Fig. 51.1
Potential UKA placement errors that can occur in coronal plane
Appropriate patient selection and well-designed, accurately implanted prosthetic components have proven to be critical. It is proposed that up to 20 % of total knee replacements could have been UKAs [5]. UKAs have shown improved kinematics as related to total knee replacements, less pain from surgery, and a knee that patients prefer [6–8]. Errors related to conventional instrumentation causing inaccurate bone preparation or stress fractures from pinning can cause early failures.
In the late 1990s, Repicci and Eberle introduced a unicompartmental knee procedure utilizing an inlay tibial component termed “minimally invasive surgery” [9]. This procedure resulted in earlier mobilization, shorter inpatient stay, and shorter length of rehabilitation than had been observed for the conventional incision. However, concerns were raised about loss of accuracy with minimally invasive techniques. With minimally invasive procedures, visualization is reduced leading to potential errors in implant placement, limb alignment, cement technique, and bone preparation (Fig. 51.2) [10, 11].
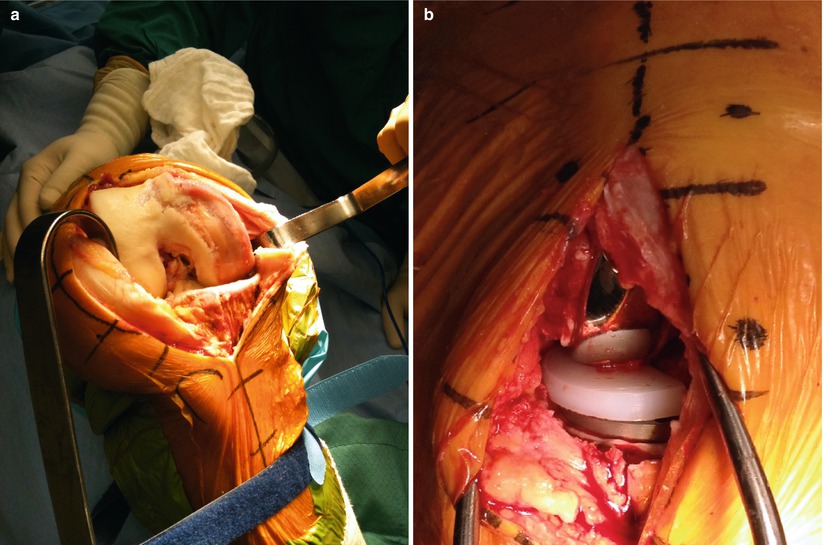
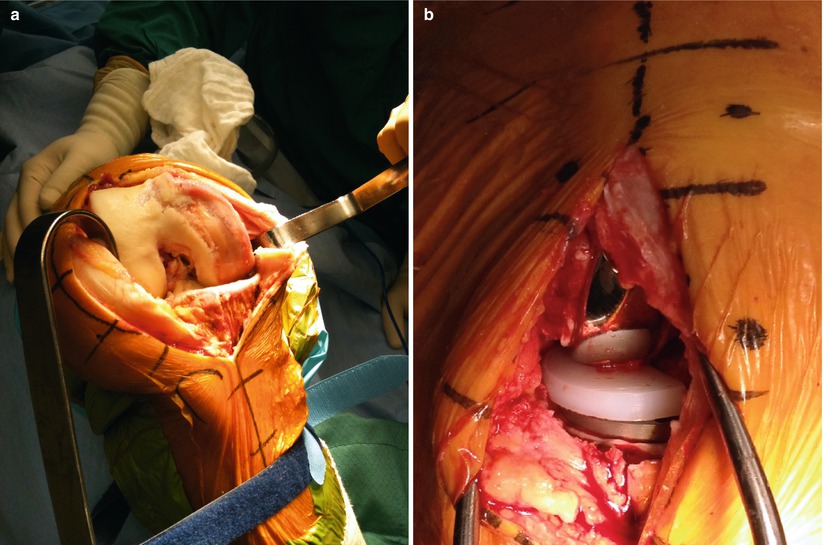
Fig. 51.2
Comparison of incision of both approaches for (a) standard open and (b) minimally invasive implantation of UKA
The introduction of technology to improve accuracy and unicompartmental outcomes began with navigation. Jenny et al. reported on a series of 60 patients who underwent navigated minimally invasive UKA and 60 patients who underwent navigated open UKA. These authors cited the advantages of reduced surgical trauma, reliability, and safety obtained with the navigated minimally invasive procedure, while radiographic accuracy of implantation was the same for both minimally invasive and open navigation techniques [12].
Robotic assistance was first introduced by Justin Cobb using the Acrobot robot in 2000 in order to improve the accuracy of implant positioning during UKA.
Cobb et al. first reported a prospective comparison of a tactile-guided robot-assisted UKA and conventional UKA performed with manual instrumentation [13]. Their robotic system employed static referencing that required rigid intraoperative fixation of the femur and tibia to a stereotactic frame. The primary outcome measurement was the angle of the tibiofemoral alignment in the coronal plane, measured by CT. Implant position errors relative to the planned position averaged 1.1 mm and 2.5° with robotic assistance compared to 2.2 mm and 5.5° conventionally along any axis. Overall tibiofemoral coronal plane alignment was within 2° for every case performed with robotic assistance. Only 40 % of conventional surgery achieved this level of accuracy.
In 2006, MAKO Surgical Corporation obtained FDA clearance to begin the first implantation of medial UKAs using a haptic-controlled passive robotic arm (Fig. 51.3). This system allows an accurate surgical preparation of only the patients’ diseased knee compartment in a singular or multiple compartments, sparing healthy tissue in the undiseased compartment(s). This allows the surgeon to tailor the surgical procedure to the patients’ arthritic and kinematic needs. Addressing the medial, lateral, and patellofemoral joint in an individual, or modular, manner can be planned preoperatively and refined intraoperatively as the patients knee kinematics and disease pathology require.


Fig. 51.3
RIO® Robotic Arm Interactive Orthopedic System manufactured by MAKO Surgical Corp
Modular implants (Fig. 51.4) allowed inlay tibial or onlay tibial components to be used, with an anatomic femoral and trochlear implant. The implants are approved for cementation. The implant design was based on computed tomography (CT)-based parameters of over 100 healthy and diseased knees. The femoral and patellofemoral components are created from a single, continuous surface. The inner geometries are contoured to allow bony preparation using a 6 mm burr. The femoral component allows deep flexion and has angled pegs to improve implant stability. The patellar component is a dome-shaped all-polyethylene three-pegged design, not pictured.


Fig. 51.4
RESTORIS® MCK Multicompartmental Knee System with anatomic design to optimize robotic technique
The integration of robotic arm assistance required a surgeon controlled, highly accurate system that could be integrated into the present surgical workflow. The enabling technology in this robotic platform was the development of haptics. Haptics is the science of applying touch (tactile) sensation and control to interaction with computer applications (Fig. 51.5). The evolution of this technology into the orthopedic arena was enabled by the needs of the surgeon to obtain an accurate reproducible surgical result in all six degrees of freedom (3 translational and 3 rotational), which the human eye cannot reproduce to the same level of precision.
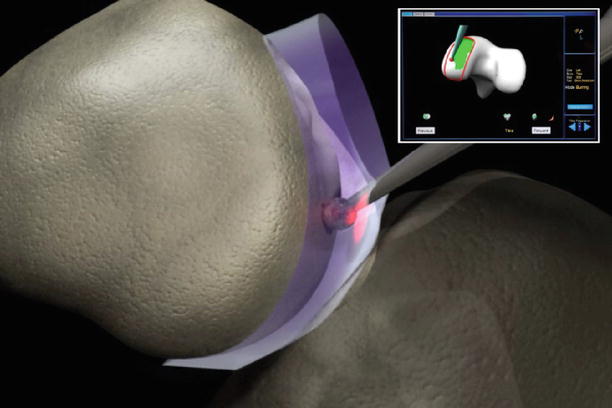
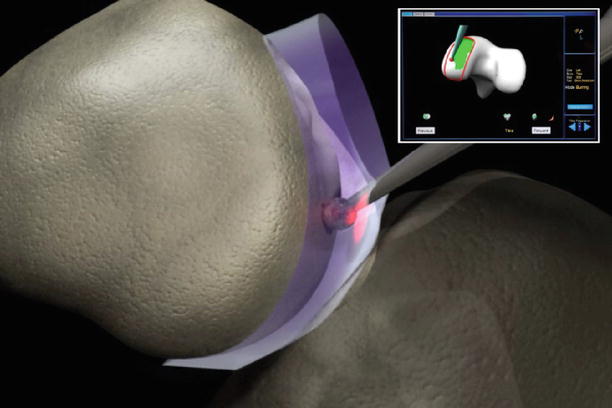
Fig. 51.5
Virtual bone resection shows the RIO® burr in a 3D virtual haptic safe zone. Burr is only active for cutting when burr tip is within haptic safe zone. Allows precise and reproducible bone sculpting. Green depicts the volume of the femoral implant to be resected, Red outline is the edges of the haptic wall
This system utilizes optical motion capture technology to dynamically track marker arrays fixed to the robotic arm, femur, and tibia, allowing the surgeon to freely adjust limb position and orientation during tactile-guided bone cutting. This robotic-assisted platform enables the surgeon to utilize a pre-op computer-assisted planning system and a high-speed burr controlled by a tactile guidance system intraoperatively, thus eliminating the need for conventional instrumentation.
It is important to note that there are several systems in place throughout the procedure to ensure accuracy is achieved. Tibial and femoral checkpoints must be verified before each section of bone is prepared. At any point throughout the procedure, the robotic arm and mechanical burr tip can be removed from the surgical zone, and a tracker probe can be used to visualize accuracy and cuts directly on the patients CT scan (Fig. 51.6).
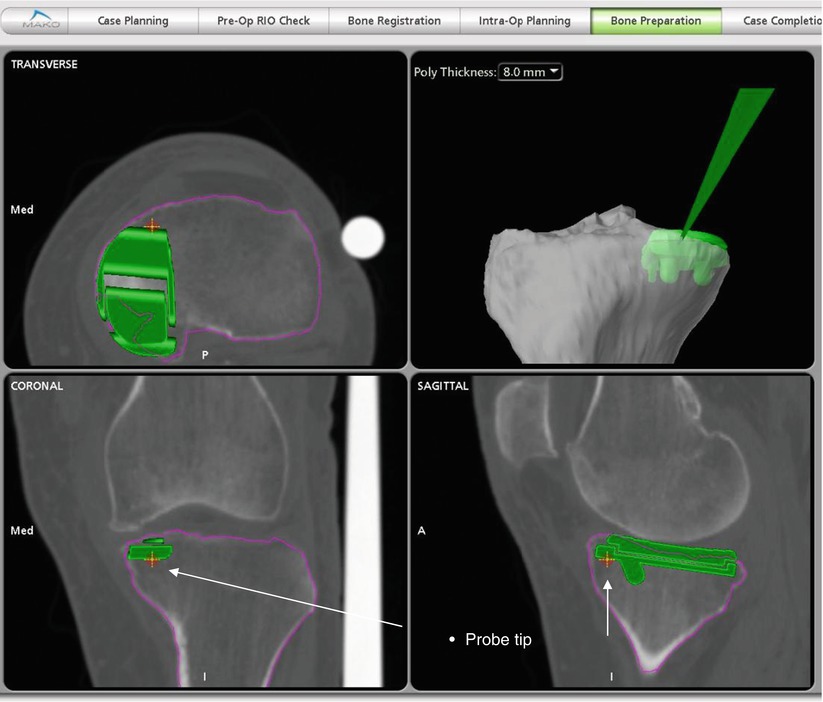




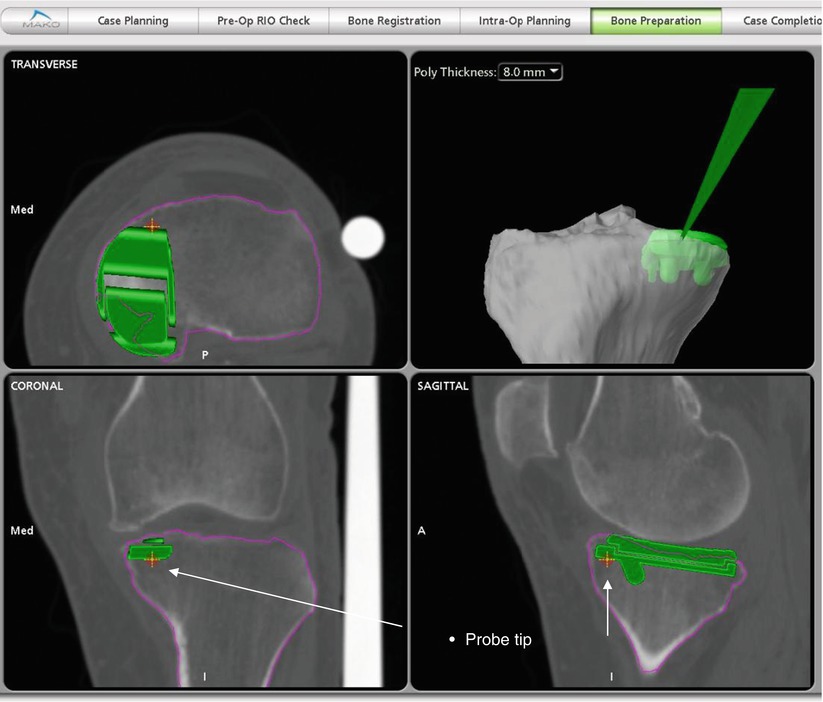
Fig. 51.6
Screen capture from software shows how probe confirms planned depth of cut on CT view
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








