SECTION III DIAGNOSTIC RADIOLOGY IMAGING
Essentials 1
Questions
1. Which ONE of the following is the MOST likely diagnosis?
A. Early intrauterine pregnancy
B. Ectopic pregnancy
C. Ruptured ectopic pregnancy
D. Spontaneous abortion
E. Molar pregnancy
2. Which ONE of the following is the MOST common location for the case diagnosis?
A. Ampullary
B. Isthmic
C. Fimbrial
D. Interstitial
E. Ovarian
3. Which measurement is diagnostic of pregnancy failure?
A. Crown-rump length ≥ 7 mm and no yolk sac
B. Crown-rump length ≥ 7 mm and no heartbeat
C. Mean sac diameter of 16 to 24 mm and no embryo
D. Enlarged yolk sac > 7 mm
E. Small gestational sac in relation to the size of the embryo, < 5 mm difference between the mean sac diameter and crown–rump length
Answers and Explanations
Question 1
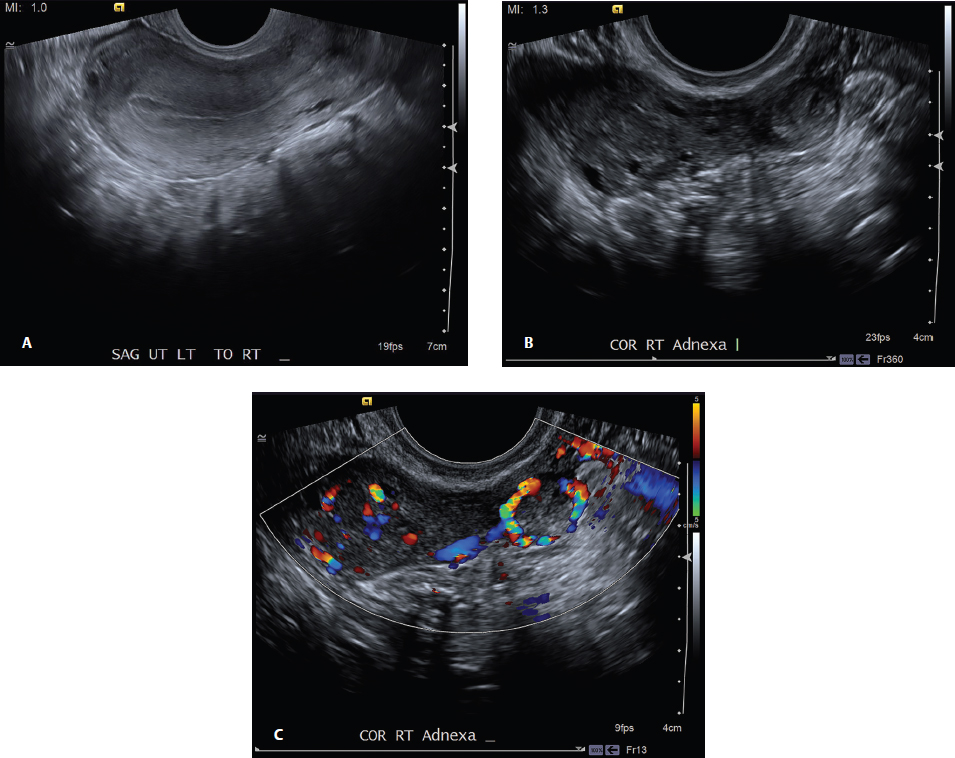
B. Correct! In a patient with a positive pregnancy test, an adnexal mass, and no intrauterine gestational sac, an ectopic pregnancy is the most likely diagnosis. The test case images demonstrate the lack of an intrauterine gestation sac and an adnexal mass associated with a ring of fire.
Other choices and discussion
A. Early intrauterine pregnancy is a diagnostic consideration, but the adnexal mass makes this choice less likely.
C. A ruptured ectopic pregnancy would demonstrate hemorrhagic free fluid, which is not seen in this case.
D. Spontaneous abortion is a diagnostic consideration, but the adnexal mass makes this choice less likely.
E. Abnormal tissue within the uterus would be expected with a hydatidiform molar pregnancy. Hydatidiform moles are a benign form of gestational trophoblastic disease and can either be a complete (absence of an embryo) or partial (abnormal fetus/fetal demise) molar pregnancy.
Question 2
A. Correct! Ampullary. The most common location for an ectopic pregnancy is within the fallopian tube. Within the tube, the most common location is the ampullary portion (75 to 80%). The answer choices are listed in decreasing frequency. Abdominal, cervical, and scar ectopic pregnancies are rare. 1
Question 3
B. Correct! A crown–rump length ≥ 7 mm and no heartbeat is diagnostic of pregnancy failure.
Other choices and discussion
A. This is not a criterion.
C. Mean sac diameter of 16 to 24 mm without an embryo is suspicious but not diagnostic for pregnancy failure.
D. Enlarged yolk sac > 7 mm is suspicious but not diagnostic for pregnancy failure.
E. A small gestational sac relative to the size of the embryo is suspicious but not diagnostic for pregnancy failure.
References
1. Levine D. Ectopic pregnancy. Radiology 2007;245(2):385–397 2. Doubilet PM, Benson CB, Bourne T, et al. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med 2013;369(15):1443–1451Top Tips
“Ring of fire” is not a specific sonographic finding and can be seen in ectopic pregnancy, corpus luteal cyst, or hemorrhagic cyst.
Methotrexate is the treatment of choice in stable patients with tubal ectopic pregnancy. Surgical treatment is indicated if the ectopic pregnancy has cardiac activity or if the adnexal mass is > 4 cm.
Findings diagnostic of pregnancy failure include:
Crown–rump length ≥ 7 mm and no heartbeat
Mean sac diameter of ≥ 25 mm and no embryo
Absence of embryo with heartbeat ≥ 2 weeks after a scan that showed a gestational sac without a yolk sac
Absence of embryo with heartbeat ≥ 11 days after a scan that showed a gestational sac with a yolk sac 2
Essentials 2
Questions
1. Which ONE of the following is the MOST likely diagnosis?
A. Bladder calculus
B. Left ureterovesicular junction calculus
C. Phlebolith
D. Bladder wall calcification
E. Calcification of a bladder carcinoma
2. What is the largest sized urinary calculus that will likely (> 50%) pass with medical treatment alone?
A. 3 mm
B. 4 mm
C. 5 mm
D. 6 mm
E. 7 mm
3. Which ONE of the following type of urinary calculus is radiolucent on computed tomography?
A. Calcium oxalate
B. Cystine
C. Indinavir
D. Struvite
E. Uric acid
Answers and Explanations
Question 1
B. Correct! There is a calculus at the UVJ that is impacted or “telescoped” into the bladder. The axial images demonstrate subtle left posterior wall thickening and enhancement that extends to the calculus. The images show a “floating” calculus, signifying that it is held by soft tissue. If desired, prone images could be used to confirm that the calculus is impacted in the UVJ.
Other choices and discussion
A. Bladder calculi are most commonly found in the most dependent portion of the bladder (i.e., the midline or within a diverticulum). Bladder calculi can either form within the urinary bladder from urinary stasis or can represent calculi that move from the proximal collecting system into the bladder.
C. Phleboliths are calcifications within veins and are the most common mimic of urinary calculi in the distal ureter. Phleboliths are not surrounded by ureteral tissue, however, as is seen in this case.
D. Bladder wall calcifications are normally more thin and linear than the depicted ovoid calcification. Causes of bladder wall calcifications include schistosomiasis, tuberculosis, and bladder carcinoma. 1
E. Calcifications found with bladder carcinoma normally “encrust” the tumor along the intravesicular side.
Question 2
C. Correct! 5 mm. It is generally accepted that calculi that are ≤ 5 mm will spontaneously pass the majority of time (68%), and stones that are between 5 and 10 mm will pass < 50% of the time. Calcium channel blockers and alpha-receptor antagonists can be used to help facilitate passage. When medical therapy fails or if the calculi are too large to pass, shock-wave lithotripsy and ureteroscopy are the next steps in management. 2
Question 3
C. Correct! Indinavir sulfate is a protease inhibitor used in the treatment of human immunodeficiency virus. These stones form in approximately 20% of patients and are not reliably seen on computed tomography (CT). 3
Other choices and discussion
The remaining stones can all be seen on CT.
A. Calcium-based stones are the most common type of genitourinary stones (70 to 80%).
B. Cystine stones are associated with cystinuria, which is an autosomal recessive inherited disease that causes impairment in reabsorption of cystine in the proximal tubules.
D. Struvite stones form in the setting of urinary tract infections (urease-producing bacteria) and produce magnesium ammonium phosphate crystals. They can form staghorn calculi.
E. Uric acid stones are not seen on conventional radiography but are seen on CT. These can be treated with urinary alkalinization as first-line therapy. 4
References
1. Shinagare AB, Sadow CA, Sahni VA, Silverman SG. Urinary bladder: normal appearance and mimics of malignancy at CT urography. Cancer Imaging 2011;11:100–108 2. Preminger GM, Tiselius HG, Assimos DG, et al. 2007 guideline for the management of ureteral calculi. J Urol 2007;178(6):2418–2434 3. Schwartz BF, Schenkman N, Armenakas NA, Stoller ML. Imaging characteristics of indinavir calculi. J Urol 1999;161(4):1085–1087 4. Kambadakone AR, Eisner BH, Catalano OA, Sahani DV. New and evolving concepts in the imaging and management of urolithiasis: urologists’ perspective. Radiographics 2010;30(3):603–623Top Tips
Indinavir = invisible on all imaging
Uric acid = uncovered on CT, invisible on radiography
Struvite = staghorn
Calcium oxalate = commonly occurring
Cystine = congenital
Calculi ≤ 5 mm = medical treatment (calcium channel blocker and alpha-receptor antagonist)
Essentials 3
Questions
1. Which ONE of the following is the MOST likely diagnosis?
A. Obstructive uropathy
B. Pyelonephritis
C. Pyonephrosis
D. Renal infarction
E. Lymphoma
2. Which ONE of the following is the BEST management for a young and otherwise healthy female suspected to have an uncomplicated case of the diagnosis shown above?
A. Computed tomography (CT) to confirm pyelonephritis, outpatient treatment with oral antibiotics
B. CT to confirm pyelonephritis, inpatient intravenous (IV) antibiotics
C. CT to confirm pyelonephritis, IV antibiotics in an emergency department, outpatient treatment with oral antibiotics
D. Ultrasound to confirm pyelonephritis, IV antibiotics in an emergency department, inpatient treatment with IV antibiotics
E. Clinical assessment to confirm pyelonephritis, IV antibiotics in an emergency department, outpatient treatment with oral antibiotics
3. How does treatment differ between pyelonephritis and pyonephrosis?
A. No difference
B. Pyonephrosis needs more aggressive hydration
C. Antibiotic treatment for pyelonephritis, outpatient treatment for pyonephrosis
D. Antibiotic treatment for pyelonephritis, urgent percutaneous nephrostomy for pyonephrosis
E. Antibiotic treatment for pyelonephritis, surgical nephrectomy for pyonephrosis
Answers and Explanations
Question 1
B. Correct! The “striated” nephrogram seen in the test case is the classic appearance of pyelonephritis. The areas of low attenuation involve both the cortex and medullary components, and the differentiation between the two is blurred. Areas of normal intervening parenchymal enhancement are commonly seen. This case is slightly atypical, as pyelonephritis is more common in women than in men.
Other choices and discussion
A. Obstructive uropathy can cause asymmetric delayed enhancement of the kidney. However, the process affects the entire kidney, and the corticomedullary differentiation is usually maintained. Obstruction can result from calculi, intrinsic/extrinsic mass, or bladder outlet obstruction.
C. Pyonephrosis refers to infection or pus within the collecting system with an obstructive component. This obstructive component can occur from calculi or a mass, but can also result from the pus alone. Imaging findings show a dilated collecting system, which is not seen in this case. Ultrasound shows debris within the collecting system.
D. Renal infarction can have wedge-shaped areas of nonenhancement, which can look similar to this striated nephrogram. Unless embolic, infarcts are less often multiple (and if embolic and originating from the heart, bilateral disease would be expected). In addition, the “cortical-rim” sign is absent, which is seen in approximately 50% of renal infarcts. The cortical-rim sign refers to normal enhancement along the capsule from the capsular artery. It usually takes at least 8 hours for this sign to develop. 1
E. Lymphoma could mimic the appearance of the test case. Infiltrative lymphoma often enlarges the kidney, however, which is not seen in this case. In addition, retroperitoneal lymph node involvement is absent.
Question 2
E. Correct! If a young female that is otherwise healthy has clinical signs and symptoms of uncomplicated pyelonephritis, no imaging is needed! The patient should be evaluated in an emergency department and treated with IV fluids and a dose of IV antibiotics. The patient can then be treated as an outpatient with oral antibiotics. If the patient fails outpatient treatment after 72 hours or has suspected complicated pyelonephritis, a CT with contrast is the study of choice. In these cases, renal abscess, pyonephrosis, and source of obstruction should be sought. These patients should also be admitted to the hospital for IV antibiotic therapy. 2 , 3
Question 3
D. Correct! Urgent percutaneous nephrostomy or ureteral stent placement for decompression and drainage of the infective debris is the treatment of choice for pyonephrosis.
Discussion
Pyelonephritis should be evaluated in an emergency department with IV antibiotics and aggressive IV hydration.
Pyonephrosis needs urgent decompression of the dilated collecting system and drainage of the pus.
Although pyonephrosis can lead to urosepsis, surgical removal of the kidney is the last resort.
References
1. Kamel IR, Berkowitz JF. Assessment of the cortical rim sign in posttraumatic renal infarction. J Comput Assist Tomogr 1996;20(5):803–806 2. Soulen MC, Fishman EK, Goldman SM, Gatewood OM. Bacterial renal infection: role of CT. Radiology 1989;171(3):703–707 3. Nikolaidis P, Casalino DD, Remer EM, et al. ACR Appropriateness Criteria® Acute Pyelonephritis. https://acsearch.acr.org/docs/69489/Narrative/. Accessed February 29, 2016Top Tips
Pyonephrosis requires urgent percutaneous catheter drainage or ureteral stent placement
Cortical-rim sign can be seen in renal vascular compromise (infarct), but this sign is only seen about 50% of the time and only becomes apparent after 8 hours.
Lymphoma can mimic pyelonephritis on CT.
Essentials 4
Questions
1. Based only on image A, what is the MOST likely diagnosis?
A. Acute necrotizing pancreatitis
B. Acute edematous pancreatitis
C. Chronic pancreatitis
D. Duodenitis
E. Gastritis
2. Follow-up imaging of the same patient 5 weeks later is shown in image B. What does this collection most likely represent?
A. Acute peripancreatic collection with superimposed infection
B. Acute necrotic collection with superimposed infection
C. Pseudocyst without superimposed infection
D. Pseudocyst with superimposed infection
E. Walled-off necrosis with superimposed infection
3. Which ONE of the following is a criterion for pseudocyst treatment?
A. Compression of small vessels
B. Sterile pseudocyst
C. Compression of the common bile duct
D. At least 3 cm in diameter
E. Pancreaticoduodenal fistula
Answers and Explanations
Question 1
A. Correct! On image A, we see decreased enhancement of nearly the entire pancreas, which is a sign of necrotizing pancreatitis. Peripancreatic inflammation as well as peripancreatic and intraperitoneal fluid are present. Acute pancreatitis is classified into early (first week) and late (> 1 week) phases. Acute pancreatitis is also classified into edematous and necrotizing pancreatitis. 1 The severity of pancreatitis is based on the presence or absence of organ failure.
Other choices and discussion
B. Acute edematous pancreatitis usually maintains normal or nearly normal enhancement, unlike this case. There may be mildly decreased attenuation due to pancreatic and peripancreatic edema.
C. Chronic pancreatitis is a recurrent process with the following common associations: pancreatic ductal dilatation, pancreatic atrophy, and parenchymal calcifications.
D. Although the inflammation of duodenitis can extend into the peripancreatic space, the inflammation in the test case is pancreas-centered. The most common cause of duodenitis is secondary inflammation from pancreatitis.
E. Gastritis is normally depicted as gastric wall or submucosal edema. Gastric ulceration may also be present. These findings are not seen in the test case. The most common cause of gastritis is Helicobacter pylori infection.
Question 2
E. Correct! This is walled-off necrosis of the pancreas. By definition, this occurs after 4 weeks. Walled-off necrosis is usually centered in the space where the pancreas resides. In this case, there are multiple gas bubbles, which are compatible with superimposed infection. This collection should be treated.
Other choices and discussion
A. Acute peripancreatic collection is seen within the first 4 weeks of edematous pancreatitis. It is usually adjacent to the pancreas and has a homogenous fluid density.
B. Acute necrotic collection is seen within the first 4 weeks of necrotizing pancreatitis and is a heterogeneous collection.
C. Pseudocysts occur after 4 weeks and are usually adjacent to the pancreas. They have a well-defined wall and are usually homogenous and of fluid density. Pseudocysts may communicate directly with the pancreatic ducts.
D. Although this collection is infected, it is not a pseudocyst.
Question 3
C. Correct! A pseudocyst should be treated if it causes external compression on the common bile duct.
Other choices and discussion
A. A pseudocyst should be treated if there is compression of large vessels.
B. Infected pseudocysts should be drained.
D. A pseudocyst should be treated if the diameter is > 5cm and size and morphology have not changed for more than 6 weeks.
E. A pseudocyst should be treated if there is a pancreaticopleural fistula. 2
References
1. Thoeni RF. The revised Atlanta classification of acute pancreatitis: its importance for the radiologist and its effect on treatment. Radiology 2012;262(3):751–764 2. Aghdassi AA, Mayerle J, Kraft M, Sielenkamper AW, Heidecke CD, Lerch MM. Pancreatic pseudocysts—when and how to treat? HPB (Oxford) 2006;8(6):432–441Top Tips
Pseudocysts require > 4 weeks to develop in acute pancreatitis by definition (Revised Atlanta classification of acute pancreatitis 2012).
Severity of acute pancreatitis is based on whether organ failure (OF) is present and, if present, for how long. These are separated into mild (no OF), moderate (< 48 hours of OF), and severe (> 48 hours of OF).
Necrotizing pancreatitis demonstrates lack of enhancement on computed tomography imaging.
Essentials 5
Questions
1. Which ONE of the following is the MOST likely diagnosis?
A. Pulmonary edema
B. Pneumonia
C. Pleural effusion
D. Pneumothorax
E. Atelectasis
2. Which ONE of the following is a DIRECT sign of the case diagnosis?
A. Increased lung density
B. Elevation of the diaphragm
C. Hilar displacement
D. Mediastinal shift
E. Compensatory hyperinflation
3. What is the MOST appropriate next step in the management of this patient?
A. No further management necessary
B. Incentive spirometry
C. Chest computed tomography
D. Bronchodilator
E. Antibiotics
Answers and Explanations
Question 1
E. Correct! This is a case of atelectasis. There is volume loss of the left lung depicted by elevation of the left hemidiaphragm and leftward shift of the mediastinum. Left upper lobe atelectasis can have varying degrees of volume loss. It typically collapses anteriorly and superiorly, as is shown on the lateral radiograph. This can cause a left lung “veil-like” density on the frontal radiograph. It is important to remember that particularly in an adult, lobar atelectasis should be considered secondary to neoplasm until proven otherwise.
Other choices and discussion
A. Pulmonary edema is typically bilateral and when unilateral, it usually affects the right, not the left, lung.
B. Pneumonia is a differential consideration in this case. Typically, pneumonia should be a space-occupying lesion (pus in the alveoli), not a process that predominantly causes volume loss.
C. Pleural effusions can cause increased density overlying the left hemithorax on the frontal view, but the lateral radiograph shows the opacity along the anterior chest wall. Free-flowing pleural fluid would be expected posteriorly.
D. A tension pneumothorax can shift the mediastinum, but would not cause an anterior opacity on the lateral radiograph. Additionally, a visceral pleural line to confirm a pneumothorax would be expected.
Several named signs of volume loss:
“Golden S” sign—Right upper lobe collapse with minor fissure elevation and a downward bulge in the medial portion of the minor fissure. Caused by a centrally obstructing mass. 1
“Luftsichel” sign—Hyperinflated superior segment of the left lower lobe outlining the aortic arch. Seen in left upper lobe collapse. 1
“Flat waist” sign—Left lower lobe collapse with cardiac rotation and subsequent loss of the left heart border concavity. 2
Question 2
A. Correct! Increased pulmonary density is a direct sign of atelectasis. Other direct signs of atelectasis include displacement of the fissures and crowding of the bronchi.
Other choices and discussion
B. Elevation of the diaphragm is an indirect sign of atelectasis.
C. Hilar displacement is an indirect sign of atelectasis.
D. Mediastinal shift is an indirect sign of atelectasis.
E. Compensatory hyperinflation is an indirect sign of atelectasis.
Note that ipsilateral intercostal space narrowing is also an indirect sign of atelectasis.
Question 3
C. Correct! The use of a chest CT is invaluable for the evaluation of a potential centrally obstructing mass that causes secondary atelectasis.
Other choices and discussion
A. Further management is needed. The cause of the left upper lobe atelectasis must be determined.
B. Incentive spirometry is a commonly used tool to help promote healthy lung function following surgery or a respiratory illness, but is not used to diagnose an unknown cause of lobar atelectasis.
D. Mucous plugging (e.g., with asthma) causing atelectasis can be improved with bronchodilator therapy, but a CT chest to exclude an underlying mass is crucial.
E. Antibiotics are used to treat an infectious process, not atelectasis.
References
1. Woodring JH, Reed JC. Radiographic manifestations of lobar atelectasis. J Thorac Imaging 1996;11(2):109–144 2. Kattan KR, Wlot JF. Cardiac rotation in left lower lobe collapse. “The flat waist sign.” Radiology 1976;118(2):275–279Top Tips
Direct signs of atelectasis:
Increased density
Displacement of fissures
Crowding of bronchi
Indirect signs of atelectasis:
Mediastinal shift
Elevation of the ipsilateral hemidiaphragm
Ipsilateral intercostal space narrowing
Compensatory hyperinflation of other lobes or the contralateral lung
Where does the collapsed lung go?
Left upper lobe—anteriorly and superiorly
Right upper lobe—superiorly and medially
Right middle lobe—inferiorly and medially
Right lower lobe and left lower lobe—inferiorly, medially, and posteriorly
Essentials 6
Questions
1. Which ONE of the following is the MOST likely diagnosis?
A. Pulmonary edema
B. Lobar pneumonia
C. Usual interstitial pneumonia
D. Sarcoidosis
E. Pulmonary emboli with pulmonary infarction
2. What pulmonary wedge pressure is MOST commonly seen with an INTERSTITIAL case of the diagnosis above?
A. 8 to 12 mm Hg
B. 12 to 17 mm Hg
C. 17 to 25 mm Hg
D. > 25 mm Hg
3. Which ONE of the following can cause localized right upper lobe pulmonary edema?
A. Acute mitral regurgitation
B. Chronic mitral regurgitation
C. Mitral stenosis
D. Low ejection fraction
E. Dilated cardiomyopathy
Answers and Explanations
Question 1
A. Correct! This is pulmonary edema. Bilateral perihilar opacities have a broad differential diagnosis. The key to this diagnosis is the follow up radiograph, which demonstrates resolution of the pulmonary opacities. Given this short time interval, pulmonary edema is the most likely diagnosis.
Other choices and discussion
B. Lobar pneumonia is typically seen in one lobe and often depicted by consolidation with air bronchograms. The test case image could represent bronchopneumonia, which is commonly associated with multifocal patchy opacities, as well as tree-in-bud opacities on computed tomography.
C. Usual interstitial pneumonia is an interstitial lung disease that predominately affects the lung bases. It has a reticular pattern and subpleural involvement with pulmonary fibrosis and associated “honeycombing.”
D. Sarcoidosis has five radiographic stages (0 to 4). Stage 0 has a normal chest radiograph. Stage 1 has the classic 1-2-3 sign, which depicts lymph node enlargement of the right paratracheal, right hilar, and left hilar lymph nodes. Stage 2 has nodal enlargement and parenchymal disease. Stage 3 has only parenchymal disease. Stage 4 is end-stage pulmonary sarcoidosis, associated with pulmonary fibrosis. Although the test case could have the appearance of stage 3 pulmonary sarcoidosis, the rapid resolution of the pulmonary opacities would be atypical.
E. Pulmonary emboli with pulmonary infarction may cause consolidative opacity. However, this opacity usually extends to the periphery. Hampton’s hump is a radiologic sign of pulmonary infarction, depicted by a wedge-shaped peripheral opacity.
Question 2
C. Correct! Interstitial pulmonary edema is seen at 17 to 25 mm Hg. Kerley lines are present. 1
Other choices and discussion
A. The normal pulmonary wedge pressure is 8 to 12 mm Hg.
B. Pressures of 12 to 17 mm Hg will demonstrate cephalization (redistribution to the upper lobes).
D. Alveolar pulmonary edema is seen when the pulmonary wedge pressure increases beyond 25 mm Hg.
Question 3
A. Correct! Acute mitral regurgitation can lead to acute right upper lobe pulmonary edema. This can be secondary to myocardial infarction with subsequent papillary muscle rupture or rupture of the chordae tendineae. Mitral valve replacement is the treatment of choice. 2 Other etiologies include infective endocarditis and acute rheumatic fever.
Other choices and discussion
B. Chronic mitral regurgitation will lead to left ventricular enlargement, dilatation of the left atrium, and ultimately, the development of left ventricular failure. This results in diffuse pulmonary edema. 3
C. Mitral stenosis is commonly associated with an enlarged left atrium, which is seen as the “double density” sign on chest radiography. This condition may lead to diffuse interstitial pulmonary edema.
D. Low ejection fracture may cause diffuse pulmonary edema.
E. Dilated cardiomyopathy is normally depicted as a large left ventricle with associated diffuse pulmonary edema.
References
1. Gluecker T, Capasso P, Schnyder P, et al. Clinical and radiologic features of pulmonary edema. Radiographics 1999;19(6):1507–1531; discussion 1532–1503 2. Schnyder PA, Sarraj AM, Duvoisin BE, Kapenberger L, Landry MJ. Pulmonary edema associated with mitral regurgitation: prevalence of predominant involvement of the right upper lobe. Am J Roentgenol 1993;161(1):33–36 3. Woolley K, Stark P. Pulmonary parenchymal manifestations of mitral valve disease. Radiographics 1999;19(4):965–972Top Tips
Chest radiographic findings of pulmonary edema wax and wane over hours or days, depending on fluid status.
Acute mitral valve regurgitation (papillary muscle rupture) can lead to right upper lobe pulmonary edema after myocardial infarction.
Bronchopneumonia is commonly seen as multifocal patchy pulmonary opacities on chest radiograph and may have tree-in-bud opacities on computed tomography.
Essentials 7
Questions
1. Which ONE of the following is the MOST important finding on the test case images?
A. Aortic dissection
B. Intramural hematoma
C. Abdominal aortic aneurysm
D. Aortic pseudoaneurysm
E. Aortic rupture
2. Which ONE of the following criteria warrants elective repair of the case diagnosis?
A. AAA measuring 4.5 cm in a woman
B. AAA measuring 5 cm in a man
C. AAA measuring at least 1.5 times the expected diameter of the aorta
D. AAA expanding at a rate of at least 5 mm/year
E. AAA expanding at a rate of at least 10 mm/year
3. Which sign is associated with impending AAA rupture?
A. Aortic nipple sign
B. Draping aorta sign
C. Three sign
D. Hyperattenuating crescent sign
E. Air crescent sign
Answers and Explanations
Question 1
E. Correct! The critical finding on this case is a ruptured abdominal aortic aneurysm (AAA) with a large volume of retroperitoneal hemorrhage. Most unruptured AAAs are asymptomatic. Rupture is associated with a high mortality. The images provided demonstrate a large aortic aneurysm with contrast extending through a posterolateral defect and a large left retroperitoneal hematoma.
Other choices and discussion
A. Aortic dissection is not demonstrated. Aortic dissection is most commonly associated with hypertension.
B. There is intramural hematoma, but this is not the salient finding. Intramural hematoma refers to hemorrhage within the aortic wall from the vaso vasorum. 1
C. An AAA is absolutely present in this case, but the rupture is the most important finding. AAA is defined as enlargement of the abdominal aorta > 1.5 times the normal adjacent diameter or a measurement of > 3 cm.
D. Aortic pseudoaneurysms are usually posttraumatic and result in focal outpouchings of the aorta. There is disruption of at least one layer of the aortic wall, and these are contained ruptures.
Question 2
E. Correct! An AAA expanding at a rate of at least 10 mm/year is a criterion warranting elective AAA repair.
Other choices and discussion
A. AAA size of > 5 cm in female patients warrants elective AAA repair.
B. AAA size of > 5.5 cm in male patients warrants elective AAA repair.
C. An AAA is defined when the vessel measures at least 1.5 times the expected diameter of the aorta. However, this is not a criterion for elective repair.
D. A rapidly expanding AAA is measured as > 5 mm in 6 months or > 10 mm in 1 year, and these criteria warrant elective AAA repair.
Question 3
D. Correct! The hyperattenuating crescent sign on noncontrast computed tomography (CT) can be seen in patients with impending AAA rupture. This sign represents acute hematoma in either the mural thrombus or within the aortic wall. A noncontrast CT examination can help in differentiating between blood pool and aortic wall/mural thrombus.
Other choices and discussion
A. The “aortic nipple” sign is a tiny bump along the aortic arch on plain radiography that correlates with the left superior intercostal vein.
B. The “draping aorta” sign signifies a contained rupture.
C. The “three” sign is seen in coarctation of the aorta. This is comprised of the dilated left subclavian artery, indentation of the coarctation, and the poststenotic aortic dilatation.
E. The “air crescent” sign is seen as a radiolucent pulmonary cavity surrounding a mass. This is classically seen with aspergilloma.
References
1. Macura KJ, Corl FM, Fishman EK, Bluemke DA. Pathogenesis in acute aortic syndromes: aortic dissection, intramural hematoma, and penetrating atherosclerotic aortic ulcer. Am J Roentgenol 2003;181(2):309–316 2. Khosa F, Krinsky G, Macari M, Yucel EK, Berland LL. Managing incidental findings on abdominal and pelvic CT and MRI, Part 2: white paper of the ACR Incidental Findings Committee II on vascular findings. J Am Coll Radiol 2013;10(10):789–794Suggested Readings
Restrepo CS, Ocazionez D, Suri R, Vargas D. Aortitis: imaging spectrum of the infectious and inflammatory conditions of the aorta. Radiographics 2011;31(2):435–451 Takayama T, Miyata T, Nagawa H. True abdominal aortic aneurysm in Marfan syndrome. J Vasc Surg 2009;49(5):1162–1165Top Tips
Due to the increasing chance of AAA rupture based on size, as the AAA grows, the imaging follow-up interval should decrease. Recommended guidelines for follow-up include 2 :
Aortic diameter
Imaging interval
2.5–2.9 cm
5 years
3.0–3.4 cm
3 years
3.5–3.9 cm
2 years
4.0–4.4 cm
1 year
4.5–4.9 cm
6 months
5.0–5.5 cm
3–6 months
Atherosclerosis is the most common cause of AAAs. Other risk factors include smoking, male gender, diabetes, hypertension, and hypercholesterolemia. 2
Acute intramural hematoma can be seen in cases of impending AAA rupture. On noncontrast CT, this manifests as crescentic high attenuation (60 to 70 HU) thickening of the aortic wall.
Essentials 8
Questions
1. Which ONE of the following is the MOST likely diagnosis?
A. Jefferson burst fracture (C1)
B. Hangman’s fracture (C2)
C. Flexion teardrop injury
D. Extension teardrop injury
E. Rotary subluxation
2. Using the Levine and Edwards classification, how would this injury be classified? (Hint: there is 3.5 mm of anteroposterior translation, and angulation is present.)
A. Type I
B. Type II
C. Type IIA
D. Type III
3. What is the appropriate treatment for type I traumatic spondylolisthesis of the axis?
A. Rigid cervical collar for 4 to 6 weeks
B. Halo immobilization for 6 to 12 weeks
C. Internal fixation
D. Reduction using hyperextension, then halo immobilization for 6 to 12 weeks
Answers and Explanations
Question 1
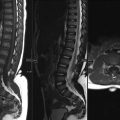
B. Correct! This is a hangman’s fracture. Traumatic spondylolisthesis of the axis is also known as a hangman’s fracture, a name termed after judicial hangings. However, this type of injury is now most commonly seen in motor vehicle collisions and falls. It is defined by bilateral fractures of the pars interarticularis of C2. The mechanism of injury is hyperextension. 1 The test case image demonstrates bilateral fractures of the pars interarticularis of C2 with anterior translation of C2 on C3 and angulation of C2.
Other choices and discussion
A. Jefferson burst fracture involves C1 and is best evaluated on the open-mouth odontoid view.
C. Flexion teardrop injury is considered a distraction-type injury. It usually affects the subaxial cervical spine, with injury starting from the supraspinous ligament and continuing anteriorly with a superimposed compression component. This causes a large fracture fragment of the anteroinferior portion of the affected vertebral body.
D. Extension teardrop injury is considered a distraction-type injury. It usually affects the subaxial cervical spine, with the injury starting from the anterior aspect of the cervical spine. There is an avulsion fracture of the anterior aspect of the inferior endplate.
E. Rotary subluxation involves the C1–C2 articulation.
Question 2
B. Correct! This is type II. Type I fractures have < 3 mm anteroposterior translation without an angulation component. Type II fractures have > 3 mm of anteroposterior translation with angulation (> 11 degrees) and disruption of the posterior longitudinal ligament. Type IIA fractures have a horizontal fracture line instead of a vertical fracture line, with angulation. This injury does not have anteroposterior translation. Type III injuries have unilateral or bilateral facet dislocation with translation and are very unstable. Immediate application of halo traction is used to reduce the facet dislocation. 2
Question 3
A. Correct! Rigid cervical collar for 4–6 weeks. A type I fracture is stable and will usually heal with a rigid cervical collar.
Other choices and discussion
B, C. These treatments can be used for type II fractures, depending on the amount of displacement. Displacement of > 5 mm will likely need internal fixation.
D. This is usually used for type IIA injures.
References
1. Mirvis SE, Young JW, Lim C, Greenberg J. Hangman’s fracture: radiologic assessment in 27 cases. Radiology 1987;163(3):713–717 2. Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am 1985;67(2):217–226Top Tips
Type I injuries are stable injuries, and type III injuries are grossly unstable. 2
Type I and type II injuries cause widening of the spinal canal, which decreases the chance of neurologic compromise, although neurologic deficits sometimes do occur.
Although not specifically discussed in this case, dens fractures and mimics are also important to know. See the following:
Essentials 9
Questions
1. What is the most common mechanism for this type of injury?
A. Axial compression
B. Anteroposterior flexion
C. Anteroposterior extension
D. Rotational
E. Craniocaudal distraction
2. What is the most important factor in determining stability for the injury in the test case?
A. Alar ligament integrity
B. Transverse ligament integrity
C. Anterior longitudinal ligament integrity
D. Tectorial membrane integrity
E. Apical ligament integrity
3. An unstable C1 burst fracture is demonstrated by a sum of the lateral mass displacement of greater than:
A. 5 mm
B. 6 mm
C. 7 mm
D. 8 mm
E. 9 mm
Answers and Explanations
Question 1
A. Correct! Axial loading from a fall onto the head is the most common mechanism for this injury. Other common causes include motor vehicle collision or heavy object falling onto the head. Due to the angulation of the articular surfaces of the lateral masses, fractures and splaying of the anterior and/or posterior arch commonly occur with this mechanism. 1 In the image provided, there is a fracture of the anterior arch of C1 extending into the left lateral mass. The lateral mass is displaced laterally. There is also a fracture of the posterior arch of C1.
Other choices and discussion
B. Anteroposterior flexion usually leads to distraction injury of the subaxial cervical spine in a step-wise fashion. This includes the supraspinous ligament, interspinous ligament, facet capsular joint, ligamentum flavum, and the posterior longitudinal ligament. If the injury continues, it can cause either a fracture of the vertebral body (e.g., in the case of “flexion teardrop” injury, when a component of compression is present) or it can disrupt the disk and anterior longitudinal ligament.
C. Anteroposterior extension is not the most common mechanism. However, hyperextension can cause fractures of the C1 posterior arch. The first reported case of this type of injury involved Sir Geoffrey Jefferson as the treating physician. On a misty morning in 1919, a pilot crashed into telegraph wires and was thrown from his plane. Dr. Jefferson described the resultant segmental fracture of the posterior arch, and the fracture was later named after him.
D. Rotational injuries are usually described as atlantoaxial rotatory fixation, traumatic isolation of the articular pillar, and unilateral interfacetal dislocation. These patients are unable to return their head from a rotated to a neutral position. 2
E. Craniocaudal distraction injury may occur at any level, but is most frequently found at the craniocervical junction, with craniocervical dissociation/dislocation and widening of the occipital condyle-C1 articulation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree