Renal Vein Thrombosis
Renal vein thrombosis (RVT) was first described by Reyer in 1840.1 The first report in the English literature occurred in 1926 by Aschner, who described five cases, four in adults and one in an infant.2 At this time, the mortality rate was high, and most diagnoses were made at autopsy. In 1942, Campbell and Matthews3 reported the first preoperative diagnosis of RVT that was subsequently confirmed at the time of surgery. Emergent nephrectomy was advocated for unilateral disease and generally supported until 1964, when Stark4 reported the full recovery of three infants treated with conservative measures alone. It is now recognized that whereas RVT can occur spontaneously and without preexisting conditions, by far most cases occur secondary to intrinsic renal disease.
 Etiology
Etiology
Renal vein thrombosis is intimately related to and dependent on Virchow’s triad, which includes (1) venostasis; (2) endothelial injury; and (3) a hypercoagulable state. The occurrence of any of these three conditions alone within the renal venous system can result in RVT. The newborn infant is particularly susceptible to RVT because of (1) the risk of hemoconcentration and dehydration secondary to poor fluid intake and (2) the characteristically low renal perfusion resulting from the two consecutive (afferent/efferent) intrarenal capillary beds.5–7 Venous congestion results in regional hypoxia, cellular disruption, and intrarenal parenchymal hemorrhage. RVT starting in the arcuate and intralobular veins can remain localized or propagate into the main renal vein and inferior vena cava (IVC) (Fig. 35–1). Predisposing factors to RVT in infants and children are shown in Table 35–1. Prenatal RVT also has been diagnosed both in utero10 and after delivery13 based on the ultrasound findings of a calcified thrombus.
Ricci and Lloyd5 classified 46 infants with RVT presenting over a 32-year period as falling into one of three groups. Group 1 (9%) consisted of healthy full-term infants with no underlying medical problem. Group 2 comprised infants and young children who had a medical condition that could predispose to RVT, such as cyanotic congenital heart disease, necrotizing enterocolitis, and acute myelogenous leukemia. This was the largest group, constituting 72% of the study population. Group 3 (19%) included children who had severe underlying concomitant renal disease, in particular the nephrotic syndrome (NS).
In adults, RVT can be due to dehydration and shock; however, most cases are secondary to the nephrotic syndrome occurring as a result of underlying and severe medical renal disease. A review of the literature by Zucchelli14 reported the incidence of RVT in patients with NS to vary from 1.9 to 42.3%. Other diseases responsible for RVT includes systemic lupus erythematosus (Fig. 35–2)15,16 and primary antiphospholipid syndrome.17,18 Renal vein thrombosis involving grafts has been reported in patients status post renal transplant receiving high-dose prophylactic OKT3 administration.19
Obstructive RVT can occur with primary and secondary tumors of the kidney and adrenal glands. These neoplasms can involve the ipsilateral renal vein and extend into the IVC (Figs. 35–3 and 35–4) and right atrium, with embolization to the lung.20 Retroperitoneal malignancies such as lymphoma and primary wall tumors of the renal vein and JVC (leiomyosarcoma) also can result in RVT. Inflammatory processes such as pancreatitis, abscess, and retroperitoneal fibrosis likewise can cause RVT. Iatrogenic injuries to the renal vein secondary to surgery or misplacement or migration of an IVC filter can compromise renal vein flow. Anatomic conditions resulting in compression of left renal vein between the superior mesenteric artery and the aorta (“nutcracker” phenomenon) also can cause mechanical obstruction of the vessel.21 Spontaneous renal vein thrombosis in adult patients with no underlying medical condition also has been reported.22
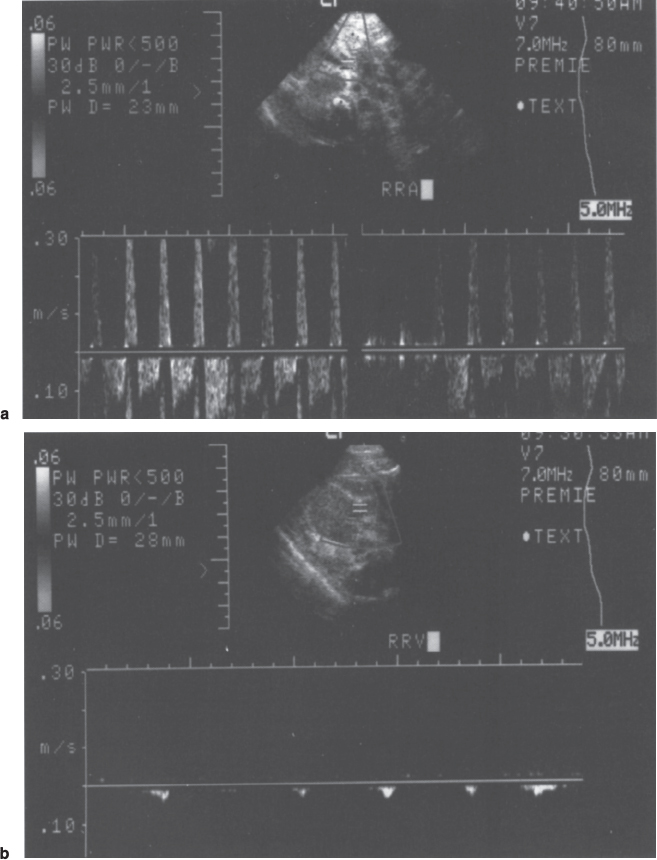
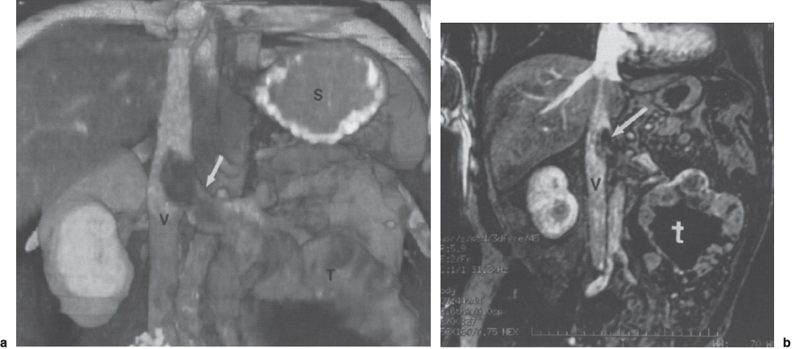
FIGURE 35–1. Right renal vein thrombosis in a premature infant with an elevated creatinine level, (a) Right renal artery was patent with positive Doppler signal. Note the reversal of diastolic flow within the artery on the Doppler spectrum. (b) Renal venous Doppler evaluation demonstrated respiratory artifact and no venous flow. Thrombus involving the inferior vena cava also was demonstrated (not shown).
Dehydration/polycythemia Shock Sepsis Asphyxia Gestational diabetes Traumatic delivery Sickle cell disease Seizure disorders Inherited thrombophilic disorders* |
*Protein C and S deficiency, antithrombin III deficiency, congenital inherited resistance to activated protein C.
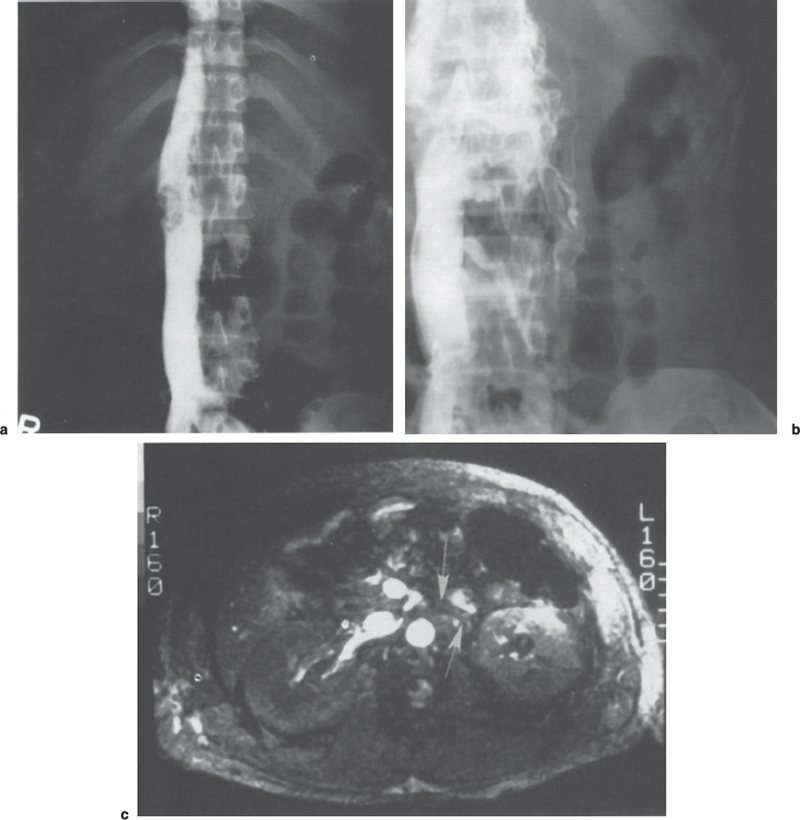
FIGURE 35–2. A 28-year-old woman with systemic lupus erythematosus and renal vein thrombosis. (a) The inferior vena cavagram demonstrates bilateral filling defects projecting into the inferior vena cava (IVC) lumen. (b) The selective left renal venogram demonstrates thrombosis of the left renal vein and collateral flow through the paravertebral plexus. (c) The axial magnetic resonance image (TR-22, TE-13) clearly demonstrates flow in the (shorter) right renal vein and lack of a flow signal (arrows) in the (longer) left renal vein.
 Nephrotic Syndrome
Nephrotic Syndrome
Because the NS is widely associated with RVT in both children and adults, a further discussion of the pathological processes is warranted. Injury to the glomeruli, which can occur from a host of insults, manifests itself as proteinuria, and although not all proteinuria is a result of a glomerluar injury, it is a rather sensitive indicator of gomerular damage.23 Some of the more common conditions resulting in glomerular injury, proteinuria, and the NS are shown in Table 35–2. The NS is characterized by severe proteinuria (>3.5g/24 hours/1.73m2), hypoproteinemia (in particular, hypoalbuminemia), edema, hyperlipidemia, and lipiduria. Proteinuria occurs as a direct result of the insult to the glomerular wall, which causes an increased permeability with protein loss into the urine; hypoproteinemia and edema are the consequences of excessive protein loss; and hyperlipidemia is secondary to the over synthesis of albumin by the liver in an effort to compensate for the lipiduria that occurs as a result of losses from the injured glomerular membrane.23
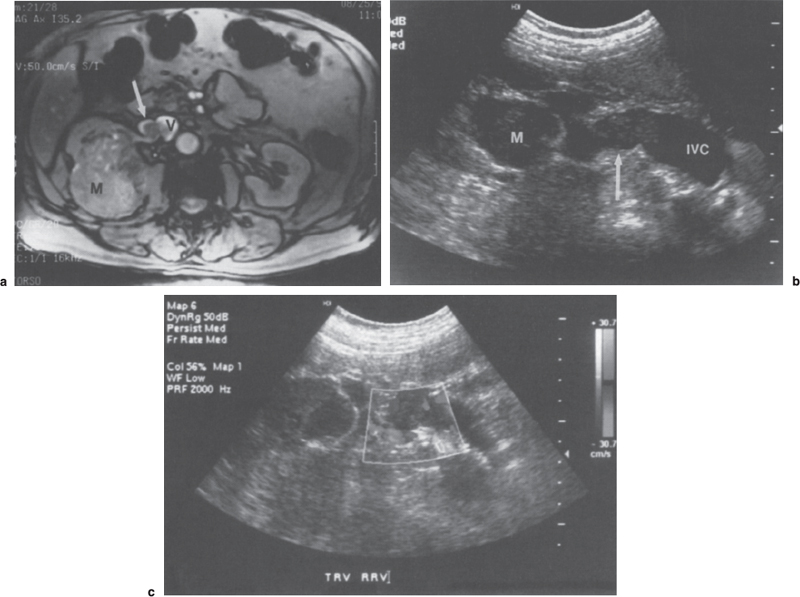
FIGURE 35–3. Right-sided renal cell carcinoma with venous extension of tumor, (a) Flow-sensitive axial magnetic resonance image shows renal mass (M) with tumor extension into the right renal vein (arrow) and inferior vena cava (V). (b) Transverse-oriented sonogram of same patient shows right renal mass (M). Tumor thrombus (arrow) shown as a low echogenicity mass within the renal vein with inferior vena cava extension. (c) Transverse sonogram demonstrates low echogenicity thrombus partially occluding the renal vein. Venous blood flow shown in blue (arrow) (renal mass, m; arterial flow, arrowhead).
Once thought to result in NS, RVT is now better understood to be the result of NS.14 Studies have shown that patients with NS have increased levels of factors V and VIII, fibrinogen, alpha-2 antiplasmin, alpha-2 microglobulin, and protein C and S. In addition, the platelet count, adhesiveness, and aggregation also are increased. Key components of the fibrinolytic system are concomitantly decreased including plasminogen, plasminogen activator, and antithrombin-III.14,23,27,28 Thrombotic extrarenal arterial events involving the mesenteric, brachial, and pulmonary arteries; bypass grafts; and left ventricle and aorta also have been reported.28–32 Extrarenal venous thromboses of the splenic vein, hepatic veins, adrenal veins, dural sinus, and iliac and pelvic veins likewise have occurred.5,25,27,28 Despite these significant changes mentioned in the coagulation system, no available tests allow for the prediction of thrombosis on the basis of alterations in any component(s) of the coagulation/fibrinolytic system.14 In summary, NS results not only in RVT, which may manifest itself as the presenting event, but potentially in widespread venous and arterial thromboses throughout the vascular system.