Retreatment after Radiotherapy: The Possibilities and the Perils
Of patients presenting at major cancer centers in the Western world, about 1 in 10 present with a second cancer. The following are the three major reasons for this:
Continued lifestyle—For example, factors associated with the first malignancy may continue to have an effect; smoking that caused a lung cancer may result later in a head and neck cancer, or alcohol that caused esophageal cancer may also result in a cancer of the tongue.
Genetic predisposition—Some syndromes, such as Li-Fraumeni syndrome, predispose to multiple primary tumors. This involves a very small proportion of the population, but it is incredibly important to the persons affected.
Treatment-related—Radiotherapy and/or chemotherapy can induce second malignancies. In the case of radiotherapy, most second cancers not only occur within or close to the treatment field, but also occur in remote locations, especially in radiogenic organs such as the lung. This is of particular importance in young children because they are 10 to 15 times as sensitive to radiation-induced malignancies as middle-aged adults are. For a second cancer to be considered as treatment-related, the latency must be appropriate, namely, short for a leukemia and long for a solid tumor.
For any of the previously mentioned reasons, it may be necessary to consider treatment to a tumor located in any area of the body that had previously been irradiated. Decisions regarding the safety of such retreatment are complex. For example, surgery may be compromised if the tissues involved had been previously irradiated to a high dose. The discussion here, however, focuses principally on the safety of reirradiation of an area of normal tissue previously exposed to radiation. Information on this subject is far from complete, but certain general principles emerge from experimental and clinical experience. One thing is clear, namely, that if the radiation tolerance of a given organ or tissue has been exceeded by the initial treatment, to the extent that function is lost or is in the process of being lost, then subsequent retreatment cannot be contemplated with safety. By contrast, if the initial treatment is below the tolerance of the organ or tissue exposed, then some retreatment at a later date is safe, varying very much with the organ or tissue involved and depending on several other factors.
When considering retreatment with radiation, whether it is intended to be either curative or palliative, several factors must be taken into account:
The dose and volume treated during the initial radiotherapy and the extent to which the retreatment fields overlap with the initial fields
Whether chemotherapy was added to the initial radiotherapy
The time interval that has elapsed since the initial radiotherapy
The tissues and organs involved because they differ markedly in their ability to recover
Highly conformal techniques, such as stereotactic radiosurgery, stereotactic body radiotherapy (SBRT), or brachytherapy, are most appropriate.
Whether there are alternative options to radiation that could be considered
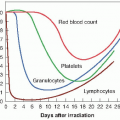
▪ EARLY- AND LATE-RESPONDING TISSUES
Early-responding tissues are usually self-renewing tissues and are characterized by a rapidly proliferating stem cell compartment that provides cells to differentiate and become the mature functioning cells. If some stem cells survive within the irradiated volume, or if undamaged stem cells can migrate into the irradiated volume from outside, the tissue architecture may be partially or completely restored. Consequently, rapidly proliferating tissues generally recover well from the initial radiotherapy and will tolerate reirradiation to almost full doses, provided sufficient time is allowed.
By contrast, most late-responding tissues are much less able to tolerate retreatment because they do not have the ability to recover from the initial damage inasmuch as they do not have a rapidly proliferating stem cell compartment. Some slowly proliferating tissues are capable of partial proliferative and functional recovery, although this takes months and some residual damage remains.
▪ PRECLINICAL DATA
Experiments with rodents show that radiationinduced skin damage can recover well, with restoration of almost full radiation tolerance. As would be expected, recovery occurs quickly after low doses, but more slowly as the initial dose is increased. Using hind limb deformation as an endpoint, representing late subcutaneous fibrosis, much poorer retreatment tolerance was observed than for the early skin reaction. Preclinical data also show that retreatment with reduced doses is possible in both lung and spinal cord after an interval of 3 to 6 months. There is a plethora of data for the spinal cord in animals ranging from rodents to rhesus monkeys. The experiments with monkeys demonstrated a large capacity for the spinal cord to recover from occult radiation injury induced by a commonly prescribed elective dose (44 Gy in 2 Gy fractions) in that only 4 of 45 monkeys developed myeloparesis following a retreatment with 57.2 to 66 Gy given 1 to 3 years after the initial therapy.
Other slowly proliferating organs, such as the kidney or bladder, do not appear to be capable of recovery from late functional damage even after lower subtolerance doses.
▪ CLINICAL STUDIES
Clinical radiation oncologists are, quite rightly, reluctant to transfer quantitative reirradiation data from animals (especially rodents) to humans, although the general principles and lessons, particularly the big difference between different organs and tissues, are probably applicable.
Unfortunately, the clinical data available are sketchy to say the least. In most cases, the number of patients is small, collected over a long period, with changing radiotherapy techniques (dose, fractionation pattern, etc.), and with no detailed outcome of a matched control group of patients who had received the same initial therapy, but not the retreatment.
Clinical review papers are beginning to express data in terms of the biologically effective dose (BED), calculated on the basis of the linearquadratic model, using an α/β of 10 for earlyresponding tissues and 3 for late-responding tissues. This is a good first step, but unconventional fractionation patterns are often used for retreatment schedules, particularly in a palliative setting, it would be necessary to convert the BED values obtained to an equivalent BED calculated for a 2 Gy per fraction schedule if different experiences are to be compared. Unfortunately, such complete data are seldom available.
Spinal Cord
The spinal cord is a major dose-limiting organ in the treatment of primary tumors of the spinal cord or of neoplastic disease in the direct vicinity of the cord. When initial radiation therapy is delivered in conventional 2 Gy per day fractions, the consensus is that the incidence of myelopathy is less than 1% for total doses of 50 to 55 Gy, and up to 5% for total doses of 55 to 60 Gy. The published clinical data on reirradiation suggest that there is a substantial recovery, provided the initial treatment did not exceed about 90% of the acceptable BED and that there was a time interval of a year or more between the initial and subsequent treatments. The data suggest an important threshold of a cumulative BED of 130% to 135% of the acceptable BED in a single course of therapy (calculated with an appropriate α/β ratio of about 3). The reader is referred to the appropriate review papers (Grosu et al., 2002; Nieder et al., 2000) for more details, but the overall conclusion is that it is not possible
to suggest more detailed recommendations concerning the optimal total dose and fraction size to result in the maximal palliative effects accomplished by minimal side effects.
to suggest more detailed recommendations concerning the optimal total dose and fraction size to result in the maximal palliative effects accomplished by minimal side effects.
There are two later reports of the use of SBRT for the salvage therapy of patients with prior radiation of spinal metastases (Nelson et al., 2009; Sahgal et al., 2009). The development of this highly conformal treatment makes it possible to give a dose of approximately 24 Gy in about three fractions, without unacceptable toxicity. The authors conclude that SBRT is both safe and effective in the palliative/retreatment setting.
In summary, the clinical data, although minimal, do not contradict the more detailed data available from primate studies, which suggest that retreatment is a real possibility in this site.
Brain
There are no animal data available on the reirradiation tolerance of the brain. It might be thought that information derived from studies of the spinal cord could be transferred to the brain, but the available clinical studies indicate that this is not the case, at least, in regard to the influence of the time interval between initial treatment and reirradiation.
The most recent overview of currently available clinical data on reirradiation of the brain comes from studies of the treatment of recurrent glioma (Mayer & Sminia, 2008). For conventional radiotherapy techniques, radiationinduced normal brain tissue necrosis was found when the cumulative BED (i.e., the sum of the BEDs from both the initial treatment and reirradiation) exceeded 100 Gy. In most cases, the initial treatment consisted of a standard regimen of 60 Gy in 2 Gy fractions. The BED was calculated using the linear-quadratic formalism, employing an α/β ratio of 2 Gy and normalized to 2 Gy fractions because the literature contains several reirradiation schemes with regard to total dose and fraction size. There was no correlation between the time interval between the initial and reirradiation course and the incidence of radionecrosis. When more conformal techniques were employed, such as fractionated stereotactic radiosurgery, higher retreatment doses were possible without increasing the probability of normal brain tissue necrosis.
The Radiation Therapy Oncology Group Protocol 90-95 studied 156 patients with recurrent previously irradiated primary brain tumors and brain metastases, retreated with single fraction radiosurgery. They found that the maximum tolerated doses were 24 Gy, 18 Gy, and 15 Gy for tumors less than or equal to 20 mm, 21-30 mm, and 31-40 mm in diameter, respectively. Unacceptable central nervous system toxicity was more likely in patients with larger tumors, whereas local tumor control was most dependent on the type of recurrent tumor and the treatment unit used (linac versus Gamma Knife).
Head and Neck
Despite significant improvements in outcome for head and neck squamous cell carcinoma treated aggressively by modern techniques, the major pattern of failure continues to be locoregional recurrence. There is no consensus on the best way to handle this problem and, as a result, there is a wide variation in the approaches used. There have been several reviews in recent years (Chopra et al., 2006; DeCrevoiser et al., 1998; Kasperts et al., 2005; Lee et al., 2007; Salama et al., 2006; Wong, 2006). Radical reirradiation with doses of 50 to 60 Gy, either definitive or postoperative, does improve locoregional control and possibly improves survival, whereas lower doses are ineffective. However, reirradiation with such potentially curative doses within a few years of a similar initial treatment is associated with severe toxicity and functional sequelae, as well as a small but nonnegligible incidence of treatment-related deaths. The most recent review by Sulman et al. (2009) reported on the use of intensity-modulated radiation therapy (IMRT) to retreat recurrent head and neck cancer and came to the same general conclusion except that the treatment-related morbidity, although significant, may have been less than in previously published reports using conventional techniques. In this case, the median time interval between initial radiation and retreatment was almost 4 years, and the median lifetime dose was 116.1 Gy.