Fig. 16.1
Contrast-enhanced axial scans (a–d). Ulcer of the anterior bulb of the duodenum (red arrow), perforated in the peritoneal cavity. Signs of peritonitis are air in the lesser sac, in the intrahepatic fissure (green arrow), periportal free gas (yellow arrows) and free air in the peritoneal cavity (blue star)
The most significant sign to distinguish upper from lower GI tract perforation is the periportal free gas for the anatomical relationship between the portal tract and the gastric antrum or duodenal bulb (Fig. 16.1).
A distal duodenal perforation produces extraluminal air in the right anterior pararenal space because of the retroperitoneal position of the duodenum distal to the bulb (Fig. 16.2).
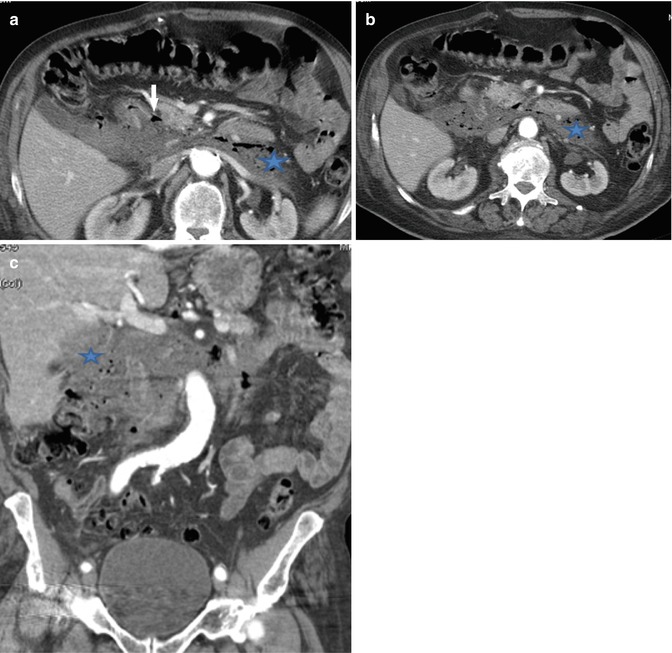
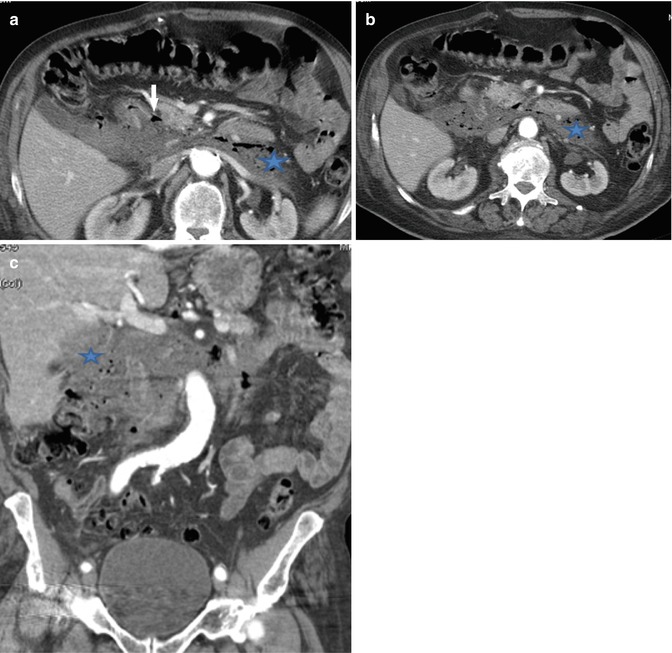
Fig. 16.2
Ulcer in the III portion of the duodenum. (a, b) Axial scans, (c) coronal reconstruction shows a wall defect in the III portion of the duodenum (white arrow) with an inflammatory collection in the retroperitoneal space (blue star)
Other CT signs about the perforated wall are wall thickening and wall focal enhancement.
The stomach and duodenum contain acidic, biliary and pancreatic secretions so that gastric and duodenal perforation produce a rapid chemical peritonitis which can be followed by a systemic inflammatory response syndrome (SIRS) with a possible progress to an infected peritonitis and sepsis.
CT signs of peritonitis due to gastrointestinal perforation are increased fat density adjacent to the site of wall defect, perigastroduodenal fluid, stranding and gas bubbles in close proximity to the site of perforation and fluid between the duodenum and pancreatic head (Fig. 16.2).
16.6 Small Bowel Perforation
The incidence of small bowel perforation is low, but it can be produced by a variety of causes including ischaemic or bacterial enteritis, Crohn disease, diverticulitis, ingested foreign bodies, bowel obstruction, volvulus and intussusceptions [21].
The amount of extraluminal air in these cases is small or absent, and it is depicted only in 50 % of CT performed in patients with small bowel perforation.
When present free air is depicted in the mesenteric folds.
Indirect signs of small bowel perforation and related peritonitis are an increased attenuation of small bowel mesenteric fat, free fluid in the mesenteric folds or leaking of intestinal contents into the interloop spaces.
Crohn disease is a common small bowel inflammatory condition but can rarely lead to free perforation, from the colon (1.6 %) or small bowel (0.7 %) [22].
Small bowel perforation could be a complication of wall ischaemia with transmural necrosis, leading to peritonitis.
Also penetrating abdominal trauma can produce small bowel perforation; in these cases abdominal CT has a sensitivity of 64 % and accuracy of 82 % in detecting the site of perforation even in the absence of the free air but especially with the help of indirect signs as infiltration of the mesentery and/or intraperitoneal fluid [23].
Small bowel perforation can also result from GI lymphoma, GISTs or metastasis.
Fish bones and chicken bones are the most common ingested foreign bodies to cause perforation (Fig. 16.3).
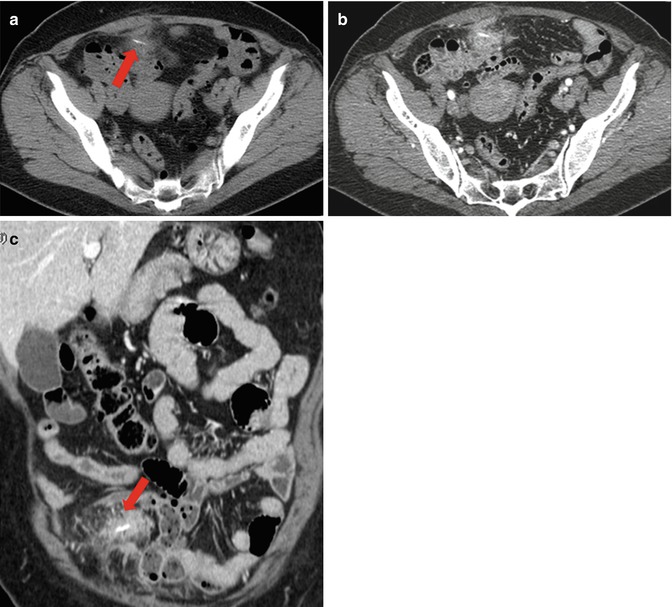
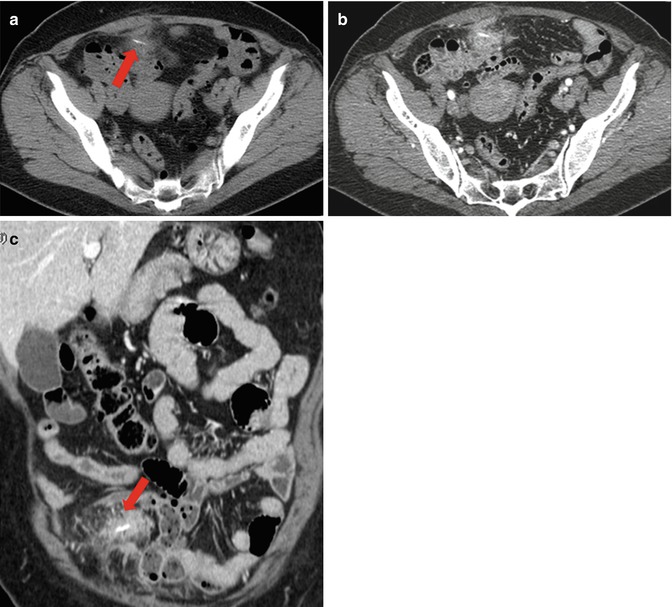
Fig. 16.3
Localized peritonitis. (a) Unenhanced axial scan, (b) enhanced axial scan and (c) coronal MPR reconstruction depicted an extraluminal ingested foreign body, a toothpick (red arrows) close to an ileal loop, at the site of perforation. An inflammatory reaction of the mesenteric fat around the foreign body is also present
16.7 Appendix Perforation
CT has a high sensitivity and specificity for diagnosing acute appendicitis ranging from 94 to 98 % [24]. Unfortunately detecting appendiceal perforation is not so simple in CT especially in early stage; rupture of the appendix, in fact, can be a localized process, and the amount of extraluminal air is usually small or absent (no more than 1 or 2 ml) because acute appendicitis is typically initiated by luminal obstruction.
CT reaches a sensitivity and specificity of 95 % in the diagnosis of perforated appendicitis when it presents a combination of these five findings: (1) extraluminal air, (2) extraluminal appendicolith, (3) abscess, (4) phlegmon and (5) defect in enhancing the appendiceal wall [24] (Figs. 16.4 and 16.5).
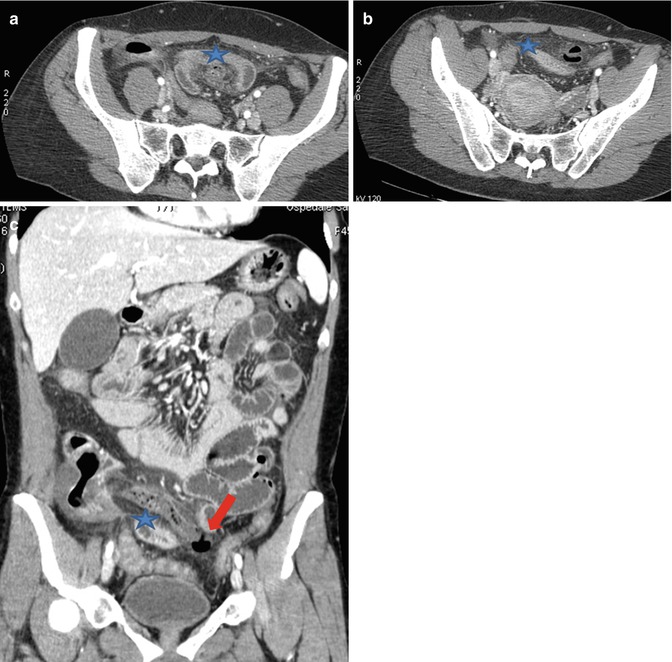
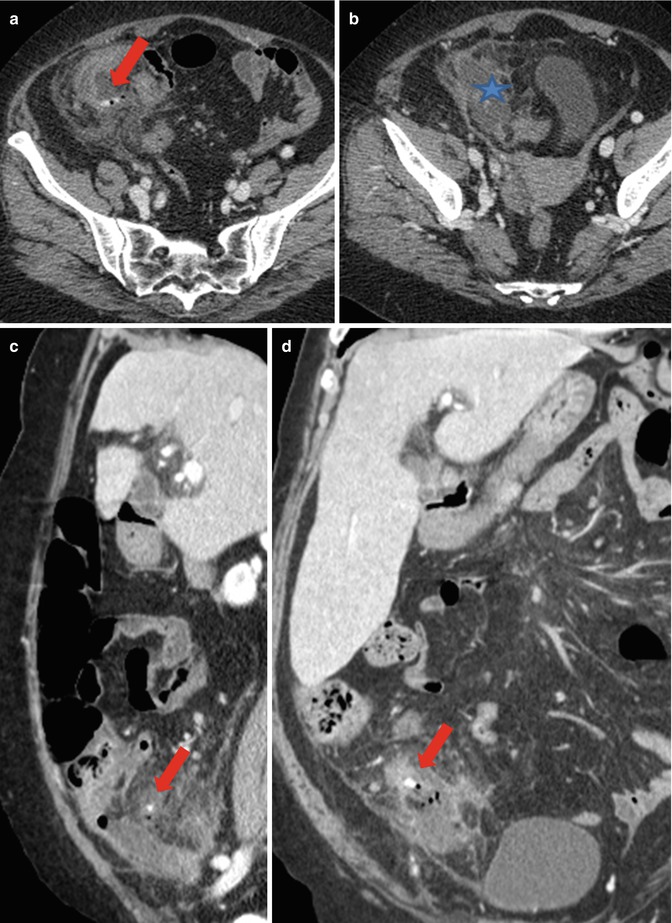
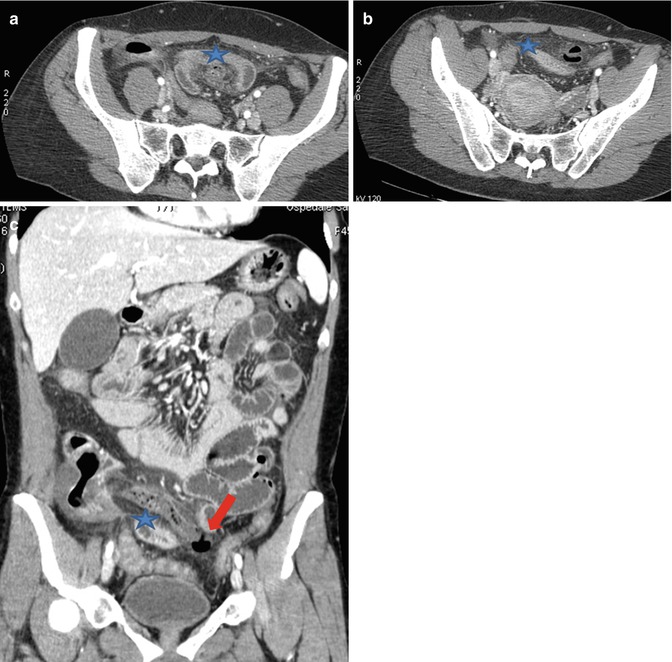
Fig. 16.4
Peritonitis due to mesoceliac perforated appendicitis. (a, b) Axial scans, (c) coronal MPR reconstruction: a long mesoceliac appendicitis (blue star) perforated on the top with free air (red arrow) and inflammatory reaction of the perivisceral fat
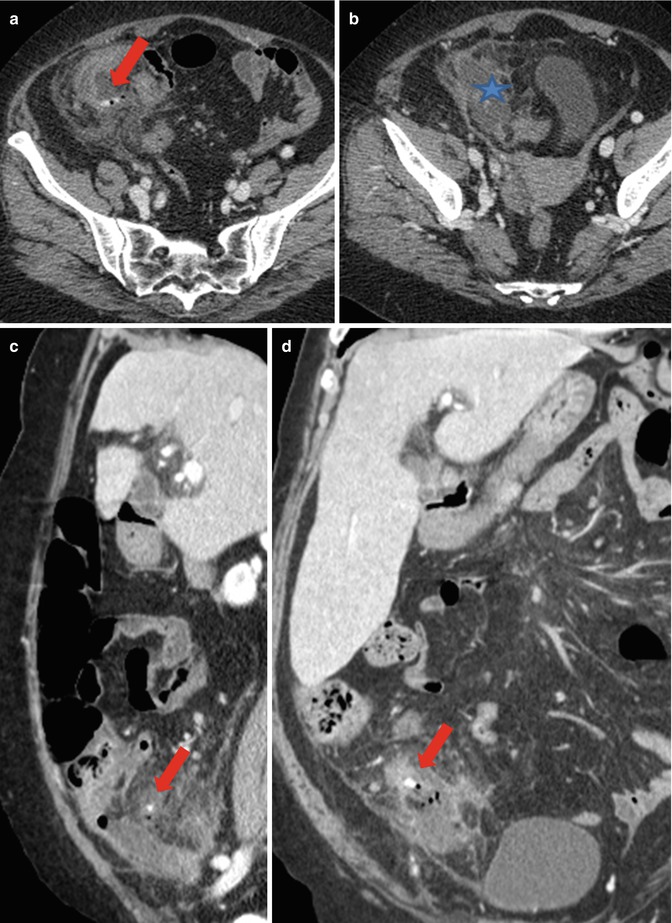
Fig. 16.5
Peritonitis due to gangrenous perforated appendicitis. (a, b) Axial scans, (c) sagittal reconstruction, (d) coronal reconstruction detects a gangrenous perforated appendicitis with extraluminal bubbles and extraluminal appendicoliths (red arrow); also a perivisceral abscess is present (blue star)
The signs of peritonitis as periappendiceal stranding and fluid can be detected in the perforated but also in non-perforated appendicitis.
16.8 Colon Perforation
Malignant neoplasm and diverticulitis are the major causes of large bowel perforation, followed by trauma, ischaemia, inflammatory lesions and iatrogenic causes.
Inflammatory lesions and penetrating trauma are frequently observed in the right colon, whereas malignant neoplasm, spontaneous perforation, diverticulitis, blunt trauma and ischaemia are generally detected in the left colon [21]; perforation of cecum can occur when the intraluminal pressure of the colon is increased, as in the case of bowel obstruction or in malignant tumour (Fig. 16.6).
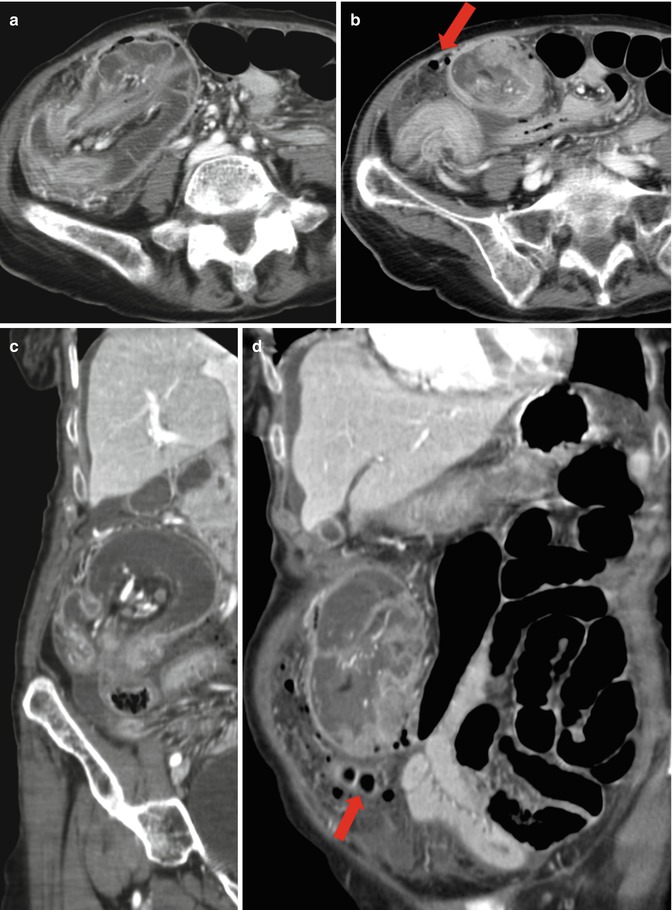
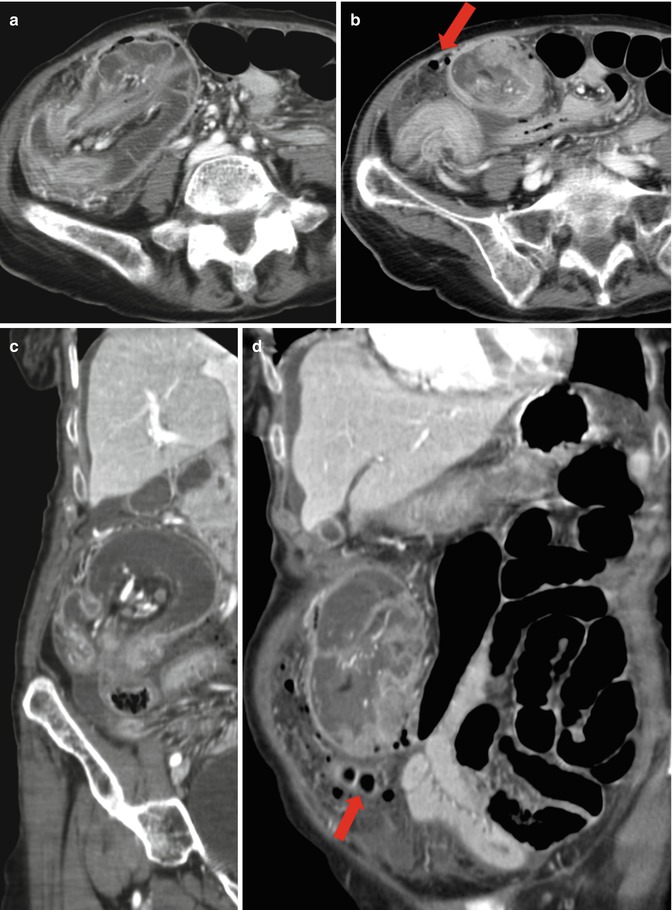
Fig. 16.6




Peritonitis due to perforation of the cecum neoplasm with intussusception. (a, b) Axial scans, (c, d) coronal reconstruction shows a pathological cecum wall thickening with an ileum-cecum-colon intussusception and wall perforation with gas bubbles (red arrow) and an increased attenuation in mesenteric fat
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree