SECTION V GENITOURINARY IMAGING
Essentials 1
Questions
1. Which ONE of the following is the correct diagnosis?
A. Myelolipoma
B. Angiomyolipoma
C. Liposarcoma
D. Renal cell carcinoma
2. The left renal mass measures 5.3 cm maximally. What is the MOST appropriate treatment?
A. Conservative management with 6-month follow up imaging
B. None, as this lesion is benign
C. Embolization/ablation
D. Surgical excision
3. With which syndrome are AMLs associated?
A. Tuberous sclerosis (TS)
B. Von Hippel-Lindau
C. Neurofibromatosis 2
D. Birt-Hogg-Dube
Answers and Explanations
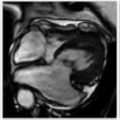
Question 1
B. Correct! This is an angiomyolipoma (AML). Images demonstrate a lesion containing macroscopic fat arising from the lateral aspect of the left kidney. Macroscopic fat typically demonstrates loss of signal on fat-suppressed images. Microscopic fat does not demonstrate loss of signal on fat-suppressed images; rather, it exhibits a loss of signal between in- and out-of-phase chemical shift imaging. The components of an AML include blood vessels (angio), smooth muscle (myo), and fat (lipoma).
Other choices and discussion
A. A myelolipoma is typically a macroscopic fat-containing lesion of the adrenal gland. In this case, the lesion clearly arises from the kidney. Note the “claw” sign. The “claw” represents normal renal parenchyma around the lesion, suggesting the organ of origin.
C. In this anatomic region, liposarcomas generally arise from the retroperitoneum and exert mass effect on the kidney. They rarely arise de novo from the kidney. Liposarcomas are usually hypovascular. The key to making the diagnosis of liposarcoma is determining that the site of origin is the retroperitoneum rather than the kidney.
D. Although 5% of RCCs contain fat, that fat is usually microscopic. Sonographically, however, AML and RCC may be indistinguishable. In some challenging cases, a lipid-poor AML may be indistinguishable from RCC with any type of imaging, and surgery may be indicated to exclude RCC.
Question 2
C. Correct! Embolization/ablation is recommended. The greatest risk for an AML is hemorrhage. The risk increases when the lesion reaches 4 cm in size or when the patient is pregnant.
Other choices and discussion
A. Conservative management with imaging is acceptable if the lesion is small (< 4 cm) and the patent is asymptomatic.
B. This lesion is benign but its size warrants treatment.
D. This lesion is usually successfully treated with embolization and ablation, which have lower risks than surgery.
Question 3
A. Correct! Renal AMLs are associated with TS. TS, also known as Bourneville disease, is a neurocutaneous disorder. A total of 20% of all AMLs are associated with TS, and up to 75% of individuals with TS have AMLs. When associated with TS, AMLs tend to be bilateral and multiple. Classically, TS is associated with the triad of mental retardation, seizures, and adenoma sebaceum. However, that classic triad is often absent. Other manifestations of TS include facial angiofibromas, cortical/subcortical tubers, subependymal giant cell astrocytomas, lymphangiomyomatosis of the lungs, and cardiac rhabdomyomas. This disorder is inherited in an autosomal dominant fashion but can be sporadic.
Other choices and discussion
B. Von Hippel-Lindau is associated with multiple renal/liver/pancreatic cysts as well as clear cell–type RCC. There is an increased risk of pheochromocytoma, papillary cystadenoma of the epididymis, and pancreatic neoplasms (serious cystadenoma and islet cell tumors). There is an association with central nervous system hemangioblastomas and retinal angiomas. This disorder can be inherited (autosomal dominant) or sporadic.
C. Neurofibromatosis 2 is an autosomal dominant condition classically associated with multiple schwannomas, meningiomas, and ependymomas.
D. Birt-Hogg-Dube syndrome is an autosomal dominant multisystem disease involving the kidneys, skin, and lung. It is characterized by multiple bilateral renal tumors (chromophobe/clear cell RCC and oncocytoma), multiple lung cysts (with an increased risk of spontaneous pneumothorax), and cutaneous lesions (papules and angiofibromas).
Suggested Readings
Bharwani N, Christmas TJ, Jameson C, et al. Epithelioid angiomyolipoma: imaging appearances. Br J Radiol 2009;82: e249–252 Hidalgo J, Chéchile G. Familial syndromes coupling with small renal masses. Adv Urol 2008. Israel GM, Hindman N, Hecht E, et al. The use of opposed-phase chemical shift MRI in the diagnosis of renal angiomyolipomas. Am J Roentgenol 2005;184:1868–1872 Jinzaki M, Tanimoto A, Narimatsu Y, et al. Angiomyolipoma: imaging findings in lesions with minimal fat. Radiology 1997;205:497–502 Maclean DF, Sultana R, Radwan R, et al. Is the follow-up of small renal angiomyolipomas a necessary precaution? Clin Radiol 2014;69:822–826 Sherman JL, Hartman DS, Friedman AC, et al. Angiomyolipoma: computed tomographic-pathologic correlation of 17 cases. Am J Roentgenol 1981;137:1221–1226Top Tips
A macroscopic fat-containing lesion of the kidney is essentially diagnostic of an AML.
AML > 4 cm should be treated (by embolization/ablation, or less often, partial nephrectomy) because of the risk of hemorrhage.
Make sure to confirm that the macroscopic fat-containing lesion arises from either the kidney or the adrenal. If not, retroperitoneal liposarcoma must be considered.
Essentials 2
Case
A 19-year-old woman presents with chronic dull pelvic pain. The low density portion of the adnexal mass has a hounsfield unit of −53.

Questions
1. Which ONE of the following is the MOST likely diagnosis?
A. Hemorrhagic cyst
B. Endometrioma
C. Mature ovarian teratoma
D. Ovarian serous cytadenoma
2. What is the MOST likely complication associated with this test case?
A. Malignant transformation
B. Hemorrhage
C. Ovarian torsion
D. Rupture
3. What entity is the rounded hyperechoic structure within the mass on the ultrasound image?
A. Rokitansky nodule
B. Calcification
C. Retracted clot
D. Fat
Answers and Explanations
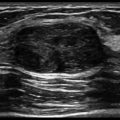
Question 1
C. Correct! This is a teratoma. A mature teratoma is a slowly growing ovarian tumor having at least two of the three germ cell layers. In this case, the computed tomography (CT) demonstrates fat density (matching the density of the surrounding pelvic fat) and soft tissue density. Although CT and magnetic resonance imaging are excellent at diagnosing a teratoma, ultrasound is the modality of choice because of its convenience, lack of ionizing radiation, and high accuracy. Ultrasound typically demonstrates a cystic adnexal mass with mural components, often including an echogenic mass with posterior shadowing.
Other choices and discussion
A. A hemorrhagic cyst would not demonstrate fat on CT. On ultrasound, a hemorrhagic cyst appears as a complex cyst with internal blood products. Acute blood is hyperechoic and becomes increasingly hypoechoic over time.
B. An endometrioma would not demonstrate fat on CT. Its appearance on ultrasound can mimic that of a hemorrhagic cyst.
D. Ovarian serous cystadenomas do not contain fat. They tend to be cystic, large, and often bilateral. In addition, they are more common in older women.
Question 2
C. Correct! Torsion is the most common complication of a teratoma, occuring in 5 to 15% of cases. For this reason, these masses are often resected when they are large. The risk of torsion increases once the ovary reaches 5 cm in size.
Other choices and discussion
A. The rate of malignant transformation is < 2%. It can occur in any of the three germ cell layers (ectoderm, mesoderm, and endoderm). Squamous cell carcinoma arising from the lining of the cyst is the most common type. Factors associated with malignant transformation of a dermoid include patient age > 45 years, tumors > 10 cm, elevated serum tumor markers, and a predominantly enhancing soft tissue component.
B. Hemorrhage is a rare complication.
D. Rupture is a rare complication (1 to 4% of patients). Infection is also a rare complication.
Question 3
A. Correct! This is a Rokitansky nodule, which is also referred to as a dermoid plug. It is typically composed of hair, dermal elements, teeth, and/or sebacious material. A Rokitansky nodule has an echogenic and nodular appearance on ultrasound.
Other choices and discussion
B. Calcification can contribute to (but is not the only component of) the Rokitansky nodule.
C. If the lesion were simply a cyst with blood products, a retracted clot would be the correct choice. However, the additional elements shown on CT confirm a teratoma.
D. Fat can contribute to (but is not the only component of) the Rokitansky nodule.
Suggested Readings
Friedman AC, Pyatt RS, Hartman DS, et al. CT of benign cystic teratomas. Am J Roentgenol 1982;138:659–665 Outwater EK, Siegelman ES, Hunt JL. Ovarian teratomas: tumor types and imaging characteristics. Radiographics 2001;21:475–490 Patel MD, Feldstein VA, Lipson SD, et al. Cystic teratomas of the ovary: diagnostic value of sonography. Am J Roentgenol 1998;171:1061–1065Top Tips
Mature teratomas are common, slowly growing ovarian neoplasms that contain at least two of the three germ cell layers.
Ultrasound is the modality of choice for teratoma and can usually make the definitive diagnosis. Typically, there is an echogenic component, shadowing, and a fluid-fluid level.
Several useful ultrasound signs for teratoma: The “tip of the iceberg” sign refers to the echogenic structures within the lesion obscuring deeper portions because of poor sound penetration. The “dot-dash” sign refers to multiple thin echogenic bands due to hair within the cystic lesion.
Essentials 3
Questions
1. What is the correct diagnosis?
A. Bowel perforation
B. Intraperitoneal bladder rupture
C. Extraperitoneal bladder rupture
D. Rupture of a hemorrhagic cyst
2. What is the MOST appropriate management?
A. Close observation with serial imaging
B. Surgery with bladder repair
C. Radical cystectomy
D. Foley catheter placement
3. What is the MOST appropriate way to instill contrast solution for a voiding cysturethrogram on a trauma patient?
A. Manually inject 100 mL by hand into the Foley catheter.
B. Power inject 300 mL into the Foley catheter.
C. By gravity, use a bag raised above the patient with a volume of 300 mL (or until the patient can tolerate).
D. Inject contrast intravenously and wait for its excretion into the urinary bladder.
Answers and Explanations
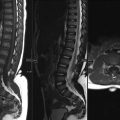
Question 1
B. Correct! This is an intraperitoneal bladder rupture. The initial images demonstrate thickening of the superior bladder wall with adjacent fluid, and the delayed images demonstrate contrast surrounding loops of bowel with tracking into the paracolic gutters. Intraperitoneal bladder rupture represents 10 to 20% of all bladder injuries. It occurs with individuals that sustain a direct blow to a distended urinary bladder. On imaging, extravasated contrast insinuates between bowel loops. This is known as a type 2 injury by cystography.
Other choices and discussion
A. There is no evidence of bowel injury. The density of the contrast within the abdomen on the delayed images matches that in the ureter, confirming its origin from the urinary system/bladder. Additionally, there is no oral contrast on these images. The standard computed tomography protocol for blunt abdominal trauma is computed tomography of the abdomen and pelvis with intravenous contrast but no oral contrast.
C. Extraperitoneal bladder rupture is the most common type of bladder injury (80 to 90%). It is most often associated with pelvic fractures or penetrating trauma. Extravasated contrast tends to accumulate within the prevesicle space (also known as the retropubic space or space of Retzius). This is known as a type 4 injury by cystography.
D. A ruptured hemorrhagic cyst would not produce such extensive and dense fluid throughout the abdomen. Furthurmore, this would not account for the irregular morphology of the bladder on the coronal image.
Question 2
B. Correct! Intraperitoneal bladder rupture requires surgery. Given the risk of chemical peritonitis, there is significant potential morbidity if the defect is not surgically corrected.
Other choices and discussion
A. Conservative management is only appropriate for extraperitoneal bladder rupture.
C. Radical cystectomy is a drastic measure and represents major surgery. In most cases, the urinary bladder is salvagable following trauma.
D. An indwelling Foley catheter is the treatment for extraperitoneal bladder rupture.
Question 3
C. Correct! The gravity method allows the least traumatic direct entry for contrast. Contrast administration should stop when the patient feels full or can no longer tolerate the instillation.
Other choices and discussion
A. Manually injecting contrast is too intrusive and may cause additional injury/discomfort.
B. Power injecting contrast is too intrusive and may cause additional injury/discomfort.
D. The indirect method of intravenous contrast administration would not ensure optimal urinary bladder filling, and a significant finding might potentially be missed.
Suggested Readings
Ramchandani P, Buckler PM. Imaging of genitourinary trauma. Am J Roentgenol 2009;192:1514–1523 Vaccaro JP, Brody JM. CT cystography in the evaluation of major bladder trauma. Radiographics 2000;20:1373–1381Top Tips
Computed tomography cystography or voiding cysturethrogram are the studies of choice to diagnose a bladder rupture. Plain film may demonstrate a “pear-shaped bladder.”
Intraperitoneal bladder rupture: caused by blunt force or penetrating trauma to a full bladder; requires surgical repair.
Extraperitoneal bladder rupture: caused by adjacent pelvic fracture; can be treated conservatively.
Driving with a full bladder places one at an increased risk for a bladder injury. Void first!
Essentials 4
Questions
1. Imaging features of this lesion are classic for which entity?
A. Multilocular cystic nephroma
B. Hemorrhagic cyst
C. Renal cell carcinoma
D. Oncocytoma
2. What Bosniak category does this lesion fall into?
A. Bosniak 1
B. Bosniak 2
C. Bosniak 3
D. Bosniak 4
3. What is the standard management for this test case?
A. Observation
B. Resection
C. Embolization
D. Further imaging
Answers and Explanations
Question 1
A. Correct! This is the classic appearance for a multilocular cystic nephroma. Multilocular cystic nephroma (MLCN) is typically encapsulated, T2 hyperintense, herniates into the renal pelvis, and has variable septal enhancement. This lesion has a bimodal age distribution which includes young men and middle-aged women.
Other choices and discussion
B. Hemorrhagic cysts are typically homogenously T1 hyperintense and nonenhancing.
C. This could represent a cystic RCC. Although it does have the the classic appearance of a MLCN, RCC is much more common than MLCN. These two lesions are often difficult to differentiate by imaging, and both lesions are often resected.
D. Oncocytomas are large, well-demarcated lesions that are less cystic than the test case. They classically have a nonenhancing central stellate scar (which is T2 hypointense), a finding seen in 30% of cases. Relatively homogeneous enhancement is common. Oncocytomas can be multiple and bilateral. There is also an association of oncocytomas with tuberous sclerosis and Birt-Hogg-Dube.
Question 2
C. Correct! This is Bosniak 3. Bosniak 3 lesions are indeterminate for malignancy and usually require resection or ablation. Key findings of Bosniak 3 lesions include thick/nodular septa and a wall with measurable enhancement (both are seen here). Malignant potential is 55%.
Other choices and discussion
A. Boniak 1 lesions are simple cysts with imperceptible walls. There is no malignant potential, and follow up is not necessary.
B. Bosniak 2 lesions are minimally complex cysts. These include hemorrhagic cysts < 3 cm, cysts with few thin septations (< 1 mm), and cysts with thin calcifications. There is no malignant potential, and follow up is not necessary.
Bosniak 2F lesions are slightly more complex cysts. These include hemorrhagic cysts > 3 cm in size, an increased number of (or minimal thickening of) septa, and nodular or thickened calcifications, but still no measurable contrast enhancement. The malignant potential is 5%. These require follow up at 6 months.
D. Bosniak 4 lesions are clearly malignant. These includes cysts with a solid-enhancing nodule or mass.
Question 3
B. Correct! Resection is the treatment of choice.
Other choices and discussion
A. While this entity is benign, it is not readily distinguished from RCC by imaging, and observation could be a mistake.
C. Embolization is not the standard of care. If performed, embolization is generally reserved for small tumors. One drawback of embolization is that it would probably require multiple treatments, thus prolonging the time period for therapy. In addition, because malignancy is not definitively excluded by imaging, resection is indicated.
D. Further imaging would not result in a more definitive diagnosis.
Suggested Readings
Israel GM, Bosniak MA. How I do it: evaluating renal masses. Radiology 2005;236:441–450 Madewell JE, Goldman SM, Davis CJ, et al. Multilocular cystic nephroma: a radiographic-pathologic correlation of 58 patients. Radiology 1983;146:309–321 Palmer WE, Chew FS. Renal oncocytoma. Am J Roentgenol 1991;156:1144 Silver IM, Boag AH, Soboleski DA. Best cases from the AFIP: Multilocular cystic renal tumor: cystic nephroma. Radiographics 2008;28:1221–1225Top Tips
Multilocular cystic nephroma is a benign lesion that is often difficult to distinguish from RCC in adults and from Wilms tumor in children.
Bimodal distribution of MLCN: young men (< 5 years old) and women in the fifth and sixth decades of life.
MLCN imaging: multiloculated cystic lesion, well encapsulated, septations with variable enhancement, often herniating into the renal pelvis.
Essentials 5
Questions
1. What is the correct diagnosis?
A. Bartholin gland cyst
B. Skene gland cyst
C. Urethral diverticulum
D. Gartner duct cyst
2. What is the MOST important magnetic resonance imaging (MRI) sequence for making this diagnosis?
A. T2-weighted sequence
B. T1-weighted sequence
C. Contrast-enhanced T1-weighted sequence
D. Diffusion-weighted imaging
3. What type of cancer MOST commonly arises within a urethral diverticulum?
A. Transitional cell carcinoma
B. Adenocarcinoma
C. Squamous cell carcinoma
D. Small cell carcinoma
Answers and Explanations
Question 1
C. Correct! The patient has a urethral diverticulum. These occur posterolateral to the urethra and above the level of the pubic symphysis. They can grow and surround the ureter posteriorly (“Saddlebag” morphology), as in this case. Symptoms include dysuria, dribbling, and dysparunia (the 3 Ds) as well as urinary frequency and urgency. A connection to the urethral lumen is demonstrated in most cases.
Other choices and discussion
A. Bartholin gland cysts typically occur posterior to the lower vagina and below the level of the pubic symphysis. They are associated with the labia majora and result from chronic inflammation leading to ductal obstruction. These cysts are usually asymptomatic but may require drainage due to superimposed infection.
B. Skene gland cysts are rentention cysts that form secondary to inflammation/obstruction of the paraurethral ducts. These are typically located lateral to the external urethral meatus and below the level of the pubic symphysis. Skene gland cysts are usually asymptomatic but may require drainage or excision due to superimposed infection.
D. Gartner duct cysts typically occur anterior to the superior vagina and above the level of the inferiormost aspect of the pubic symphysis. They result from the incomplete regression of the wolffian ducts. When Gartner duct cysts are located at the level of the urethra, they can cause mass effect on the urethra, giving rise to urinary tract symptoms.
Question 2
A. Correct! T2 is the MRI sequence of choice and should be obtained in all three planes. T2 is the most sensitive for the detection of small cystic lesions. MRI is the current test of choice for the diagnosis of urethral diverticulum. Historically, either contrast-enhanced radiography (voiding cystourethrography or double-balloon urethrography) or fiberoptic urethroscopy were used to make the diagnosis. However, these methods are invasive, difficult to perform, and uncomfortable for the patient. Additionally, if the urethral diverticulum contains hemorrhage, pus, or stones, the diverticulum may be missed.
Other choices and discussion
B. T1-weighted sequence is less sensitive than T2 for the detection of small cystic lesions. However, T1 is useful in detecting the sometimes-found internal hemorrhage.
C. Postcontrast images are less sensitive than T2 for making this diagnosis. However, contrast is useful in detecting underlying inflammation, infection, or malignancy.
D. Diffusion-weighted imaging is not the sequence of choice. However, diffusion-weighted imaging is to supplement the detection of underlying infection/malignancy.
Question 3
B. Correct! Adenocarcinoma is the most common cancer type to arise within a urethral diverticulum. Note that the overall incidence of malignancy within a diverticulum is low. Adenocarcinoma also occurs within urachal remnants and diverticula.
Other choices and discussion
A. Transitional cell carcinoma is the most common cell type in the genitourinary tract and is found most commonly within the bladder, urethra, and ureters.
C. Sqamous cell carcinoma is not common within the genitourinary tract. About 5% of bladder cancers are of squamous cell origin.
D. Small cell carcinoma is not common within the genitourinary tract.
Suggested Readings
Chou CP, Levenson RB, Elsayes KM, et al. Imaging of female urethral diverticulum: an update. Radiographics 2008;28: 1917–1930 Hahn WY, Israel GM, Lee VS. MRI of female urethral and periurethral disorders. Am J Roentgenol 2004;182:677–682 Patel AK, Chapple CR. Female urethral diverticula. Curr Opin Urol 2006;16:248–254 Siegelman ES, Outwater EK, Banner MP, et al. High-resolution MR imaging of the vagina. Radiographics 1997;17:1183–1203Top Tips
A urethral diverticulum should be distinguished from other cystic lesions of the lower female pelvis by its location, which is superior to the bottom of the pubic symphysis and posterior to the urethra.
T2 is the most sensitive MRI sequence for detection of a urethral diverticulum (or other cystic lesions of the female pelvis).
Adenocarcinoma is the most common malignancy in both urethral diverticula and urachal remnants. Transitional cell carcinoma is the most common malignancy in the remainder of the urinary tract.
Essentials 6
Questions
1. What is the MOST likely cause for this patient’s hematuria?
A. Renal calculus
B. Blood clot
C. Transitional cell carcinoma
D. Renal cell carcinoma
2. Which ONE of the following is a risk factor for the development of the diagnosis in the test case?
A. Smoking
B. Alcohol
C. Infection
D. Intravenous iodinated contrast
3. Metachronous tumors of the urinary tract are most common with:
A. Bladder transitional cell carcinoma
B. Upper urinary tract transitional cell carcinoma
C. Urethral transitional cell carcinoma
D. Renal cell carcinoma
Answers and Explanations
Question 1
C. Correct! This is a case of transitional cell carcinoma (TCC). This is the classic appearance of a ureteral tumor by plain film urography, with the formation of a meniscus or a “goblet” sign. The lack of upstream ureteral dilatation suggests that this process developed slowly. TCC is most commonly found in an older population (average age of 65) with a 4:1 predilection for males. A total of 96% of cases are found in the urinary bladder, 3% in the renal pelvis, and 1% in the ureter. These tumors are usually characterized as either papillary or nonpapillary.
Other choices and discussion
A. Renal calculus is unlikely given lack of upstream dilation, which would be expected with a stone of this size. In addition, this stone would have to be radiolucent, and a stone would not produce the meniscus effect seen here.
B. A blood clot of this size would be expected to cause upstream dilatation of the collecting system.
D. RCC is extremely rare in the ureter.
Question 2
A. Correct! Risk factors and industrial exposures linked to TCC cancer development include smoking, certain amine and phenyl dyes, cyclophosphamide, phenacetin, and aristolochic acid (Balkan nephropathy).
The other choices are all incorrect.
Question 3
B. Correct! Metachronous tumors of the urinary tract are more common with upper urinary tract TCC. Metachronous tumors are those that occur at different times. Approximately 40% of patients with upper urinary tract TCC will develop additional sites of tumor distally (usually in the bladder). The surgical treatment of choice for an upper tract TCC (involving the kidney or ureter) is a nephroureterectomy (where the ipsilateral kidney and ureter are removed).
Other choices and discussion
A. Only 2 to 4% of patients with bladder TCC develop tumor elsewhere within the urinary tract. Surgical treatment for bladder TCC typically consists of radical cystectomy with ileal conduit formation. (The bladder is first removed. Then a portion of the ileum is removed and connected to the ureters to serve as the urinary bladder.) The conduit drains through an ostomy.
C. Urethral TCC is extremely rare. Most carcinomas of the urethra are squamous cell.
D. There is an increased risk of metachronous RCC in patients von Hippel-Lindau disease, patients diagnosed with RCC before the age of 40, and patients with familial RCC.
Suggested Readings
Browne RF, Meehan CP, Colville J, et al. Transitional cell carcinoma of the upper urinary tract: spectrum of imaging findings. RadioGraphics 2005;25:1609–1627 Kawashima A, Goldman SM. Neoplasms of the renal collecting system, pelvis and ureters. In: Pollack HM, McClennan BL, Dyer RB, Kenney PJ, eds. Clinical Urography. New York, NY: Saunders; 2000:1560–1641 Vikram R, Sandler CM, Ng CS. Imaging and staging of transitional cell carcinoma. Lower urinary tract. Am J Roentgenol 2009;192:1481–1487Top Tips
TCC is the most common tumor of the urinary tract and occurs most frequently in the bladder.
Upper TCC is more prone to metachronous lesions than bladder TCC. The surgical treatment differs depending on the site of disease.
In the ureter, look for the “goblet” sign when differentiating from a calculus. TCC may variably result in obstruction.
Essentials 7
Questions
1. Which ONE of the following is the MOST likely cause for these imaging findings?
A. Ureterovesical stone
B. Duplex kidney
C. Congenital megaureter
D. Renal sinus cyst
2. In a duplicated collecting system, which system typically refluxes and which system obstructs?
A. Upper pole both obstructs and refluxes
B. Lower pole obstructs and upper pole refluxes
C. Upper pole obstructs and lower pole refluxes
D. Lower pole both obstructs and refluxes
3. What is the MOST accurate way to diagnose this condition?
A. Ultrasound
B. Multiphase CT
C. Portal venous phase CT
D. Intravenous pyelogram
Answers and Explanations
Question 1
B. Correct! This is a duplex kidney. The first image demonstrates a cystic structure in the left upper pole, which is contiguous with the dilated ureter seen on the magnetic resonance urogram (second image). There is also focal atrophy at the upper pole of the left kidney. This atrophy is the result of chronic obstruction. The remaining lower portion of the kidney is normal and has a nondilated collecting system. These are all typical findings of a duplicated collecting system with two ureters. The visible ureter is dilated and extends from the upper pole moiety. The ureter of the lower pole moiety is not visible. A duplicated system is one of the most common congenital renal anomalies. The extent of duplication is on a spectrum. It may be a simple as duplication of only the renal pelvis, draining with a single ureter, or two distinct collecting systems that drain into the bladder. When the latter occurs, the anatomy usually follows the Weigert-Meyer rule (see below). Duplication is seen in 0.7% of the population, and mild forms are often overlooked with imaging. Most cases are asymptomatic, but complications of infection, obstruction, and reflux sometimes occur.
Other choices and discussion
A. If a left ureterovesical junction stone were to cause this degree of ureteral dilatation, atrophy of the entire kidney would be expected. Additionally, given lack of perinephric edema, this process appears to be chronic.
C. A congenital megaureter could be the answer, if a normal collecting system wasn’t visualized in the lower portion of the left kidney. A true primary congenital megaureter is related to a distal adynamic segment with proximal dilatation. This is analogous to primary achalasia in the esophagus. This entity is often diagnosed in children. This can rarely be associated with congenital megacalyces. Vesicoureteric reflux can also result in ureteral dilatation.
D. The cystic structure in the first image is a part of the dilated collecting system. A renal sinus cyst does not connect to the renal pelvis and collecting system.
Question 2
C. Correct! The upper pole obstructs and lower pole refluxes. According to the Weigert-Meyer law, the lower pole ureter inserts orthotopically (in its normal location), and the upper pole ureter inserts ectopically, inferiorly, and medially relative to the lower pole ureter. The ectopic insertion is often associated with a ureterocele, which can cause obstruction of the upper pole moiety. There is often distortion of the ectopic ureter insertion, resulting in reflux. On pyelogram, sometimes only the lower pole opacifies (due to upper pole obstruction). Mass affect from the dilated upper pole forms the classic “drooping lily” sign.
The other choices are incorrect.
Question 3
B. Correct! Use of contrast to confirm or exclude communication of the “cyst” with the collecting system is the best way to differentiate a renal sinus cyst from hydronephrosis. (A cystic structure filling with contrast that subsequently passes into the collecting system does not represent a renal sinus cyst.) In terms of which contrast study to select, the important point is to be able to compare precontrast to postcontrast, possibly including delayed imaging. Of the answer choices, multiphase CT is the best option.
A multiphase magnetic resonance imaging study is equally as effective as a contrast-enhanced CT for this purpose.
Note that a cystic structure in this region that opacifies could represent either hydronephrosis or a calyceal diverticulum, which also communicates with the collecting system. The morphology should be able to differentiate these choices.
Other choices and discussion
A. Renal ultrasound can often (but not always) differentiate parapelvic cysts from hydronephrosis.
C. A single phase of a contrast study can have limitations in making this diagnosis.
D. An intravenous pyelogram can demonstrate hydronephrosis and can often demonstrate deformities of the collecting system by adjacent renal sinus cysts, but the anatomic assessment is limited and intravenous pyelogram cannot demonstrate the cysts themselves.
Suggested Readings
Callahan MJ. The drooping lily sign. Radiology 2001;219: 226–228 Fernbach SK, Feinstein KA, Spencer K, et al. Ureteral duplication and its complications. Radiographics 1997;17:109–127 Lebowitz RL, Avni FE. Misleading appearances in pediatric uroradiology. Pediatr Radiol 1980;10:15–31Top Tips
Duplex kidney is a common congenital renal tract anomaly. The site and extent of duplication may vary.
With complete duplication of the collecting system, the two ureters insert separately (according to the Weigert-Meyer rule). The upper pole moiety ureter inserts ectopically, inferomedially to the orthotopic lower pole moiety ureter.
With a complete duplex system, the upper pole moiety obstructs, while the lower pole moiety refluxes.
Essentials 8
Questions
1. Which ONE of the following is the correct diagnosis?
A. Crossed fused renal ectopia
B. Duplicated right renal collecting system
C. Horseshoe kidney
D. Low-lying right kidney
2. In this test case, where is the left ureter likely inserting into the urinary bladder?
A. Inferiorly from the right ureteral insertion
B. Together with the right ureter at its insertion
C. Orthotopically
D. Superior to the right ureteral insertion
3. Unilateral renal agenesis is commonly associated with which of the following? Choose ALL that are correct.
A. Caroli disease
B. Chromosomal anomalies
C. Müllerian duct anomalies
D. Budd-Chiari syndrome
Answers and Explanations
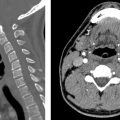
Question 1
A. Correct! The kidneys are not in their expected location on these images, and a fused kidney is seen in the right lower quadrant. This is the characteristic appearance of crossed-fused renal ectopia. Computed tomography depicts the parenchymal band connecting the kidneys. Potential complications of this anomaly include nephrolithiasis, infection, and hydronephrosis. Crossed fused renal ectopia results from abnormal renal ascent in embryogenesis. Normally by the eighth week of life, the kidneys reach their appropriate position at the L2 level.
Other choices and discussion
B. A duplicated collecting system would not explain both the absence of a contralateral kidney and the pelvic kidney location.
C. A horseshoe kidney refers to fusion of both kidneys (either with a parenchymal or a fibrous band) with the respective kidneys remaining on their own side. With a horseshoe kidney, the inferior pole of each kidney is medially positioned while the superior pole is laterally positioned. This is the reverse of normotopic kidneys.
D. While the right kidney is low lying, a pelvic kidney is an incomplete diagnosis. Additionally, this would not account for the fusion of the kidneys.
Question 2
C. Correct! The abnormally fused kidney’s ureter inserts into its normal location (orthotopically); in this case, on the left side of the bladder.
Other choices and discussion
A. An inferior insertion of the ureter may be seen with a duplicated renal collecting system.
B. A fused insertion with the right ureter might occur along the spectrum of a duplicated collecting system.
D is incorrect.
Question 3
B. Correct! Renal agenesis can be association with a number of chromosomal anomalies, including Down syndrome and Turner syndrome.
C. Correct! Unilateral renal agenesis is commonly associated with müllerian duct anomalies.
Renal agenesis results from absence of induction of the metanephros by the ureteral bud at 6 to 7 weeks gestation. The metanephros becomes the adult kidney, and absence of its formation results in the complete absence of the structure. The metanephros is also important for normal internal genital formation, explaining the association of renal anomalies with wolffian and müllerian duct anomalies. In the absence of a kidney, always check the pelvic structures, as uterine anomalies in females and ipsilateral seminal vesicle agenesis in males are commonly associated. Adrenal agenesis is extremely rare and can be associated with renal agenesis.
Other choices and discussion
A. Caroli disease is a congenital disorder with multifocal cystic dilatation of the segmental intrahepatic bile ducts. It is associated with autosomal recessive and autosomal dominant polycystic kidney disease as well as medullary sponge kidney.
D. Budd-Chiari is hepatic venous obstruction and is not associated with renal agenesis.
Suggested Readings
Bauer BS. Anomalies of form and fusion, crossed renal ectopia with and without fusion. In: Alan J, ed. Wein: Campbell-Walsh Urology Book. 9th ed. Philadelphia: WB Saunders; 2007:3269–3304 Dyer RB, Chen MY, Zagoria RJ. Classic signs in uroradiology. Radiographics 2004;24(suppl 1):S247–280 Gay SB, Armistead JP, Weber ME, et al. Left infrarenal region: anatomic variants, pathologic conditions, and diagnostic pitfalls. Radiographics 1991;11:549–570 Kaufman MH, Findlater GS. An unusual case of complete renal fusion giving rise to a “cake” or “lump” kidney. J Anat 2001;198:501–504Top Tips
After horseshoe kidney, cross-fused renal ectopia is the next most common congenital renal anomaly.
Differentiating between renal agenesis, a pelvic kidney, and an atrophic kidney has significant clinical relevance. A nuclear medicine renal scan can sometimes detect occult renal function.
Because of their embryologic origins, renal anomalies sometimes occur in association with pelvic genitalia anomalies. When you see one, make sure to check the other as well.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree