Fig. 13.1
Leiomyoma. The tumor is gray-white and its cut surface has a whorled appearance. This lesion was identified immediately adjacent to the prostate and was clinically indistinguishable from malignancy, prompting excision (From MacLennan and Cheng (2011), with permission)
Imaging
Ultrasound
Typically appears as a small mass in the pelvis; more common in females.
It is hypoechoic and has a homogeneous inner pattern.
Computed Tomography
The density of the tumor varies according to the inner structure.
Purely cystic to solid masses have been reported. The tumor may also contain hemorrhage.
Magnetic Resonance Imaging
The signal intensity on the T1-weighted image is mostly isointense relative to the adjacent muscle. It is hyperintense on T2-weighted images. The signal intensity increases in relation to the extent of myxoid change in the stroma. Hypointense streaks within the mass on the fat-saturated T2-weighted images have been reported.
It shows strong enhancement after contrast material administration.
Pathology
Leiomyosarcoma
General Information
Leiomyosarcoma is the second most common sarcoma of the retroperitoneum.
Most patients are more than 50 years old, and the majority are female.
Leiomyosarcoma can also originate from the renal capsule, renal vein, or the inferior vena cava (IVC). It is the most common malignant tumor of the IVC.
Imaging
Intravenous Pyelography (IVP)
IVP demonstrates displacement of retroperitoneal organs or of gas within the lumen of retroperitoneal portions of the intestines (ascending and descending colon).
Observation of a well-defined fat plane between the mass and the displaced kidney helps to confirm the extrarenal location of the mass. If the mass is caudal to the kidney, the retroperitoneal origin of the mass is more reliably ascertained.
Renal dysfunction is uncommon but may be secondary to severe long-standing ureteral obstruction caused by the mass.
Barium Enema
May be helpful in mass localization if there is displacement of retroperitoneal portions of the bowel.
If there is secondary bowel invasion, distinction between a bowel primary and invasion by extrinsic cancer is difficult.
Ultrasound
The tumor appears as a solid, hypoechoic mass with well-defined margins. It has a heterogeneous echo texture and often contains cystic spaces and irregular walls.
Necrotic areas may be evident.
Intraluminal localization of the tumor suggests leiomyosarcoma of IVC origin. Color flow Doppler is more useful in this case.
Ultrasound is the imaging modality of choice for successful image-guided biopsy.
Computed Tomography
Leiomyosarcoma appears as a large, solid, lobular, nonfatty mass with clear outlines on CT images. It is easily distinguished from adjacent structures. Organs next to the mass are usually displaced, whereas native retroperitoneal structures are invaded directly (Fig. 13.2a, b).
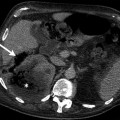
Fig. 13.2
Leiomyosarcoma in a 68-year-old man. (a) Contrast-enhanced CT scan reveals a large mass adjacent to the right kidney that displaces the kidney, liver, and pancreas. The mass has heterogeneous enhancement with central nonenhancing foci that correspond to necrosis. The tumor has some fatty components at the center. (b) Leiomyosarcoma. A large fleshy bulging tumor with an extensively necrotic and hemorrhagic central aspect displaces and compresses the adjacent kidney (Image courtesy of Francisco Paras, M.D.). (c) Angiography performed for the embolization of the tumor shown in (a) confirms the hypervascularity of the mass. Selective angiography shows the feeding arteries (arrow) of the tumor in detail
Necrosis and calcifications in the tumor may be evident.
CT angiography may help to verify retroperitoneal vessel invasion. A mass with intraluminal and extraluminal components is highly suggestive of IVC leiomyosarcoma.
Dilatation of the IVC by a solid mass that shows irregular enhancement and obstruction of the IVC is typical of intravascular leiomyosarcoma. Optimal contrast study is necessary for a complete evaluation.
Magnetic Resonance Imaging
Leiomyosarcoma appears as a large, solid mass with an average diameter of 15 cm. It is usually hypointense in T1-weighted images and hyperintense in T2-weighted images.
Tumor enhances heterogeneously after contrast injection.
Presence of necrosis and hemorrhage is indicative of malignancy.
MRI is useful in determining vascular patency and invasion of adjacent organs.
Tumors originating from the upper segments of IVC may cause a secondary Budd-Chiari syndrome or may result in development of a thrombus in the renal vein. If the involvement is in the lower segments, edema in the lower extremities is inevitable.
Angiography
Most retroperitoneal leiomyosarcomas are hypervascular or moderately vascular and receive blood supply from more than one artery (Fig. 13.2c). Areas of tumor necrosis demonstrate an avascular center surrounded by a thick hypervascular rim.
Venography may be helpful in evaluating intraluminal leiomyosarcoma. Two-view interpretation is essential. Small masses appear as irregular filling defects. Thrombus enlarges the vascular lumen and obstructs the IVC and its branches. Collateral veins are observed.
Differential Diagnosis
Retroperitoneal leiomyosarcoma is characteristically large, nonfatty, and extensively necrotic, with a propensity for intravascular extensions. However, tumor invasion of the IVC is also seen in cancers of the kidney, adrenal, liver, and uterus.
Liposarcoma is a common retroperitoneal sarcoma; however, its fat content is distinctive. Malignant fibrous histiocytoma is difficult to distinguish radiologically from leiomyosarcoma. Lymphoma tends to envelop the IVC and aorta, but typically shows less necrosis than leiomyosarcoma.
Pearls and Pitfalls
Contrast enhancement in leiomyosarcoma usually occurs in the late phase. This feature is used to differentiate the lesion from the other hypervascular retroperitoneal tumors.
In some cases leiomyosarcoma is extensively cystic, making it hard to distinguish radiologically from other cystic retroperitoneal tumors.
In some cases there is discordance between CT and ultrasound findings. The CT findings may suggest the presence of large areas of necrosis which appear solid on sonograms. These areas represent non-liquefied necrotic or avascular regions of the tumor.
Tumors of Skeletal Muscle
Rhabdomyosarcoma
General Information
Rhabdomyosarcoma is a malignant neoplasm that shows evidence of skeletal muscle (sarcomeric) differentiation. Nonetheless, it may arise in areas where striated muscle is normally absent, such as the common bile duct or urinary bladder, or sparse, such as the nasal cavity, the middle ear, or vagina. It most commonly occurs in infants and children, with a lesser incidence in adolescents and young adults. Its incidence in various anatomic regions is approximately as follows: head and neck, 35 %; genitourinary sites, 25 %; and extremities and other sites, 40 %. Only 5 % of rhabdomyosarcomas are located in the retroperitoneum.
Imaging
Ultrasound
Rhabdomyosarcoma appears as a solid, well-circumscribed, lobular, hyperechoic mass on ultrasound examination. Color flow Doppler ultrasound demonstrates a highly vascular mass.
Computed Tomography
The density of rhabdomyosarcoma is identical to that of skeletal muscle (Fig. 13.3a, b), and consequently it may be difficult to distinguish on non-enhanced CT scans.
Fig. 13.3
Rhabdomyosarcoma. Axial (a) and sagittal (b) contrast-enhanced CT images demonstrate retroperitoneal mass (arrows) with mild contrast enhancement. This mass invades left paravertebral soft tissues
After contrast material injection, areas of central necrosis manifest more precisely.
Magnetic Resonance Imaging
Rhabdomyosarcoma exhibits medium signal intensity on T1-weighted images and high signal intensity on T2-weighted images (Fig. 13.3c).
Signal intensity and the homogeneity of the tumor vary according to the presence and the amount of necrosis. Necrotic areas are identified more clearly after the contrast material administration.
Pathology
Differential Diagnosis
If the patient is a child the differential diagnosis, depending upon the location of the tumor, may include such diverse conditions as hydrometrocolpos, neuroblastoma, and teratoma.
In adults, the differential includes other soft tissue tumors, both benign and malignant, such as leiomyoma, leiomyosarcoma, and malignant fibrous histiocytoma.
Tumors of Adipose Tissue
Lipoma
General Information
Retroperitoneal lipomas are benign encapsulated tumors composed of normal adipose tissue.
Most occur in the perirenal area.
Imaging
Computed Tomography
Lipomas are the most common benign tumors of the retroperitoneum.
Encapsulated mass with the appearance of fat tissue.
Density measurements yield density less than or equal to that of normal fat.
Imaging
Computed Tomography
CT reveals a well-defined mass with homogeneous appearance and fat density.
Magnetic Resonance Imaging
Lipomas are bright on T1-weighted sequences and show loss of signal with fat suppression.
No enhancement occurs after intravenous contrast administration.
Lipoblastoma
General Information
Lipoblastomas are derived from fetal adipose tissue. They are composed of adipocytes and lipoblasts. They are encountered almost exclusively in infants and young children.
Lipoblastoma usually forms a circumscribed mass, but some have a diffuse distribution, crossing tissue planes, in which case the lesion is designated lipoblastomatosis.
Occurrence of lipoblastoma in the retroperitoneum is extraordinarily rare.
Imaging
Computed Tomography
Well-defined fat-containing lesion with multiple thick septa. They demonstrate contrast enhancement.
Magnetic Resonance Imaging
Lipoblastomas appear on T1-weighted images with the signal intensity less than the adjacent subcutaneous fat.
T2-weighted images demonstrate intermediate to high signal intensity within the mass.
Patchy contrast enhancement occurs on contrast-enhanced images.
Liposarcoma
General Information
Liposarcoma is the commonest type of retroperitoneal sarcoma, followed in incidence by leiomyosarcoma and malignant fibrous histiocytoma. Males and females are affected with approximately equal frequency, with a peak prevalence in the sixth and seventh decades.
Retroperitoneal liposarcomas are generally large at presentation; nearly half are larger than 20 cm at the time of diagnosis.
Well-differentiated liposarcoma (WDL) is a low-grade cancer that essentially does not metastasize, but because it is typically deeply located and often very large when first diagnosed, it is technically difficult to resect completely and tends to recur locally, with reported recurrence rates as high as 91 %.
Dedifferentiation in a WDL is characterized by the presence of a component of high-grade nonlipogenic sarcoma. It occurs in about 10–15 % of well-differentiated liposarcomas. In the great majority of cases, the histologic appearance of the dedifferentiated component is simply that of a high-grade sarcoma, raising the intriguing possibility that the majority of cases of so-called malignant fibrous histiocytomas occurring in the retroperitoneum actually represent dedifferentiated liposarcomas.
The extent and grade of dedifferentiation do not influence prognosis. Cancer-related death is related to local effects of the tumor rather than the adverse effects of distant metastases.
Imaging
Ultrasound
Ultrasound plays a limited role. It can be used to define the extent of the tumor. Early recurrence is also detected by frequent ultrasound follow-ups.
Liposarcomas may appear hyperechoic on ultrasound (Fig. 13.4a). Due to the fibrous septa of the tumor, ultrasound images may show hyperechoic horizontal or concentric lines.
Fig. 13.4
Liposarcoma. (a) Gray-scale ultrasound reveals a hypoechoic mass (arrow) adjacent to the left kidney. (b) The intrinsically normal native kidney is dwarfed and compressed by a large liposarcoma surrounding it. (c) Axial-unenhanced CT demonstrates a large soft tissue density mass (arrow) with minimal calicification arising from left side of retroperitoneum. Axial (d) and coronal (e) contrast-enhanced CT images reveal heterogeneous contrast enhancement within the mass. The mass invades the ipsilateral kidney. (f) Liposarcoma in a 75-year-old woman. CT scan reveals a large mass with hypodense areas secondary to necrosis. (g) T2-weighted MRI demonstrates the necrotic and cystic components. (h) In post-contrast MR image enhancement of the solid components can be seen
Color flow Doppler ultrasound may show some compressed vessels inside the tumor, but this is not specific for the diagnosis.
Computed Tomography
CT images exhibit a large, enhancing, solid, inhomogeneous, poorly defined, infiltrating mass that usually displaces adjacent organs (Fig. 13.4b). The mass has negative attenuation and may have internal septa (Fig. 13.4c–e).
A mixed-pattern tumor with foci of fat interspersed in high-attenuating tissue.
A pseudocystic water-density tumor.
Calcification is detectable in as many as 12 % of the tumors.
Tumor homogeneity diminishes as the degree of dedifferentiation increases.
Magnetic Resonance Imaging
In well-differentiated tumors the mass shows identical signal intensity with the subcutaneous fat tissue in all sequences (Fig. 13.4f, g).
The mass has a thick peripheral rim and contains hypointense linear septa in T1-weighted images.
Gadolinium enhancement can be seen after contrast administration (Fig. 13.4h). However, the majority of liposarcomas are hypovascular and do not enhance. Fat-suppressed T1 sequences are useful to appreciate the minimal contrast enhancement.
Tumor homogeneity, which is dependent upon the amount of WDL present in the lesion, diminishes as the degree of dedifferentiation increases. This results in related signal changes in different MR sequences.
Angiography
Liposarcomas are usually hypovascular to moderately vascular, and they cause displacement of the major vessels, particularly the inferior vena cava.
Moderately hypervascular liposarcomas may show irregular, fine tumor vessels and areas of tumor stain. Venous filling may occur early, and the veins may be dilated and tortuous.
Angiography may be useful for preoperative planning, intra-arterial infusion, and/or transcatheter embolization.
Nuclear Medicine
Gallium-67 (67Ga) citrate scintigraphy scanning is positive in 75–80 % of patients with malignant soft tissue tumors. It can be used to distinguish liposarcoma from lipoma.
67Ga scanning may also have a role in imaging liposarcoma recurrence.
Thallium-201 (201Tl) chloride was reported a radionuclide sensitivity of 81 %, which is higher than that of 67Ga imaging (68.8 %).
Differential Diagnosis
Malignant fibrous histiocytoma, leiomyosarcoma, and desmoid tumors may have an appearance that is indistinguishable from that of liposarcoma.
Pearls and Pitfalls
Liposarcoma may be difficult in some cases to distinguish from renal angiomyolipoma. In contrast to renal angiomyolipoma, liposarcoma compresses the kidney without any renal tissue defect or other fat-containing renal lesions and lacks internal vascularity.
Liposarcomas with richly myxoid stroma may be misdiagnosed as cystic lesion.
Pathology
Descriptions of the pathologic findings and representative images of liposarcoma are shown in Figs. 5.11 and 5.12.
Pelvic Lipomatosis
General Information
Pelvic lipomatosis is characterized by overgrowth of histologically benign, mature fat along perirectal and perivesical spaces of the pelvis.
Small amount of inflammation and fibrosis may be noted within the fat.
Males are more frequently affected than females (M/F: 10/1).
Presenting symptoms include urinary tract symptoms (dysuria, hematuria, urgency), gastrointestinal tract symptoms (constipation, nausea, and vomiting), lower abdominal pain, backache, and flank pain.
Imaging
Cystogram
The bladder is displaced superiorly and anteriorly.
A classic finding in pelvic lipomatosis is a “pear-shaped” or “inverted drop” bladder representing symmetric compression of the bladder. A pear-shaped bladder can also be seen in pelvic hematoma and pelvic lymphadenopathies.
Intravenous Pyelography
Medial deviation of both distal ureters may be observed on IVP.
Compression of ureters may result in hydroureteronephrosis.
Barium Enema
The appearance of elongated and straightened rectum with superior displacement of the distal sigmoid colon suggests pelvic lipomatosis.
Computed Tomography
CT demonstrates increased amount of symmetrically distributed fat.
No discrete soft tissue mass is evident.
Contrast-enhanced CT reveals no enhancement in pelvic lipomatosis.
Magnetic Resonance Imaging
Pelvic lipomatosis manifests with signal intensity of fat on T1- and T2-weighted images.
Fibrous strands appear hypointense on both T1- and T2-weighted images.
Hibernoma
General Information
Hibernomas are rare benign indolent neoplasms that develop most commonly in adults between 20 and 50 years of age from the remnants of fetal brown adipose tissue, a specialized form of fat found in hibernating and nonhibernating animals, including humans.
Most arise in muscle and subcutaneous tissue, most commonly in the thigh, shoulder, back , neck, chest, arm, and abdominal cavity/retroperitoneum.
They are typically reported to be tan-brown, lobulated, and well encapsulated, but they may infiltrate adjacent structures, especially striated muscle.
Imaging
Ultrasound
Hibernoma usually appears on ultrasound as an echogenic heterogeneous mass with increased vascularity.
Computed Tomography
Computed tomography reveals a low-attenuation, well-defined lesion with intratumoral septa (Fig. 13.5a, b).

Fig. 13.5
Hibernoma. (a) Axial CT scan of the abdomen with venous contrast enhancement. The white arrowhead demonstrates a 3.3-, 2.0-, 1.5-cm nonenhancing lesion inferior to the right renal hilum and lateral to the vena cava. The black arrow indicates the vena cava and the black arrowhead indicates the ureter. (b) Coronal CT scan of the abdomen with venous contrast enhancement. The white arrowhead indicates the same mass described in (a). The black arrow indicates the vena cava and the black arrowhead indicates the ureter (With permission from Yohannan et al. (2011))
Contrast-enhanced CT demonstrates contrast enhancement in septa of the lesion. Enhancement of the whole mass may also be observed.
Magnetic Resonance Imaging
Hibernomas appear hypointense relative to subcutaneous fat on T1-weighted images. T2-weighted images reveal variable intensity.
Positron Emission Tomography
PET can distinguish hibernomas from other fat-containing lesions because hibernomas use large amounts of glucose to generate heat.
Myelolipoma
General Information
Myelolipomas mainly occur in adrenal glands. Extra-adrenal myelolipomas are rare retroperitoneal tumors composed of mature adipose cells and hematopoietic tissue.
They are usually asymptomatic, but large myelolipomas may present with hemorrhage.
Imaging
Ultrasound
Myelolipomas appear as hyperechoic masses with hypoechoic components. Ultrasound appearance varies according to the relative amounts of myeloid and adipose tissue in the tumor.
Color flow Doppler reveals vascular flow.
Computed Tomography
Well-defined lesion with fat and soft tissue density.
Calcification may occur in 10 % of myelolipomas.
Magnetic Resonance Imaging
Myeloid elements of myelolipomas demonstrate low signal intensity on T1-weighted images and intermediate signal intensity on T2-weighted images.
Pathology
Descriptions of the pathologic findings and representative images of myelolipoma are shown in Figs. 11.11 and 11.12.
Angiomyolipoma
General Information
Angiomyolipomas are composed of blood vessels, smooth muscle cells, and fat cells.
Rarely, angiomyolipoma may arise as a retroperitoneal mass separate from other organs where it may typically arise, such as the kidney or liver.
Imaging
Ultrasound
Well-defined mass with hyperechoic appearance
Computed Tomography
Angiomyolipomas present as low-attenuation mass with a fat component.
Large vessels may be visualized coursing through the mass.
Magnetic Resonance Imaging
MRI features depend on the fat content of the mass. Fat saturation images reveal signal loss.
Pathology
Descriptions of the pathologic findings and representative images of angiomyolipoma are shown in Chap. 1 (Renal Neoplasms, Figs. 1.11 and 1.12) in Vol. I.
Neural and Neuroendocrine Tumors
Ganglioneuroma
General Information
This is a benign neural neoplasm that arises from cells of the embryonal sympathetic nervous system.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree