pallidus, putamen, and bilateral caudate, implying less control of subconscious voluntary movements (65,66). GM deficits in the right-sided frontoparietal brain circuits and left DLPFC were also detected in children with ADHD, implying poor performance in executive function tasks, attention, and behavioral inhibition (67,68). Children with ADHD also have delay in cortical maturation, reaching peak of their brain development around 10 to 11 years of age, compared to typically developing children, reaching around 7 to 8 years of age (69). This may be linked to smaller total brain volumes in children with ADHD (67).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree