Fig. 8.1
Pulmonary tuberculosis. The lung tissues were demonstrated with observable tubercles, containing caseous necrosis. Necrosis was shown to be surrounded by epithelioid cells, inflammatory exudates, and lung tissue. H&E staining
Fig. 8.2
Epithelioid cells and Langerhans giant cells in tubercle, H&E staining
Fig. 8.3
Acid-fast bacilli. The bacilli were shown as red short rods, Acid-fast staining
3.
Necrosis-based lesion
In cases with large amount of infected bacteria, strong virulence, and compromised immunity or strong allergic reactions, the abovementioned exudate- or hyperplasia-based lesion may develop into caseous necrosis. Microscopy demonstrates unstructured and red-stained particles, which are of certain significance for the diagnosis of TB. In most cases, caseous necrotic tissues contain a certain amount of M. tuberculosis, constituting the source of bacterial dissemination in the body. The caseous necrosis can also be dissolved and spread, leading to deterioration and progression of TB.
The above three types of lesions commonly coexist or with one type as the main lesion. Under certain conditions, the three types of lesions are interchangeable.
8.4.2 Pathological Features of Tuberculosis
Tuberculosis is a chronic granulomatous disease caused by M. tuberculosis. It can affect all body organs, but pulmonary tuberculosis is the most common. Due to different responses in the human body between primary infection and reinfection of M. tuberculosis cause, the pulmonary lesions are different. And pulmonary TB can be categorized into primary and secondary pulmonary TB.
8.4.2.1 Primary Pulmonary Tuberculosis
Primary tuberculosis is characterized by the occurrence of primary complex. After M. tuberculosis is inhaled into the lungs, grayish white inflammatory solid lesion about 1 cm in diameter firstly forms in the vicinity of the pleura of the lower part of the upper lung lobe or the upper part of the lower lung lobe with good ventilation. Caseous necrosis can be found at the center of most primary lesions, surrounded by exudates, which is more common in the right lung. The bacteria then rapidly invade lymphatic vessels to be disseminated to the hilar lymph nodes along with lymph flow. Consequently, tuberculous lymphangitis and lymphadenitis occur, manifested as enlarged hilar lymph nodes and caseous necrosis. Primary lung lesions, tuberculous lymphangitis, and hilar lymph node tuberculosis are collectively known as the primary complex, which is the most common in pediatric cases of pulmonary TB. Under the condition of malnutrition or compromised immunity, the lesions expand, with caseous necrosis and cavity. In some cases, the lesions even disseminate in the lungs to cause miliary TB. Otherwise, the lesions may even disseminate in the whole body to cause systemic miliary TB.
8.4.2.2 Secondary Pulmonary Tuberculosis
Secondary pulmonary tuberculosis is caused by reactivated M. tuberculosis after primary infection. It is rarely exogenous reinfection. Various morphologies of TB lesions coexist in patients with secondary pulmonary tuberculosis. According to pathological feature and clinical course, the lesions of secondary pulmonary TB can be classified into the following five types:
1.
Focal tuberculosis
The lesion is about 0.2–1.0 cm in diameter, which is hyperplasia based with a small quantity of central caseous necrosis.
2.
Infiltrative tuberculosis
Infiltrative lesions are mostly developed from focal lesions. The common early lesions are demonstrated with mixed pathological changes of different degrees of inflammatory infiltration and fibrous nodules. The lesion is exudate based, with central caseous necrosis that is surrounded by inflammatory tissue.
3.
Chronic fibrocavitary tuberculosis
Chronic fibrotic cavity type is pathologically characterized by singular or multiple chronic cavities with relatively thick fibrous capsules in the lungs. The cavities are surrounded by significant fiber changes and scattered new and old lesions. The cavity wall can be divided into three layers. The inner layer is caseous necrosis, containing a large quantity of M. tuberculosis. The middle layer is tuberculous granulation tissue, and the outer layer is fibrous connective tissue.
4.
Caseous pneumonia
The caseous lesion-based infiltrative TB is known as caseous pneumonia. Microscopy mainly demonstrates large flakes of caseous necrosis. The alveolar cavity is demonstrated with serous fluid and fibrinous exudates with macrophage-based inflammatory cells.
5.
Tuberculoma
When large flake of caseous necrosis is surrounded by fibrous tissue or blocked by cavity, it is subjected to shrinkage. Those with a diameter of less than 2 cm are fibrous caseous lesions, and those with a diameter of above 2 cm are known as tuberculoma (Fig. 8.4).
Fig. 8.4
Tuberculoma. Large flake of caseous necrosis was shown to be surrounded by fibrous tissue, H&E staining
8.5 Classification of TB and Their Clinical Diagnosis
According to the new classifying criteria of tuberculosis implemented in China in 2004, tuberculosis can be classified as follows:
1.
Primary pulmonary tuberculosis including primary complex and intrathoracic lymphoid tuberculosis
Primary pulmonary TB is common in children and young adults. Clinical manifestations include irregular low-grade fever, anorexia, night sweats, and other tuberculosis poisoning symptoms. In some cases, the patients may experience acute onset and high fever. And some patients may show symptoms of cervical lymphadenectasis. Chest X-ray rarely displays typical dumbbell-like and bipolar shape signs. But CT is superior to chest X-ray in the diagnosis of pulmonary TB.
2.
Hematogenous disseminated pulmonary tuberculosis including acute, subacute, and chronic hematogenous disseminated pulmonary TB
M. tuberculosis spreads along with the blood flow to the lungs. The clinical manifestations include obvious tuberculosis poisoning symptoms such as chills, high fever, night sweats, and accompanying respiratory symptoms such as cough, expectoration, and shortness of breath. By physical examination, pulmonary rales are relatively less and hepatosplenomegaly is common. By chest X-ray, acute hematogenous disseminated pulmonary TB is displayed as typical miliary opacities, with even density, size, and distribution. Some patients can be detected with tubercles on the choroid of ocular fundus.
3.
Secondary pulmonary tuberculosis including infiltrative pulmonary tuberculosis, cavitary pulmonary tuberculosis, tuberculoma, caseous pneumonia, and fibrocavitary tuberculosis
The clinical manifestations of secondary pulmonary TB are diversified. The patients commonly experience no obvious symptoms at the early stage. Along with progress of the condition, the patients gradually show symptoms of fatigue, weariness, poor appetite, weight loss, low-grade fever, night sweats, and other tuberculosis poisoning symptoms as well as uncurable cough. In some cases, sudden hemoptysis is the first symptom, rarely with signs of pulmonary TB. The patients may experience low breath sounds or local rales and dullness to percussion. Chest X-ray demonstrates multiple patches, nodules, and cord-like opacities, cavity opacity, tuberculoma, and calcification in both lungs. Coexistence of old and new lesions is characteristically pulmonary TB, predominantly at the upper lung lobes. Based on positive result by sputum smear for acid-fast staining or Mycobacterium culture, the diagnosis can be defined.
4.
Tuberculous pleurisy including dry tuberculous pleurisy, exudative tuberculous pleurisy, and tuberculous empyema
Many patients experience pleural pain and sometimes accompanying fever, cough, fatigue, and anorexia. Shortness of breath after activities is associated with the quantity of pleural effusion. By physical examination, signs of pleural effusion can be found, and sometimes pleural fricatives can be heard at the early stage. Chest X-rays show typical signs of pleural effusion and accompanying radiological changes of pulmonary TB.
5.
Extrapulmonary tuberculosis including tracheobronchial tuberculosis, renal tuberculosis, tuberculous meningitis, and tuberculous pericarditis
Extrapulmonary TB can be classified into various types and thus is nonspecific. Extrapulmonary TB is commonly concurrent to intrapulmonary TB. Tuberculosis at different body parts has its own features whose definitive diagnosis should be based on bacteriologic and pathologic evidence.
8.6 Diagnostic Imaging
8.6.1 Radiological Demonstrations of Pulmonary Tuberculosis
8.6.1.1 Primary Pulmonary Tuberculosis
Primary Pulmonary Tuberculosis including primary complex and intrathoracic lymphoid tuberculosis
Primary Complex by Radiology
1.
Primary lesion
After invasion of M. tuberculosis into the lungs, acute exudative inflammation occurs in the bronchioles and alveoli. The lesion is commonly located at the lung margin of posterior segment of upper lung lobe and dorsal segment of lower lung lobe. The primary lesion is mostly singular in size of 0.5–2.0 cm. It may be spot-, nodule-, or patch-like in shape with poorly defined boundary. And its density is centrally high and peripherally low.
2.
Lymphangitis
The pathogenic bacteria in the primary lesion can be disseminated to the lung hilum along with lymph flow. During its course to the lung hilum, it can cause lymphangitis. Radiologically, cord-like and strip-like opacity is demonstrated between the primary lesion and the lung hilum, which is poorly defined.
3.
Hilar and mediastinal lymphadenectasis
Along with lymph flow, the pathogenic bacteria gain their access into the lung hilum and mediastinal lymph nodes to cause inflammation, with manifestation of enlarged lymph nodes at the hilum and mediastinum. Radiologically, pulmonary primary lesion, lymphangitis, hilar, and mediastinal lymphadenectasis are demonstrated, namely, typical dumbbell-shaped lesion of primary complex (Fig. 8.5).
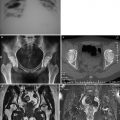
Fig. 8.5
(a, b) A male patient aged 16 years with primary tuberculosis. (a) Plain chest X-ray demonstrated spots of opacity at the margin of lateral zone in the middle right lung field, overlapping with ribs, and nodular opacity at the lower end of the middle bronchial segment adjacent to the right inferior pulmonary artery. (b) The lung window by CT scan demonstrated rare spots of opacity at the lateral segment of the middle right lung lobe and fusion of some spots. A cord-like opacity was displayed between the cluster of spots and the right lung hilum. The right lung hilum was shown to be enlarged due to right hilar lymphadenectasis
Intrathoracic Lymphoid Tuberculosis by Radiology
Pulmonary TB mainly manifested as enlarged lymph nodes at the hilum and mediastinum is known as intrathoracic lymphoid TB. Hilar lymphadenectasis can be classified into mass type and inflammation type.
Radiological demonstrations of mass-type hilar lymphadenectasis:
1.
Location: Mass type of right hilar lymphadenectasis is commonly located at the superior margin of the right hilum in the right hilar angle area around the course of the right inferior pulmonary artery. The mass type of left hilar lymphadenectasis is often located at the superior and lateral margin of left pulmonary artery arch around the course of the left inferior pulmonary artery. The mass type of right hilar lymphadenectasis is more common.
2.
Morphology: The totally exposed lymph nodes are nodular, round, or oval in shape, with intact and well-defined boundary. The partially exposed lymph nodes, due to overlapping partly with the vascular vessels in the hilar area, are semiarch-like protruding to the lung field (Fig. 8.6).
Fig. 8.6
(a–c) A male patient aged 21 years with intrathoracic lymphoid TB. (a) Plain chest X-ray demonstrated nodular opacity at the margin of right upper mediastinum. And the nodular opacity was semiarch in shape protruding to the lung field. (b) The lung window by CT scan displayed a nodular opacity beside the bronchus of the right upper mediastinum. The nodular opacity was arch shaped, protruding to the lung field. (c) The mediastinal window showed nodular opacity beside the right trachea, with spots of calcifications within and at the margin of the nodular opacity
3.
Density: The density may be either even or uneven. When caseous necrosis or liquefaction occurs in the lymph nodes, the density of the lesion is uneven. And sometimes calcification can be demonstrated. Enhanced scans show circular enhancement. When several lymph nodes are integrated into a lager mass, it shows separated enhancement. Obvious contrast can be demonstrated between enlarged lymph nodes and adjacent vascular vessels in the hilar area.
Radiological Demonstrations of Inflammation-Type Hilar Lymphadenectasis
1.
Due to caseous necrosis and capsular rupture of some lymph nodes, some lymph nodes are demonstrated with coarse unsmooth margin that is poorly defined. Otherwise, exudative inflammation around the lymph nodes causes the lymph nodes to be radiologically poorly defined.
2.
The major bronchial lumens in the hilar area are normally unobstructed, with well-defined and smooth inner wall. Occasionally, enlarged lymph nodes invade adjacent bronchi or tuberculosis of adjacent bronchi occurs to cause thickened bronchial wall and narrowed bronchial lumen.
Radiological Demonstrations of Mediastinal Lymphadenectasis
Mediastinal lymphadenectasis induced by tuberculosis is often located beside the trachea and in the tracheobronchial area, which is more common in the right lung. In most cases, several or several groups of lymph nodes are enlarged, with various sizes. The enlarged lymph nodes in the same group may be integrated, showing radiological sign of large mass opacity (Fig. 8.7).
Fig. 8.7
(a–c) A male patient aged 16 years with intrathoracic lymphoid TB. (a, b) The lung and mediastinum windows by CT scan demonstrated nodular lesions of enlarged lymph nodes at the right lower hilum and posterior mediastinum and obstructive pneumonia in the right middle lung lobe. (c) Contrast CT scans demonstrated consistently homogeneous enhancement of hilar major vascular vessels and thoracic aorta, which had obvious contrast to the adjacent nodular lymph nodes
8.6.1.2 Hematogenous Disseminated Pulmonary Tuberculosis
Acute Hematogenous Disseminated TB by Radiology
1.
Pulmonary interstitial miliary nodule
It is manifested as diffusively distributed miliary nodules in the interstitium of both lungs, which are about 1–3 mm in diameter. Their density, size, and distribution are even, mostly are well defined.
2.
Ground-glass opacity
It is manifested as focalized ground-glass opacity formed by integrated miliary nodules. The opacity has low density and is poorly defined.
3.
Interlobular septal thickening and intralobular reticular opacity
They are radiological signs induced by alveolar septal congestion and edema at the acute stage, commonly coexisting with ground-glass opacity. For most patients, they can subside after treatment.
4.
Clustered thin-walled cystic cavity opacity
In rare patients, it appears at the progressive stage and is reversible.
5.
Lobular central branch opacity and tree-bud sign
After delayed or inappropriate treatment, acute hematogenous disseminated TB progresses. The caseous substances formed in TB lesions involve alveolar cavities and spread through the bronchi. Therefore, randomly distributed nodules in both lungs and focally distributed lobular central branch opacity and tree-bud sign are radiologically displayed, which can be well or poorly defined (Fig. 8.8).
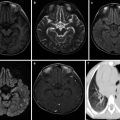
Fig. 8.8
(a–d) A female patient aged 14 years with acute hematogenous disseminated TB. (a) Plain chest X-ray demonstrated diffusively distributed miliary opacities in the upper, middle, and lower fields of both lungs. The miliary opacities were shown with the same size, even density, and even distribution. (b–d) The lung window by CT scan displayed diffusively distributed miliary opacities in the upper, middle, and lower fields of both lungs. The miliary opacities were shown with the same size, even density, and even distribution
Subacute and Chronic Hematogenous Disseminated Tuberculosis by Radiology
1.
The lesions are commonly located at the upper and middle parts of unilateral or bilateral lung fields.
2.
Exudative, hyperplastic, and even caseous lesions can coexist in upper lung field, manifesting as small nodular, patchy and mass opacities. In the middle lung field, the lesions are predominantly demonstrated as small nodular and miliary opacities. Therefore, the condition is manifested as long illness course of the lesions in the upper lung field and comparatively new lesions in the middle lung field (Fig. 8.9).
Fig. 8.9
(a–d) A male patient aged 24 years with subacute hematogenous disseminated TB. (a) Plain chest X-ray demonstrated patches of opacity with poorly defined boundary in the right upper lung field and lateral zone of left upper and middle lung fields. Small spots of and miliary opacities were displayed to be diffusively distributed in the upper and middle fields of both lungs, with poorly defined boundaries. (b–d) The lung window by CT scan demonstrated patches of opacity in the apical segment of the right upper lung lobe and lateral zone of apical posterior segment of the left upper lung lobe. The patches of opacity were accompanied by diffuse miliary opacities in both lungs, with uneven distribution
3.
Compensatory emphysema can be displayed between the lesions or in the lower part of the affected lung.
8.6.1.3 Secondary Pulmonary Tuberculosis
Secondary pulmonary TB refers to pulmonary TB occurring at any time after primary pulmonary TB, mainly including infiltrative pulmonary TB, tuberculous lobar pneumonia and caseous pneumonia, tuberculoma, and chronic fibrocavitary TB. Secondary pulmonary TB is one of the main types of pulmonary TB and is the most common type of pulmonary TB.
Infiltrative Pulmonary TB by Radiology
In cases of secondary pulmonary TB, the signs of primary pulmonary TB can sometimes be observed. The calcifications within the intrapulmonary primary lesions are demonstrated to be spotlike or nodular, with high density. Old peripheral inflammation around the lesions is common, with high central density and blurry boundary in shapes of patches and small flakes (Fig. 8.10).
Fig. 8.10
(a–c) A male patient aged 20 years with secondary pulmonary TB (specifically infiltrative pulmonary TB). (a) Plain chest X-ray demonstrated spots and small nodular and patches of opacity at the right upper lung field and interface of right upper and middle lung fields. Most of the opacities were poorly defined. (b, c) The lung and mediastinum windows by CT scan displayed spots and small nodular and patches of opacity at the right upper lung lobe. Most of the small nodular opacities were well defined. Calcifications were observable at the apical segment of right upper lung lobe
Secondary pulmonary TB:
1.
The lesions of secondary pulmonary TB are commonly located at the apical posterior segment of the upper lung lobe and the dorsal segment of the lower lung lobe.
2.
In overwhelming majority of the cases, the lesions are multiple. The lesions may be demonstrated within one lung lobe or one lung segment or within unilateral or bilateral lung fields.
3.
Exudative lesions are radiologically demonstrated as cloud-like opacity with spots, small flakes, or flakes of homogeneous or heterogeneous high-density shadows.
4.
Hyperplastic lesions are radiologically demonstrated as spots and small nodular or patchy mass-like opacity with relatively high density.
5.
Caseous dissolution occurs within the lesions to cause formation of semitransparent areas with low density or cavities. Radiologically, they are light-transparent areas with different sizes and shapes. Around the cavities, spots and small nodular opacity are demonstrated, which are known as satellite lesions (Fig. 8.11).
Fig. 8.11
(a–c) A male patient aged 25 years with secondary pulmonary TB (specifically cavitary pulmonary TB). (a) Plain chest X-ray demonstrated a thin-walled transparent area at the middle zone of right upper lung field, and its inferior wall overlapped with spots and small patches of opacities at the right middle lung field. (b, c) The lung window by CT displayed a transparent area at the posterior segment of right upper lung lobe. Between the transparent area and the lung hilum, there were dual tracks of draining bronchi. Around the transparent area, spots of satellite lesions were shown. Spots of bronchial disseminated lesions were detected at the right lower lung lobe
6.
Calcified lesions are radiologically demonstrated as spots and small nodular or linear opacity with high density.
7.
Fibrous lesions are radiologically demonstrated as cord-like or stellate-shaped opacity, with relatively high density and rough margins.
8.
Within a short period of time, progression and absorption of the lesions are slower than the lesion of lobar pneumonia and lobular pneumonia.
9.
The lesions of secondary pulmonary TB may be accompanied by pleural effusion.
10.
Secondary pulmonary TB may be complicated by hematogenous disseminated pulmonary TB. In addition to the infiltrative lesions in lung fields, the lesions of acute or chronic hematogenous disseminated pulmonary TB can be detected.
In cases of infiltrative pulmonary TB, two or more types of basic lesions such as exudation, proliferation, caseation, cavity, calcification, and fibrosis may be detected within the lungs of one patient. Radiologically, it is demonstrated with multiple lesions of different densities and various shapes. Especially, the apical posterior segment of both upper lung lobes is radiologically demonstrated with multiple lesions of various shapes and different densities. These signs are typical radiological signs of infiltrative pulmonary TB.
Tuberculous Lobar and Caseous Pneumonia by Radiology
Tuberculous Lobar Pneumonia by Radiology
Tuberculous lobar pneumonia is one of the uncommon types of secondary pulmonary TB. It is also known as bronchopneumonic TB:
1.
The lesions are commonly located at the apical posterior segment of the upper lung lobe.
2.
The lesion is radiologically shown as large flake of opacity, occupying one lung segment, one lung lobe, or even unilateral lung field. At its central area, a large area of consolidation can be found, with poorly defined boundary. Air bronchogram sign is displayed in the large flake of consolidation.
3.
In the cloudy opacity, spots and small nodular lesions with high density are displayed. Radiologically, it is displayed as a large flake of lesion surrounded by small lesions. These small lesions scatter with uneven distribution. These radiological signs facilitate the differential diagnosis from lobar pneumonia. Its mechanism involves exudative and proliferative pathological changes of the lesions in the lungs induced by M. tuberculosis infection.
4.
Within the large flake of consolidation opacity or at its margin, small low-density semitransparent areas or small transparent areas can be detected. These small areas indicate small caseous necrosis or small dissolution and liquefaction of the lesions.
5.
Scattering polymorphic spots and small nodular or patches of TB lesions in isolateral or contralateral lung field of the lesions facilitate the diagnosis (Fig. 8.12).
Fig. 8.12
(a–c) A male patient aged 36 years with secondary pulmonary TB (specifically tuberculous lobar pneumonia). (a) Plain chest X-ray demonstrated large flaky opacity at the right upper lung field, with poorly defined boundary, and spot of opacity at the right middle lung field. (b, c) The lung window by CT scan displayed large flaky opacity at the right upper lung lobe, with air bronchogram sign inside. The lesion had poorly defined boundary, which was accompanied by small flakes and spots of opacities. Small flakes and spots of opacities were also shown at the middle and lower lobes of the affected lung
Caseous Pneumonia by Radiology
Caseous pneumonia is one of the most serious types of secondary pulmonary TB. Its pathogenesis involves invasion of the lungs by large quantities of M. tuberculosis via the bronchi within a short period of time. Due to compromised immunity, the hosts who are hypersensitive to the antigen of M. tuberculosis show rapidly deterioration and progression of the condition into lobar or lobular caseous pneumonia. In some cases, caseous pneumonia is resulted from caseous necrosis of exudative lesions of tuberculous lobar pneumonia (Fig. 8.13):
Fig. 8.13
(a, b) A female patients aged 30 years with secondary pulmonary TB (specifically caseous pneumonia). The lung and mediastinum windows by CT scan displayed large flaky opacity at the right upper lung lobe. Within the lesion, multiple transparent areas were shown with different sizes and irregular shape. The mediastinum window by CT scan demonstrated spots of calcification in the lesion. The left upper lung lobe was demonstrated with cord-like opacity
1.
Lobar caseous pneumonia is radiologically shown as large flakes of cloud-like opacities that gradually develop into large flake of consolidation with intermediate density. The consolidation is more common at the upper lung lobes and occupies one lung segment, one lung lobe, or even unilateral lung, with poorly defined boundary.
2.




The density of lesion is heterogeneous. And the lesion is radiologically demonstrated as large flake of consolidation with extensive multiple semitransparent or transparent areas inside. The semitransparent or transparent areas are worm-bitten-like in shape with low density. The shape of cavities is also diversified and irregular, with poorly defined and unsmooth cavity wall.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree