In most countries, critical limb ischemia (CLI) has an incidence estimated to be 50 to 100 per 100,000 every year. CLI has a high mortality and morbidity rate and consumes important health and social care resources. , Aging of the population, increasing incidence of diabetes and renal failure, and limitations in the ability to reduce tobacco consumption explain the high likelihood of increased incidence in the near future. Treatment options include amputation, surgical or endovascular revascularization, and novel techniques of arteriogenesis or angiogenesis using stem cell or gene transfer. Amputation should be avoided as much as possible because it carries its own risk of complications and increased mortality.
Bypass surgery requires good-quality saphenous veins (not always present) and routine ultrasound-guided graft surveillance. The optimal approach should be selected according to multidisciplinary consensus and is generally based on local and general clinical factors, high-quality anatomic workup, and experience. As stated in the Trans-Atlantic Inter-Society Consensus (TASC) document in 2000 and confirmed by the recent results of the Bypass Versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial, the endovascular approach is generally regarded as the initial treatment of choice.
Indications
Based on current evidence, the indication for below-the-knee (BTK) angioplasty is limited to patients presenting with chronic CLI as defined in the TASC consensus document. Indications for BTK angioplasty are based on clinical assessment of the patient and evaluation of the extent of arterial disease. Revascularization is the only method that will prevent amputation and prolong life. These patients are at high risk for limb loss and other vascular events like stroke and myocardial infarction. Studies have shown that 25% of patients who cannot be revascularized will die within 1 year after the initial diagnosis of CLI. ,
Clinical examination should follow a sequential approach: (1) documentation of the quality of lower limb pulses, (2) assessment of the skin surface and ankle pressures (should include toe pressure in diabetic patients [critical level < 50 mm Hg], and (3) overall evaluation of the patient’s general status (renal function and cardiac and carotid evaluation). Also important is the patient’s social environment because chronic care will be needed in all cases. An appropriate link to a postoperative care network to ensure appropriate global management and nursing is key to optimal clinical management.
Next is appropriate imaging, which should be performed by well-trained radiologic personnel in a hospital environment.
With the endovascular approach, many patients can have successful reestablishment of improved flow down to the foot and healing of any ulcers. Stents may improve the results of angioplasty, but an important breakthrough has been the use of subintimal recanalization, which dramatically increases the number of patients who can be helped by the endovascular approach.
Contraindications
Contraindications to revascularization are rare. This is because endovascular techniques are less invasive and can be undertaken in patients who cannot undergo open repair. However, a patent distal vessel (whether in the lower leg or foot) is an essential prerequisite before an attempt at revascularization should be considered. In patients with CLI who have no patent distal target vessel to justify an attempt at recanalization, work is ongoing looking at the potential for other methods to improve distal arterial perfusion, such as angiogenesis using stem cell therapy or gene transfer. However, beneficial results from clinical evaluation in patients are awaited.
In patients with distal limb infection, urgent amputation should be performed to avoid septicemia and other systemic complications.
Equipment
Imaging
Both noninvasive and invasive imaging techniques are of utmost importance before considering an endovascular or surgical approach.
The initial workup should be by color duplex ultrasound imaging, which can provide (in expert hands) essential anatomic and hemodynamic information. However, the results of duplex ultrasound are variable at the BTK level, so for evaluation of the BTK circulation, many centers use computed tomographic angiography (CTA) or magnetic resonance angiography (MRA).
MRA has several advantages that are well recognized, but it is limited by the possibility of claustrophobia and other well-known contraindications. MRA for the demonstration of BTK lesions has a sensitivity of about 93%, and with recent technical refinements (venous occlusion cuff, parallel imaging), the results should further improve. ,
Multidetector CTA is now rivaling digital subtraction angiography (DSA) in the quality of imaging sensitivity and specificity. Multidetector CTA requires iodinated contrast medium, but careful hydration can overcome most of the problems related to nephrotoxicity. A significant limitation is analysis of small and calcified vessels. The results of high-quality MRA and CTA for the diagnosis of BTK disease are broadly comparable.
The gold standard for imaging BTK circulation is DSA, which has become easier to perform thanks to the development of smaller-caliber diagnostic catheters and less-toxic iodinated contrast media. A unifemoral approach, where only the ipsilateral femoral artery is punctured and subsequent angiography limited to the symptomatic leg, requires substantially less contrast medium than required for classic bilateral angiography. Patients taking metformin or other biguanides should undergo interruption of these medications for at least 48 hours after DSA, with reintroduction only after verification of unimpaired creatinine clearance (European Society of Urological Radiology guidelines). In practice, puncture of the ipsilateral common femoral artery (CFA) with a Teflon needle and injection of less than 60 mL of a contrast agent can provide adequate images of the lower limb arterial supply. Delayed images with selective injections, appropriate pixel shifting, and masking are also key elements to allow high-quality images.
Endovascular Revascularization
The following equipment is needed for endovascular revascularization.
- •
Arterial puncture needle
- •
Metallic 18-gauge needle
- •
Teflon 18-gauge needle
- •
21-gauge micropuncture needle
- •
- •
Catheters
- •
To assist in the crossover technique: pigtail or Cobra, sometimes internal mammary catheter
- •
To assist in catheterizing the origin of the superficial femoral artery (SFA): any catheter with an angulated tip (e.g., Bolia Minicath [Terumo Medical Corp., Somerset, NJ], Vanshi 2 or 3 [Cook Medical, Bloomington, IN] Van Andel catheter for subintimal use [Cook Medical])
- •
- •
Sheath
- •
Antegrade approach: 4F or 6F (Terumo): 10, 25, or 40 cm long
- •
Crossover: First choice is KSAW-5.0 (Cook Medical) with a removable Y-connector that can be replaced with a hemostatic valve. The Shuttle-SL flexor sheath (up to 80 cm) (Cook Medical) is also useful, as is the Destination sheath 5F to 6F (Terumo).
- •
- •
Guidewires
- •
Intraluminal recanalization: First choice is the Pilot 200 (Abbott Vascular, Santa Clara, CA). Other dedicated 0.014-inch wires such as the Approach CTO guidewire (Cook Medical), Winn (Abbott Vascular), and V14 (Boston Scientific, Natick, MA). Coronary chronic total occlusion 0.014-inch wires such as PT Graphix (Boston Scientific) and Choice PT (Boston Scientific) can be helpful in selected cases.
- •
Subintimal recanalization: hydrophilic 0.035-inch J and straight (stiff in some cases) (Terumo) and previously mentioned 0.014-inch wires advanced in a loop shape.
- •
0.014-inch wires for calcified occlusions (Cross-it [Abbott Laboratories, Abbott Park, IL]; Pilot intermediate [Guidant, Santa Ana, CA]).
- •
- •
Contrast media (low-osmolar contrast media preferred because of frequent renal failure in these patients): Xenetix 320 (Roissy, France) or Visipaque 320 (GE Healthcare, Princeton, NJ).
- •
Balloons
- •
0.014- or 0.018-inch coaxial balloons are preferable because they allow better crossability of calcified lesions (lower profile). Small (1.25- or 2-mm) balloons can be used to predilate difficult lesions. Short coronary balloons have better lesion crossability (Ryujin [Terumo]).
- •
0.035-inch balloons are preferred in subintimal angioplasty because they provide better pushability and allow progressive dilation by very short iterative inflation/deflation.
- •
High-pressure (up to 30 atm) balloons (Dorado [Bard Peripheral Vascular, Tempe, AZ]) are useful to overcome recoil in subintimal recanalization.
- •
0.035-inch ReKross Catheter (Bard) is useful in a very tight subintimal space.
- •
- •
Stents
- •
Self-expandable dedicated stents: Xpert (Abbott Vascular) self-expandable thin-strut Nitinol stent, Maris Deep (Medtronic Inc., Minneapolis, MN) thin-strut Nitinol stent, Astron Pulsar (Biotronik, Bulack, Switzerland)
- •
Coronary balloon-expandable stents: PRO-Kinetic explorer (Biotronik, Berlin, Germany), cobalt chromium and passive coating (silicon carbide), diameter 2.0 to 5.0 mm, length 8 to 40 mm
- •
Dedicated balloon-expandable stents: Chromis Deep (Medtronic) cobalt chromium stent up to 8 cm in length, Inperia (Maquet, Orleans, France [not available in the United States])
- •
Technique
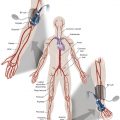
Anatomy and Approaches
In general, when performing BTK interventions, the ipsilateral antegrade approach should be used to enable direct access to the BTK circulation. According to the level of bifurcation of the CFA, antegrade puncture may be easy or difficult. When the CFA is short or the patient is obese, antegrade puncture may be technically challenging. Ultrasound-guided puncture is useful to enable successful and rapid antegrade femoral artery puncture. In obese patients or if the common femoral bifurcation is high, the SFA can be punctured directly. A contralateral technique is rarely required.
When popliteal puncture is considered, ultrasound guidance is mandatory, and one should remember the relationship of the artery to the nerves in the popliteal fossa.
Technical Aspects
Heparin should be administered (70 units/kg) intraarterially after arterial puncture. A vasodilator should also be administered to prevent spasm in the BTK arteries (e.g., tolazoline in 5-mg doses intraarterially, up to 10–15 mg, glyceryl trinitrate in 100-μg bolus injections).
After the intervention, all patients should be treated with aspirin (75–125 mg/day) and clopidogrel (300-mg loading dose and 75 mg/day thereafter until healing of the ulcer or until the relief of rest pain).
Analgesia should be administered during the procedure for patient comfort, to reduce limb movement and thereby enhance the chance of technical success. General anesthesia is seldom required but may be used for noncompliant patients.
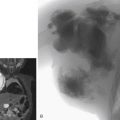
The usual technique can be summarized in the following steps: arterial puncture, sheath insertion, crossing the lesion with a hydrophilic guidewire, percutaneous transluminal angioplasty (PTA), withdrawal of the balloon (while leaving the guidewire in place), and control angiography. In certain cases, prolonged balloon inflation (3 minutes at 3 atm) can overcome severe dissection without stent placement ( Fig. 15.1 ).