Vascular diseases of the lung may affect arteries, veins, and/or capillaries. They are primarily evaluated using modalities such as echocardiography, contrast-enhanced CT, or conventional angiography, but in selected cases, HRCT may give an insight not provided by other imaging studies.
HRCT provides an accurate assessment of lung parenchymal abnormalities, but may also allow for a limited assessment of abnormalities directly involving the pulmonary arteries, pulmonary veins, and heart. This chapter focuses upon the pulmonary manifestations of pulmonary vascular disease.
PULMONARY HYPERTENSION
HRCT Findings
Pulmonary hypertension (PH) may be seen with a variety of diseases that affect the lung parenchyma, pulmonary arteries, pulmonary veins, and heart. While pulmonary artery (PA) pressures cannot be directly estimated using HRCT, it may show signs that suggest the presence and relative severity of PH (Table 7.1).
Enlargement of the Main PA
Main PA diameter correlates with the presence or absence of pulmonary arterial hypertension. This correlation is significantly more accurate in patients without parenchymal lung disease than in those with lung disease.
PA diameter should be measured perpendicular to the long axis of the vessel. This may be challenging using HRCT with spaced sections. The threshold above which PH can be said to be present varies in the literature. A threshold diameter of 3.3 cm is relatively specific for this diagnosis. The PA should also be smaller than the adjacent aorta (Fig. 7.1).
Increased Right Ventricular Size
Right ventricular (RV) size may be difficult to assess on HRCT images obtained without contrast injection; however, in many cases the location of the interventricular septum may be estimated even on non-contrast images (Fig. 7.2). The transverse diameter of the RV should be less than the left ventricle. PH is a common cause of RV enlargement.
Increased Size of the Right Atrium, Superior Vena Cava, and Inferior Vena Cava
In the setting of PH, the right atrium (Fig. 7.3), superior vena cava, and inferior vena cava are often enlarged due to tricuspid regurgitation. The size of these structures can usually be determined on non-contrast images. There are no specific size thresholds to use, and enlargement is mainly determined by reader experience. These signs are the least specific for PH as enlargement may be caused by multiple other etiologies.
Table 7.1 HRCT findings that may be associated with pulmonary hypertension
Enlargement of the main pulmonary artery
Increased right ventricular size
Increased right atrial size
Increased size of superior/inferior vena cava Mosaic perfusion
Centrilobular nodules
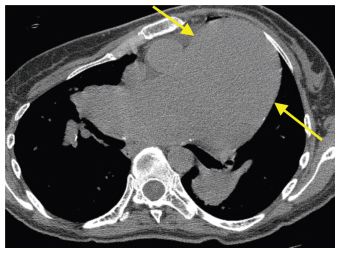
Figure 7.1
Main pulmonary artery enlargement. There is marked dilatation of the main pulmonary artery (arrows) in a patient with idiopathic pulmonary arterial hypertension.
Mosaic Perfusion
Heterogeneous lung attenuation due to regional alterations in blood flow is termed mosaic perfusion (see Chapter 5). Mosaic perfusion may be seen with either airways disease or vascular disease, the former being significantly more likely. Mosaic perfusion may be seen with any cause of PH, but is most common with chronic pulmonary thromboembolic disease.
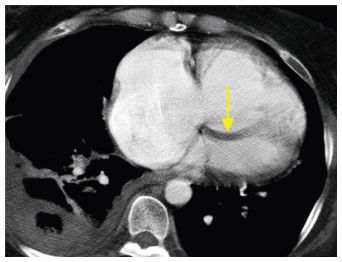
Figure 7.2
Right ventricular enlargement. The diameter of the right ventricle is significantly greater than that of the left ventricle in a patient with pulmonary hypertension due to chronic pulmonary thromboembolism. Bowing of the interventricular septum toward the left ventricle (arrow) is also seen.
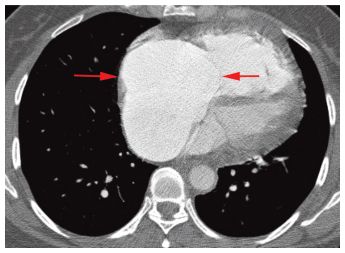
Figure 7.3
Right atrial enlargement. The right atrium (arrows) is markedly dilated in a patient with idiopathic pulmonary arterial hypertension. This finding is often due to tricuspid regurgitation resulting from dilatation of the right ventricle.
The appearance of mosaic perfusion may help to distinguish airways and vascular causes. Vascular disease usually presents with larger, peripheral, non-lobular regions of decreased lung attenuation (Fig. 7.4). Small airways disease typically shows smaller patchy regions of mosaic perfusion, some of which appear lobular.
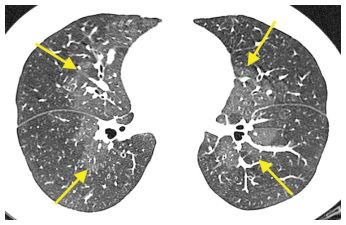
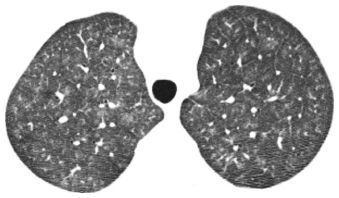
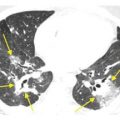
Figure 7.4
Mosaic perfusion. Heterogeneous lung attenuation is present with peripheral lung appearing decreased in attenuation and central lung regions (arrows) appearing to be of increased attenuation. In this case, the lower attenuation lung is abnormal, resulting from decreased perfusion due to vasculitis.
Centrilobular Nodules
The distal pulmonary arteries are centrilobular in location, and diseases that affect the pulmonary arterial system may manifest as centrilobular nodules. Centrilobular nodules from a vascular etiology are often of ground glass opacity (Fig. 7.5). These may be seen in association with pulmonary arterial hypertension of any cause, but they are most common with idiopathic pulmonary arterial hypertension (IPAH), capillary hemangiomatosis, pulmonary veno-occlusive disease, and vasculitis. They often reflect the presence of pulmonary edema or hemorrhage, or cholesterol granulomas, which are an indication of previous hemorrhage.
Centrilobular nodules are not specific for a vascular etiology as they may also be seen with pulmonary edema or hemorrhage (Fig. 7.6) of any cause and airways diseases such as hypersensitivity pneumonitis. In a patient with known PH, however, they are likely due to the vascular disease.
Diseases Associated with PH
The differential diagnosis of PH is very broad (Table 7.2). HRCT may be obtained in the diagnostic evaluation of a patient with PH of unknown cause. One major role of HRCT in this setting is the detection of diffuse lung disease, primarily emphysema and lung fibrosis. Contrast-enhanced CT may also be obtained to evaluate for chronic pulmonary thromboembolism (CPTE).
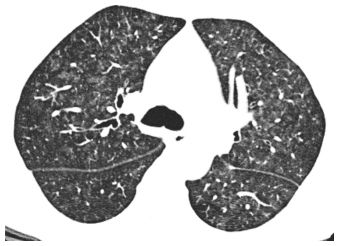
Figure 7.5
Centrilobular nodules of ground glass opacity in pulmonary hypertension. Ill-defined centrilobular ground glass opacity nodules are often seen in primary and secondary causes of pulmonary hypertension. They may represent focal areas of edema, hemorrhage, or cholesterol granuloma formation.
Figure 7.6
Centrilobular nodules of ground glass opacity. The nodules in this patient represented pulmonary hemorrhage due to systemic lupus erythematosus. Nodules of this type commonly have causes other than pulmonary hypertension. These include edema and hemorrhage unrelated to pulmonary vascular disease, hypersensitivity pneumonitis, and respiratory bronchiolitis.
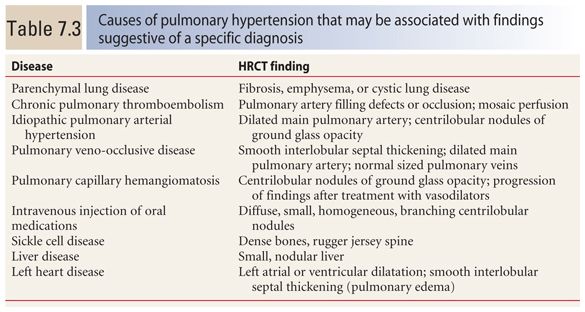
There are many causes of PH that are not well evaluated using HRCT. These are unified by a relative lack of lung abnormalities or the presence of nonspecific lung findings. Examples include systolic or diastolic left ventricular dysfunction, valvular heart disease, cardiovascular shunts, hypoventilation disorders, and sleep disorders. The discussion of specific diseases associated with PH will be restricted to those that commonly show lung abnormalities on HRCT (Table 7.3).
Table 7.2 Differential diagnosis of pulmonary hypertension
Parenchymal lung disease (emphysema, fibrosis, cystic lung disease)
Hypoxemia without parenchymal lung disease
Chronic pulmonary thromboembolism
Fibrosing mediastinitis
Left-sided heart disease
Congenital systemic to pulmonary shunts Vasculitis
Liver disease
Human immunodeficiency virus infection
Drugs
Sickle cell anemia
Idiopathic pulmonary arterial hypertension
Familial pulmonary arterial hypertension
Pulmonary veno-occlusive disease
Capillary hemangiomatosis
Intravenous injection of oral medications
Parenchymal Lung Disease
PH may result from parenchymal lung disease because of hypoxia (with vasoconstriction) or obliteration of the pulmonary capillary bed. The most common lung parenchymal processes to result in PH are emphysema (Fig. 7.7A, B) and diffuse lung fibrosis (Fig. 7.8A, B). Cystic lung disease is a rare cause of PH.
Lung fibrosis causing PH is most commonly due to idiopathic pulmonary fibrosis, connective tissue disease, or sarcoidosis. Chronic airways disease, such as cystic fibrosis, and cystic lung disease, such as lymphangioleiomyomatosis or Langerhans histiocytosis, may also be associated with PH. As lung disease associated with PH is typically extensive, it should be evident on HRCT. The lack of significant abnormality on HRCT makes a lung etiology of PH unlikely. In general, the severity of lung disease correlates with the degree of PH.
Sarcoidosis and connective tissue disease– related interstitial lung disease (Fig. 7.9A–C) may show PH disproportionate to the extent of lung disease. In these cases, vasculitis, thrombosis, stenosis, or occlusion of small pulmonary arteries likely contribute. Of note, in the presence of lung disease, there is a poor correlation between main PA diameter and the severity of PH. This is in contrast to IPAH and other diseases without significant lung manifestations in which pulmonary arterial diameter shows better correlation with the presence and severity of PH.
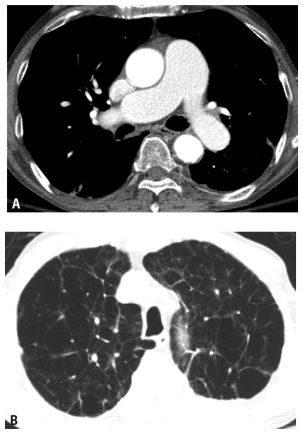
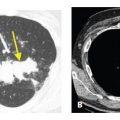
Figure 7.7
Pulmonary hypertension due to emphysema. A. The main pulmonary artery is enlarged in this patient with pulmonary hypertension. B. On lung windows, extensive centrilobular emphysema is visible.
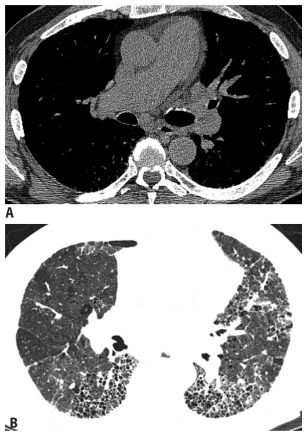
Figure 7.8
Pulmonary hypertension associated with lung fibrosis. Mild main pulmonary artery enlargement (A) is associated with fibrosis (B) in this patient with idiopathic pulmonary fibrosis.
Chronic Pulmonary Thromboembolism
The diagnosis of CPTE may be challenging. Patients present with nonspecific symptoms and initial objective examinations, such as pulmonary function tests, are nonspecific. Contrast-enhanced CT pulmonary angiography, while effective in the setting of acute pulmonary thromboembolism, has limited sensitivity in the diagnosis of CPTE.
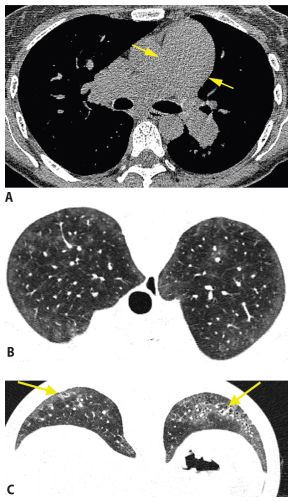
Figure 7.9
Pulmonary hypertension in connective tissue disease. This patient with scleroderma and pulmonary hypertension shows enlargement of the main pulmonary artery (arrow) (A). A prone scan through the upper lobes (B) shows lobular areas of ground glass opacity, perhaps pulmonary edema or hemorrhage related to pulmonary hypertension. In the lower lobes (C) mild fibrosis is present (arrows); it is too mild to explain the pulmonary hypertension. This patient likely has vasculitis contributing to pulmonary hypertension.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree