(Left panel from Rubin P, Hansen JT. TNM Staging Atlas with Oncoanatomy, 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2012:115.)
1. ANATOMY
• The rectum is located anterior to the lower sacrum, and extends from the rectosigmoid junction at the level of the third sacral vertebrae to the puborectalis ring. It is approximately 12 to 15 cm long, and is divided into three parts based on the distance from the anal verge.
• The upper third of the rectum is deep in the pelvis and is covered with peritoneum anteriorly and bilaterally. The middle third of the rectum is covered by the peritoneum anteriorly, and the lower third of the rectum is subperitoneal without peritoneal covering.
2. NATURAL HISTORY
2.1. Lymphatic Drainage
• Rectal cancer drains to perirectal, presacral, obturator, and internal iliac nodes. The upper half of the rectum drains to the perirectal and inferior mesenteric nodes.1,2
3. DIAGNOSIS AND STAGING SYSTEM
3.1. Signs and Symptoms
• The majority of patients present with rectal bleeding, hematochezia, mucous in the stool, change of bowel habit, and signs of rectal obstruction such as decreased stool caliber, diarrhea, constipation, incomplete emptying of the stool, and tenesmus.
• In patients with posterior extension of the disease, urinary symptoms and perineal pain can occur. Tumor invasion of sciatic notch can cause sciatic pain.2
3.2. Physical Examination
• In addition to complete history including family history of colorectal cancers and personal history of polyps, thorough digital examination of the rectum to evaluate the size, mobility, location, diameter of rectal lumen, and any ulceration of the tumor is warranted.
• Assessment of sphinter tone and function is also important for selecting candidates for sphincter preservation.
• For female patients, gynecologic exam is helpful to rule out other sites of disease origins.
• Sigmoidoscopy and proctoscopy provide direct visualization, allow biopsy of the lesion, and help evaluate the extent of obstruction and disease distance from anal verge. Colonoscopy should be done to look for synchronous lesions in the large bowel.2
3.3. Imaging
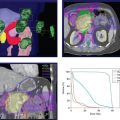
• The main imaging tools for rectal cancer are endorectal ultrasound (EUS), computed tomography (CT) of the chest, abdomen, and pelvis, and magnetic resonance imaging (MRI) of the pelvis.
• Either EUS or MRI can be used to determine the T and N classification. CT can be used to evaluate nodal involvement and metastatic disease.
3.4. Staging
• The American Joint Committee on Cancer issued new staging guidelines in 2010.3 Changes include new subdivisions in stages II and III as well as the splitting of T4 into T4a and T4b lesions. Readers are strongly urged to consult the new manual for these and other changes.
4. PROGNOSTIC FACTORS
• Stage: Clinical and pathologic T and N categories are important prognostic factors.4 Tumors that are further away from anal verge are more favorable compared to more distal tumors.
• Treatment-related and Surgical Factors: Favorable response to neoadjuvant chemoradiation is associated with longer disease-free survival.5 The circumferential resection margin or radial margin is significantly associated with rates of local recurrence and overall survival. The number of lymph nodes examined is associated with disease-free survival among node-negative patients.
5. GENERAL MANAGEMENT
• For early-stage rectal cancer (T1-2, N0), surgery alone is usually recommended. For patients with resectable tumors invading beyond the bowel wall (T3-T4), and/or nodal involvement, combined modality therapy including preoperative chemoradiation therapy with infusional 5-FU (5-fluorouracil) or capecitabine followed by total mesorectal excision and adjuvant chemotherapy is recommended.
• Treatment needs to be individualized for patients with metastatic disease. Depending on the clinical situation, these patients may need any or all of the following: chemotherapy, surgery for the primary, surgery for the metastasis, and radiation therapy.
5.1. Surgical Management
• Common sphincter-preserving operations are local excision and low anterior resection. Abdominoprineal resection is a nonsphincter-sparing procedure typically reserved for distal tumors close to the anal verge.1
• Local excision, usually through a transanal approach, can be considered for selected T1N0 rectal cancers.
• Total mesorectal excision is now accepted as a standard of care for rectal cancer. Complete removal of the mesorectal fat and lymph nodes enhances local control.
5.2. Combined Modality Treatment
• Preoperative chemoradiation therapy combined with total mesorectal excision followed by postoperative chemotherapy is recommended for T3-T4 tumors or those with positive lymph nodes.
• Postoperative irradiation can be used for those with clinical T1-2 N0 disease but later found to have more advanced pathologic stage after surgery.
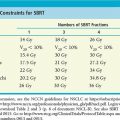
5.3. Radiation Therapy
• Preoperative chemoradiation therapy has the advantage of downsizing the tumor and making sphinter preservation more feasible, especially for distally located lesions. Preoperative chemoradiation also offers better local control, toxicity, and sphincter preservation compared with postoperative chemoradiation therapy.6 The common preoperative radiation dose is 45 Gy to the pelvis plus a boost of 5.4 Gy to the tumor, involved nodes, and adjacent pelvic and presacral regions.
• A shorter course of preoperative radiation therapy consisting of 25 Gy in 5 daily fractions has also been shown to improve local control and survival compared to surgery alone.7,8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree