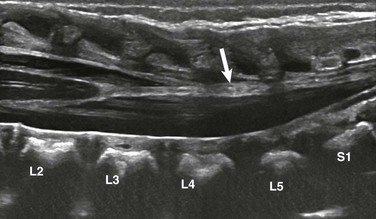
Chapter 41 Pediatric spinal cord imaging is a complex and interesting area that relies heavily on ultrasound in infants younger than 6 months of age and magnetic resonance imaging (MRI) thereafter.1,2 Other imaging modalities such as plain radiography, myelography, computed tomography (CT), and nuclear scintigraphy serve a limited role but can provide useful adjunctive information in cases with a specific question. Radiographic spine series typically include frontal and lateral radiographs of the cervical, thoracic, or lumbar region. Additional oblique radiographs may be added depending on the clinical indication. Plain radiographs have limited utility as a primary imaging tool in the evaluation of spinal cord but may demonstrate indirect evidence of underlying cord abnormalities and prompt performance of additional cross-sectional imaging. Nowhere else is this more true than in the setting of acute trauma.3 Although some studies have concluded that CT should be the initial study in acute trauma screening, radiography continues to be the mainstay for screening patients with trauma. Radiography also may be performed to screen older children with various spine-related complaints such as chronic back pain and torticollis. Subtle findings such as posterior vertebral body scalloping, widening of the neural foramina, or widening of the central canal may suggest underlying pathology (Fig. 41-1).4 Figure 41-1 A cervical cord astrocytoma on a plain radiograph and magnetic resonance imaging in a 1-year-old girl with persistent torticollis. Contrast radiography is a term that includes angiography with biplane and triplane fluoroscopy and conventional myelography. As with plain radiography, contrast radiography has a limited role in the evaluation of spinal cord pathology. Largely, conventional myelography has been supplanted by MRI. CT myelography is useful in rare, specific clinical circumstances such as when patients cannot undergo MRI because of an implanted prosthesis, for example, cochlear implants or pacemakers.5 In such patients, myelography with or without CT can provide useful information about the spinal cord and thecal sac. The role of conventional angiography in pediatric spinal imaging is as a secondary or tertiary modality to define vascular anatomy in preparation for treatment of dural fistulas and arteriovenous malformations, both of which are extremely rare in children.2 Like plain and contrast radiology, CT plays a limited role in direct spinal cord imaging. However, CT has the advantages of speed, availability, improved contrast resolution compared with radiography, limited operator independence, and the capability for multiplanar and three-dimensional reformations. It provides superior sensitivity and specificity in delineating osseous anomalies compared with other modalities and can indicate the need for additional spinal cord imaging (Fig. 41-2).3 Finally, as previously stated, CT and CT myelography can be performed in children who are unable to undergo MRI, thus allowing identification and characterization of mass lesions, calcifications, and areas of hemorrhage.5 Figure 41-2 An epidural hematoma on computed tomography (CT) in a 15-year-old athlete with sudden arm pain and weakness. Ultrasonography is a well-established method for evaluation of the neonatal spinal canal and its contents.1,6 The predominately cartilaginous and incompletely ossified spinal arches in infants serve as a superb acoustic window for transmission of the ultrasound beam. However, with progressive ossification, the acoustic window diminishes, allowing limited visualization of the spinal cord between the spinous processes.6 Although this limited acoustic window persists into adulthood, the spinal cord becomes difficult to adequately visualize on a routine basis in infants older than 6 months of age.1 Spinal ultrasound is performed with a high-frequency 7- to 12-MHz linear-array transducer or 8- to 10-MHz curved-array transducer.1 Newborns undergo imaging while prone in the longitudinal (sagittal) and transverse (axial) planes from the craniocervical junction through the conus medullaris and cauda equina (Fig. 41-3). Paramedian scanning may be useful in some patients with partially ossified vertebra.1 The vertebral bodies are carefully numbered by counting down from either the lowest rib and/or the craniocervical junction, and numbering is confirmed by counting up from the lumbosacral junction.1,7 This dual technique of numbering allows one to avoid misdiagnosing a low-lying, possibly tethered spinal cord. Real-time cine loops are obtained routinely as part of the examination in order to demonstrate the normal rhythmic movement of the cauda equina nerve roots during the cardiac cycle.1
Spinal Cord Imaging Techniques
Plain Radiography
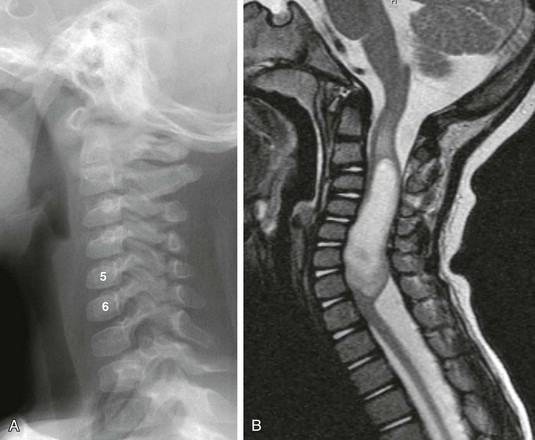
A, A lateral cervical spine radiograph shows subtle posterior vertebral body scalloping causing C5 and C6 to take on an abnormal square shape compared with the normal adjacent rectangular vertebral bodies. B, A sagittal T2-weighted magnetic resonance image confirms expansion of the cervical spinal canal because of a T2-hyperintense mass within the cervical cord. Note T2 bright cord edema above and below the mass.
Contrast Radiography
Computed Tomography
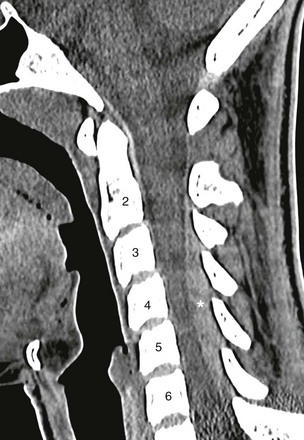
A sagittal cervical spine CT image demonstrates a posterior hyperattenuated fluid collection (asterisk) compressing the spinal cord from C3 to C6. Magnetic resonance imaging (not shown) was obtained for further evaluation and followed by surgical drainage.
Ultrasound
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine