Radiologic Evaluation of the Arthritides
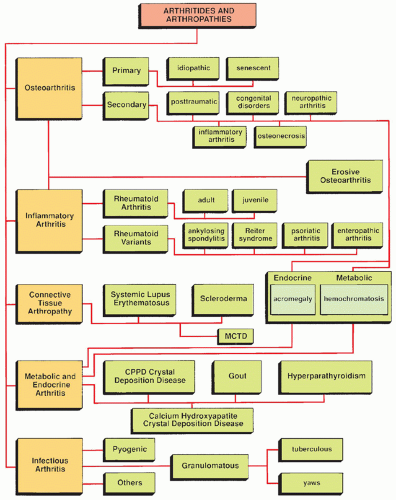
In its general meaning, the term arthritis indicates an abnormality of the joint as the result of a degenerative, inflammatory, infectious, or metabolic process (Fig. 12.1). Also included among the arthritides are connective tissue arthropathies, such as those associated with systemic lupus erythematosus (SLE) and scleroderma.
Radiologic Imaging Modalities
Conventional Radiography
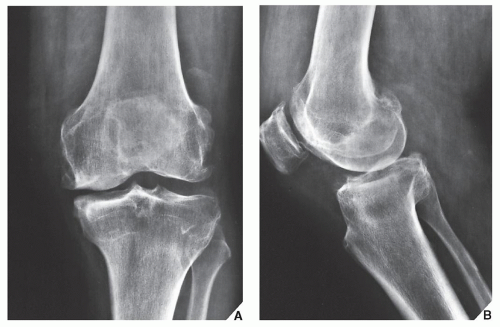
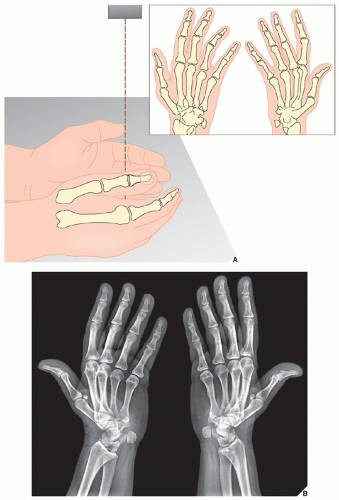
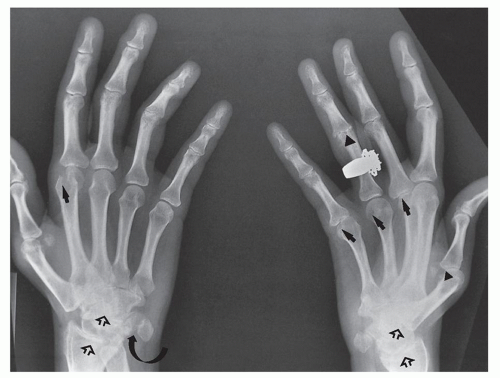
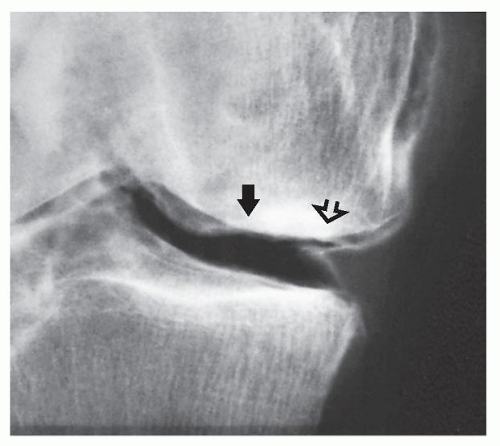
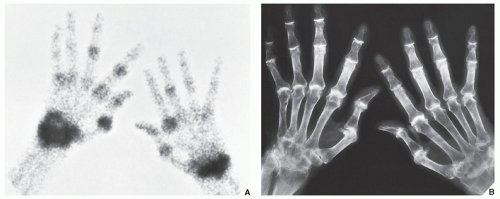
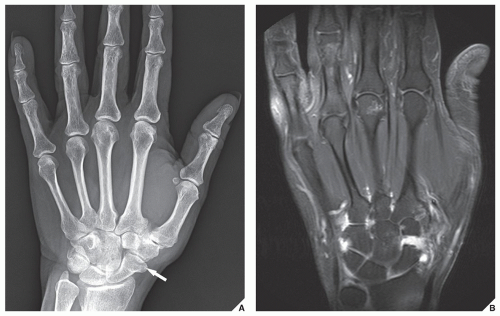
The radiologic modalities used to evaluate arthritis are very similar to those used in traumatic conditions involving the bones and joints (see Chapter 4), although there are some modifications. The most important modality for the evaluation of arthritis is conventional radiography. As in the radiographic examination of traumatic conditions, standard radiographs of the involved joint should be obtained in at least two projections at 90 degrees to each other (Fig. 12.2; see also Fig. 4.1). A weight-bearing view may be of value, particularly for a dynamic evaluation of any decrement in the joint space under the weight of the body (Fig. 12.3). Special projections may at times be required to demonstrate destructive changes in the joint to better advantages. The radial head-capitellum view (see Chapter 6), by eliminating overlap of the radial head and coronoid process and by more clearly demonstrating the humeroradial and humeroulnar joints, shows the inflammatory changes in the elbow joint to better advantage (Fig. 12.4). The semisupinated oblique view of the hand and wrist (the so-called Allstate or ball-catcher’s view), introduced by Norgaard in 1965, effectively demonstrates the radial aspects of the metacarpal heads and of the base of the proximal phalanges in the hand and the triquetrum and pisiform in the wrist (Fig. 12.5). Because the earliest erosive changes of some inflammatory arthritides begin in these areas, the Norgaard view may provide important information at the early stages of arthritides (Fig. 12.6). It may also demonstrate subtle subluxations in metacarpophalangeal joints frequently seen in SLE.
Magnification Radiography
This technique was used in the past to diagnose the very early articular changes of arthritis, which were not well appreciated on standard projections. The method involved a special screen-film system and geometric enlargement that yielded magnified images of the bones and joints with greater sharpness and bony detail. Magnification radiography is now completely replaced by digital radiography and cutting-edge technology of picture archive and communication system (PACS) for radiology images, allowing filmless high-resolution image display format with advanced radiology reading workstations.
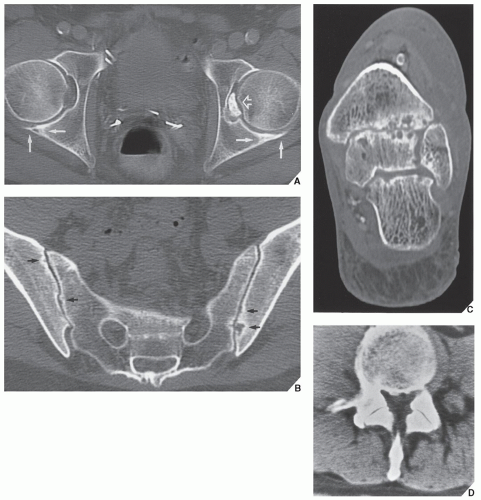
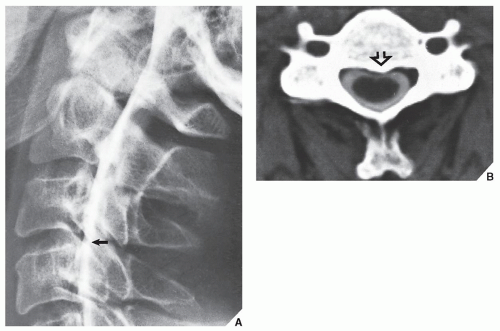
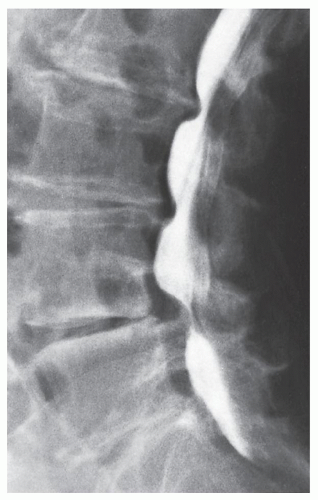
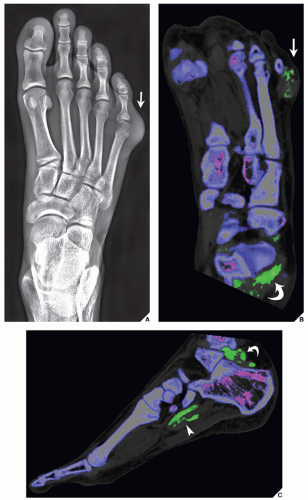
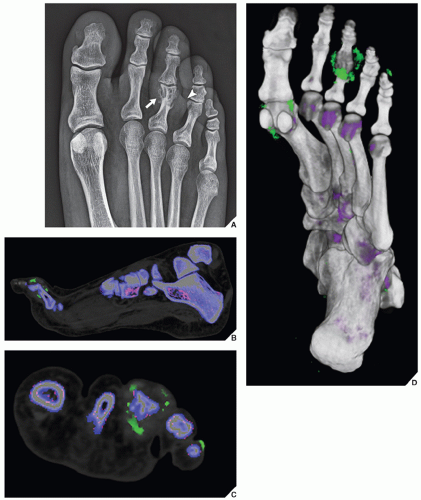
Tomography, Computed Tomography, and Arthrography
Among the ancillary imaging techniques, conventional tomography was used in the past—its major purpose being demonstration to better advantage the degree of joint destruction. Currently, it has been replaced by computed tomography (CT), which is effective in evaluating degenerative and inflammatory changes of various joints (Fig. 12.7A to C) and in the spine to document spinal stenosis (Fig. 12.7D). In the assessment of spinal stenosis secondary to degenerative changes, CT examination may also be performed after myelography (Fig. 12.8), although myelography alone is often sufficient (Fig. 12.9). Recently, dual-energy CT gained a wide acceptance as a modality used for detection or exclusion of tophaceous gout (Figs. 12.10 and 12.11; see also Figs. 2.16 and 15.28). In addition, in patients with known tophaceous gout, this technique may be used for serial volumetric quantification of subclinical tophus to evaluate response to treatment. Arthrography has some limited application in the evaluation of degenerative (Fig. 12.12), inflammatory, and infectious conditions of the joint (see Fig. 25.22B).
Scintigraphy
Radionuclide bone scan is much more commonly used than those other techniques, mainly for evaluating the distribution of arthritis in different joints (see Chapter 2). The radiopharmaceuticals currently in use in bone scan include organic diphosphonates—ethylene diphosphonate (EHDP) and methylene diphosphonate (MDP)—labeled with 99mTc, a gamma emitter with a 6-hour half-life; MDP is more commonly used, typically in a dose that provides 15 mCi (555 MBq) of 99mTc. After intravenous injection of the radiopharmaceutical, approximately 50% of the dose localizes in bone, with the remainder circulating freely in the body and eventually excreted by the kidneys. A gamma camera can then be used in a procedure known as a three-phase radionuclide bone scan. Scintigraphy can determine the distribution of arthritic changes in large and small joints (Fig. 12.13). It can also distinguish an infected joint from infected periarticular soft tissues (see Fig. 24.9). To distinguish infectious arthritis from other forms of arthritides, 111In-labeled leukocytes and 57Ga scans are employed (see Chapter 2, section on “Scintigraphy”).
Serial examinations with bone scintigraphy, as Brower and Flemming have pointed out, have also been helpful in evaluating the activity of given arthritis at a particular point in time. Such examinations may differentiate active disease from arthritis in remission.
Recently, high-resolution single photon emission CT (SPECT) trials have been attempted to detect osseous alterations in early stages of rheumatoid arthritis and erosive osteoarthritis with promising results.
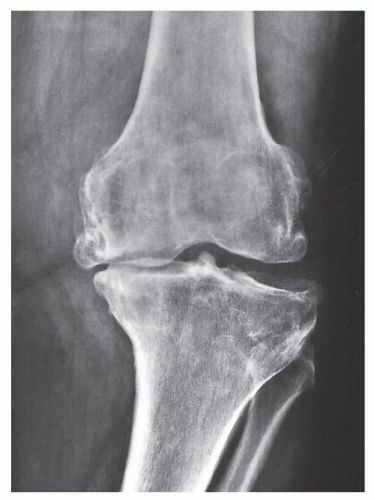 FIGURE 12.3 Osteoarthritis. Weight-bearing anteroposterior radiograph of the left knee of the same patient shown in Figure 12.2 demonstrates collapse of the medial femorotibial compartment under the weight of the body, with a resulting varus configuration of the knee. |
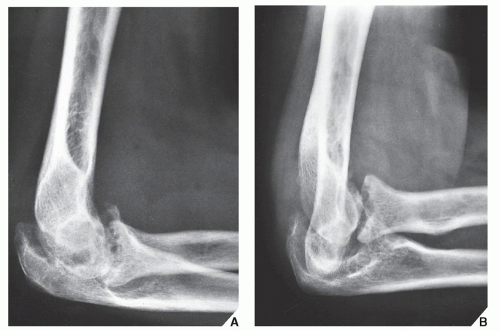 FIGURE 12.4 Rheumatoid arthritis. (A) Standard lateral radiograph of the elbow of a 48-year-old woman with known rheumatoid arthritis of several years’ duration shows destructive changes typical of inflammatory arthritis. (B) A special projection known as the radial head-capitellum view (see also Fig. 6.14) demonstrates to better advantage the details of the arthritic process involving the humeroradial and humeroulnar joints. (From Greenspan A, Norman A. Radial head-capitellum view in elbow trauma [Letter]. Am J Roentgenol. 1983; 140:1273-1275.) |
Ultrasound
Ultrasound (US) is occasionally used in the evaluation of joint abnormalities. This technique helps to differentiate popliteal fossa masses in patients with rheumatoid arthritis, in whom complications of an arthritic process (such as popliteal cyst or hypertrophied synovium) may be distinguished from conditions not related to arthritis (such as popliteal artery aneurysm) (see Figs. 2.22 and 2.25). It may also effectively diagnose deep vein thrombosis, occasionally seen in patients with rheumatoid arthritis (see Fig. 2.23). At times, US may demonstrate osseous erosions and inflammatory pannus. Recently some investigators have explored the use of power Doppler US in the evaluation of rheumatoid synovitis.
Magnetic Resonance Imaging
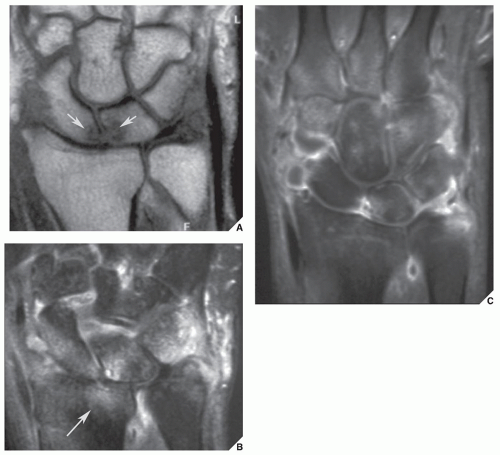
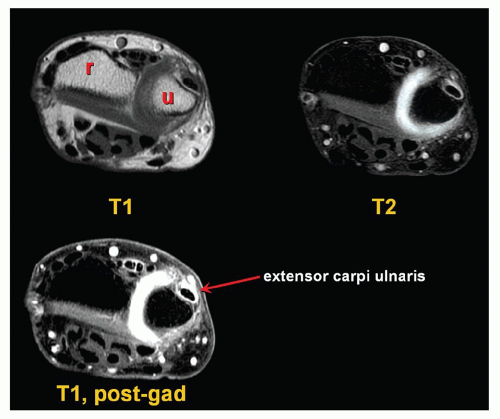
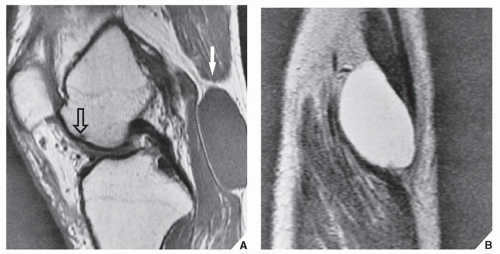
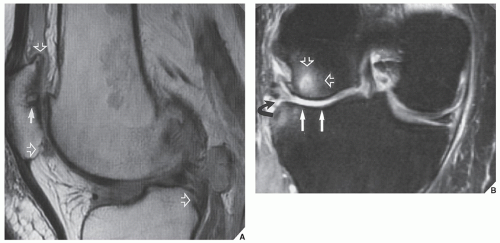
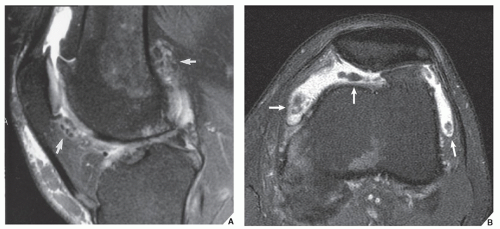
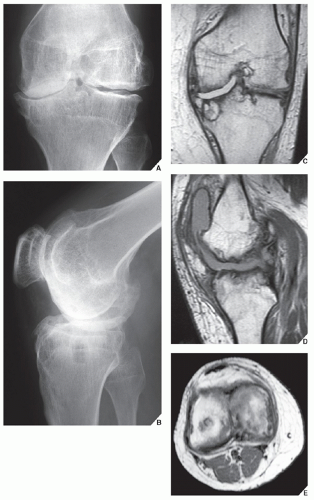
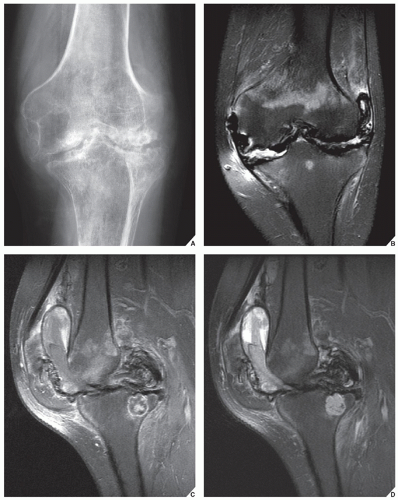
Magnetic resonance imaging (MRI) of the joints provides excellent contrast between soft tissues and bone. Articular cartilage, fibrocartilage, cortex, and spongy bone can be distinguished from each other by their specific signal intensities. It is an excellent modality for demonstrating the rheumatoid nodules and synovial abnormalities in patients with rheumatoid arthritis. MRI’s ability to contrast the synovium-covered joint from other soft-tissue structures allows for noninvasive delineation of the degree of synovial hypertrophy that accompanies synovitis, previously demonstrable only by means of arthrography or arthroscopy. Because synovitis is often accompanied by joint effusion, this too can be effectively demonstrated by MRI (Fig. 12.14). In particular, when this technique is combined with intravenous administration of gadolinium diethylenetriamine penta-acetic acid (Gd-DTPA), it is highly effective in differentiation between fluid-filled joints and tendon sheaths from synovitis. Both, fluid and intraarticular synovial tissue exhibit an intermediate signal intensity on T1-weighted images and a high signal on T2 weighting. However, gadolinium-enhanced T1-weighted images will show high-intensity signal of inflammatory pannus/synovial tissue, whereas fluid will not enhance (Figs. 12.15 and 12.16). MRI is also quite helpful in diagnosing Baker cyst (Fig. 12.17). Although MRI is quite sensitive in detecting joint effusion, it cannot yet distinguish between inflammatory fluid and noninflammatory fluid. Occasionally, MRI may provide some additional information on osteoarthritis (Figs. 12.18 and 12.19) and hemophilic arthropathy (Figs. 12.20 and 12.21). With the development of more sophisticated orthopedic methods for cartilage repair in osteoarthritis, such as new articular cartilage replacement techniques, including chondrocyte transplantation, osteochondral transplantation, and cartilage growth-stimulating factors, optimized MRI of these interventions for diagnosis and treatment planning in osteoarthritis is essential. Recent investigations of the value of contrast-enhanced MRI with subtraction technique proved to be useful for early detection of active sacroiliitis.
The most promising role of MRI, however, is in the evaluation of the spine. MR images in the sagittal plane are useful for demonstrating hypertrophy of the ligamentum flavum or the vertebral facets, grading the degree of foramina stenosis, and measuring the sagittal diameter of the spinal canal and the spinal cord. MR images in the axial plane facilitate detailed analysis of the facet joints and more accurate measurement of the thickness of the ligamentum flavum and the diameter of the spinal canal. The quality of evaluation of spinal cord abnormalities by MRI in the cervical area in patients with rheumatoid arthritis and of spinal stenosis in patients with advanced degenerative changes of the spine surpasses that obtained with other modalities. MRI is particularly useful in the examination of patients with pain related to disk disease because it can differentiate normal, degenerated, and herniated disks noninvasively (see Chapter 11). In fact, the changes of disk degeneration can be identified by MRI long before they can be detected by conventional radiography or CT.
The Arthritides
Diagnosis
Clinical Information
The accurate diagnosis of specific arthritis depends on many factors; however, the most important is to understand the patterns of symptoms and the mechanism of disease.
The clinical manifestations and laboratory data, in conjunction with the imaging findings, are of significant help in making the diagnosis of a specific arthritic process. The various arthritides, for example, have different frequencies of occurrence between the genders. Rheumatoid arthritis is much more common in females, and erosive osteoarthritis is seen almost exclusively in middle-aged women. Psoriatic arthritis, Reiter syndrome (currently known as reactive arthritis), and gouty arthritis, however, are more common in males. Clinical symptoms are of further assistance. Patients with reactive arthritis, for example, usually present with urethritis, conjunctivitis, and mucocutaneous lesions, and those with psoriatic arthritis may present with swelling of a single finger, the so-called sausage digit, as well as changes in the skin and fingernails. Patients with gouty arthritis may exhibit soft-tissue masses, representing chronic tophi, on the dorsal aspect of the hands or feet.
Laboratory data are also essential. Gouty arthritis, for instance, is associated with elevated serum uric acid concentrations, and a synovial fluid examination reveals monosodium urate crystals in leukocytes in the fluid. The synovial fluid of patients with pseudogout, however, contains calcium pyrophosphate crystals. The detection of autoantibodies is another important aid in the diagnostic workup. Rheumatoid factor (RF) is a typical finding in rheumatoid arthritis. Patients lacking the specific antibodies represented by RF are said to have “seronegative” arthritis. Patients with lupus arthritis have a positive lupus erythematosus cell test. Lastly, identification of the antigens of the major histocompatibility complex, particularly human leukocyte-associated antigens HLA-B27 and HLA-DR4, has in recent years become a crucial test in the diagnosis of arthritic disease. It has been reported that 95% of patients with ankylosing spondylitis, 86% of patients with reactive arthritis, and 60% of patients with psoriatic arthropathy test positively for antigen HLA-B27, whereas a majority of those with rheumatoid arthritis exhibit the HLA-DR4 antigen. This is helpful in differentiating certain types of arthritides as well as distinguishing psoriatic arthritis from rheumatoid arthritis in cases in which the radiographic presentation of these conditions may be very similar.
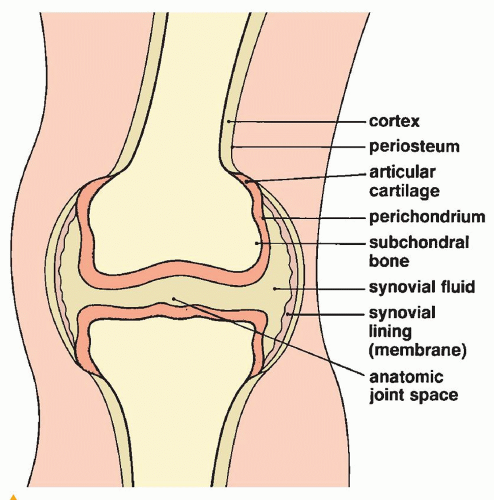 FIGURE 12.22 The constituent structures of a true or diarthrodial joint.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|