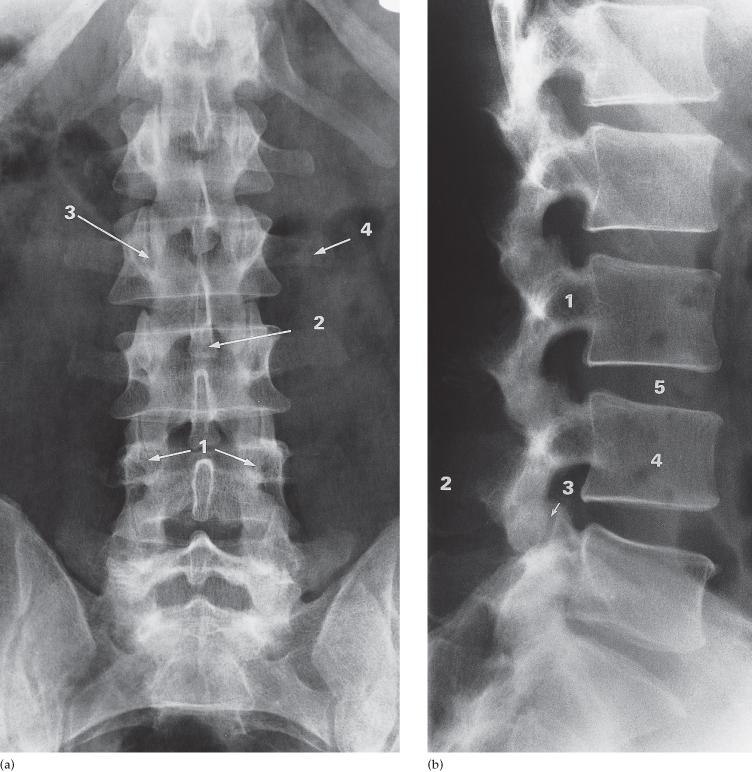
Fig. 13.2 Plain films of normal lumbar spine. (a) Frontal view. 1, pedicles; 2, spinous process; 3, facet joint; 4, transverse process. (b) Lateral view. 1, pedicles; 2, spinous process; 3, facet joint; 4, vertebral body; 5, disc space. Note how the height of the disc spaces increases from L1 to L5 with the exception of the L5/S1 disc space which is normally narrower than the one above.
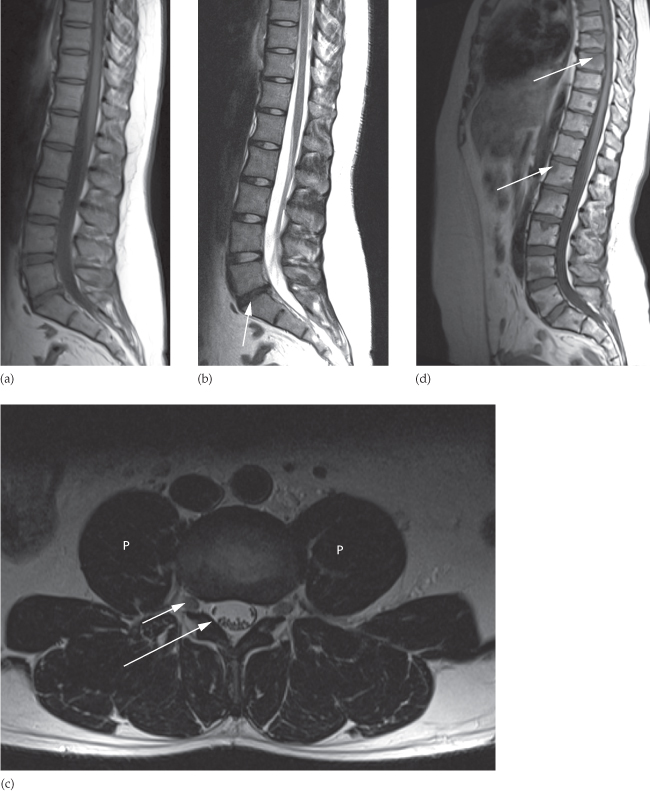
The appearances of a normal spine on MRI are illustrated in Fig. 13.3a–c. On both T1- and T2-weighted sequences, the signal from normal vetebrae is bright due to the fat content of bone marrow. Vertebral marrow should be of higher signal than the disc on a T1-weighted sequence otherwise it could indicate marrow replacement such as by metastatic disease (Fig. 13.3d). The intervertebral disc is composed of three main parts: the annulus fibrosis, which surrounds the central nucleus pulposus, and the cartilaginous endplates. On a T2-weighted scan, the CSF is of high signal with the spinal cord and nerve roots seen to pass to the exit foramina. The spinal cord extends from the cervicomedullary junction at the foramen magnum, and tapers inferiorly to become the conus medularis, which should be located no lower than the inferior border of L2. Extending inferiorly from the conus are the lumbar and sacral nerve roots which make up the cauda equina.
Fig. 13.3 MRI of the lumbar spine. (a) Normal T1-weighted scan. The discs and spinal cord are of intermediate signal. (b) Normal T2-weighted scan. The discs and CSF appear as high signal. The L5/S1 disc has lost height and is reduced in signal compared to the other discs, in keeping with degenerative changes (arrow). (c) Axial T2-weighted scan through the L3/L4 disc space. At this level, the L3 nerve roots are in the exit foramina (short arrow) and the L4 nerve roots have moved to the edge of the dural sac (long arrow) in the lateral recesses prior to exiting the spinal canal at the level below. p, psoas muscle. (d) Sagittal T1-weighted scan showing focal areas of low signal within multiple vertebral bodies (some marked with arrows) due to metastatic breast cancer.
At each level in the cervical region (C3–C7), the anterior and posterior roots extend laterally from the cord and pass into the anterolateral-orientated exit foramina and are named according to the pedicle they pass over (i.e. the C5 nerve exits the spine through the C4/C5 intervertebral foramen). Due to the presence of C8 nerves, beyond C7/T1 the nerves are named according to the pedicle they pass under (i.e. the T4 nerve exits the spine through the T4/T5 exit foramen). In the lumbar spine, the nerve roots run in the lateral recess of the lumbar canal across a disc level before exiting under the corresponding pedicle.
Radiographic Signs of Spinal Abnormality
There are some abnormalities detected on plain radiographs that often permit a diagnosis to be made, although other imaging will often be required for confirmation.
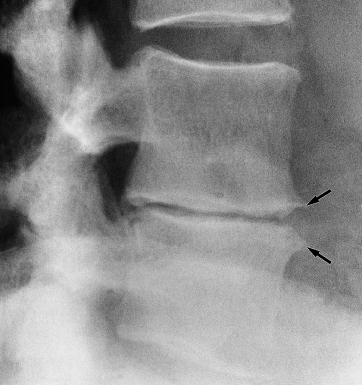
Disc Space Narrowing
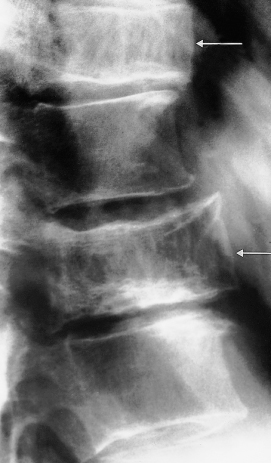
Normally, the disc spaces are the same height at all levels in the cervical and thoracic spine. In the lumbar spine, the disc spaces increase slightly in height going down the spine. A reduction in intervertebral height usually implies degenerative disc disease and may be associated with endplate sclerosis and osteophytes around the endplate margins (Fig. 13.4). A reduction in intervertebral space associated with poor visualization of the endplates may be seen in disc space infection.
Fig. 13.4 Disc space narrowing caused by disc degenerative changes between L3 and L4. Note the osteophytes (arrows) and sclerosis of the adjoining surfaces of the vertebral bodies.
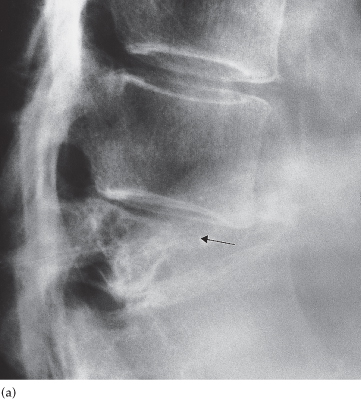
Collapse of Vertebral Bodies
A collapsed vertebral body is one that has lost height. This could be a normal bone subjected to abnormal stress such as in trauma or an abnormal weakened bone subjected to normal stress such as in metastases or myeloma. If any collapse is present, it is essential to look at the adjacent disc to see if it is narrowed, to check if part of any pedicle or cortical margin is destroyed and to assess the posterior vertebral wall to ensure that there is no compromise of the central spinal canal containing the cord or cauda equina.
Causes of vertebral collapse (Box 13.1) include:
- Metastases and myeloma. Bone destruction, or replacement of normal marrow by a lytic tumour, may be visible. The pedicles are a good place to look for evidence of bone destruction on plain film examination. The disc spaces are usually normal (Fig. 13.5a).
- Infection. The adjacent disc space is nearly always narrow or obliterated. There may be bone destruction next to the affected disc but the pedicles are usually intact (Fig. 13.5b).
- Osteoporosis. There is generalized reduction in bone density leading to compression fractures. The disc spaces are normal or even slightly increased in height and the pedicles are intact (Fig. 13.5d).
- Trauma. A compression fracture is commonly due to hyperflexion of the spine, causing the vertebral body to become wedge-shaped (Fig. 13.5c, d). The discs are normal but may be impacted into the fractured bone. Associated fractures may be seen in the pedicles or neural arch, but otherwise the bone and discs are normal.
- Eosinophil granuloma. Complete collapse of one or more vertebral bodies may occur in children or young adults with a solitary site of Langerhans’ cell histiocytosis (eosinophil granuloma). The vertebral body is flattened and sometimes referred to as a ‘vertebra plana’ (Fig. 13.5e).
- Neoplasm (metastases and myeloma)
- Osteoporosis
- Trauma
- Infection
- Eosinophilic granuloma
Fig. 13.5 Collapsed vertebra. (a) Metastasis (arrow) causing complete collapse of the vertebral body. The adjacent vertebral discs are unaffected. (Continued on following page) (b) Osteomyelitis. The disc space is narrowed and there is destruction of the surfaces of the adjacent vertebral bodies (arrows). (c) Traumatic collapse. Note the concave superior surface of the collapsed vertebral body. Some fragments have been extruded anteriorly (arrow). (d) Osteoporotic collapse. There is decreased bone density with a collapse of a vertebral body due to a compression fracture. (e) Collapse due to eosinophil granuloma. In this child the vertebral body is so collapsed that it resembles a thin disc (arrow).
Pedicle Abnormalities
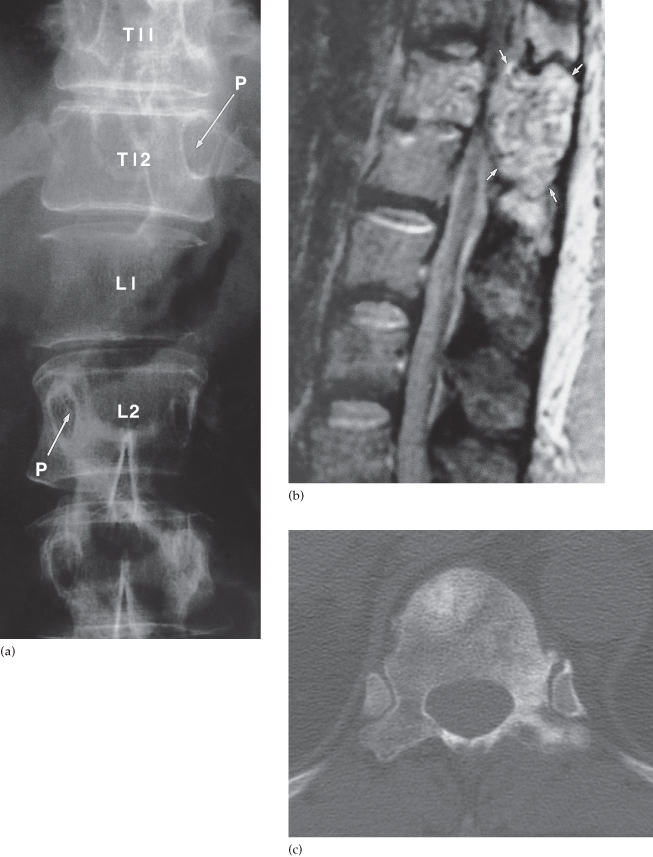
On plain films, the pedicles are best assessed in the frontal view and are very well demonstrated on CT scans. Destruction or sclerosis of one or more of the pedicles (Fig. 13.6, and see Fig. 13.29b) is a sign of spinal metastases.
Fig. 13.6 Destruction of the pedicles due to metastatic renal cell carcinoma. (a) The pedicles of L1 have both been destroyed, as has the right pedicle of T12. Arrows point to representative normal pedicles (P). (b) MRI scan in the same patient showing extensive tumour in the vertebral body and a posterior mass of tumour (arrows) which is compressing the dural sac. (c) CT scan in a different patient with prostatic metastases showing sclerosis of the left pedicle of a lower thoracic vertebra together with sclerosis in the vertebral body and transverse process.
Dense Vertebrae
Sclerosis, which is demonstrated on plain films or CT, may affect just one vertebra or may be part of a generalized process involving many bones. Common causes (Box 13.2) include the following:
- Metastases, particularly from primary tumours of the prostate or breast (Fig. 13.7).
- Malignant lymphoma.
- Paget’s disease. This may be difficult to distinguish from neoplastic disease, but a useful diagnostic feature is expansion of the overall size of the vertebra with coarsening of the trabecular pattern in Paget’s disease (Fig. 13.8).
- Haemangioma, a benign vascular abnormality that gives rise to characteristic vertical striations in a vertebra that is normal in size (Fig. 13.9).
Fig. 13.8 Paget’s disease. Note the increased density and coarse trabeculae in the vertebral bodies (arrows). They are also wider than the normal ones.
Spinal Abnormalities
Spinal Trauma
Cervical spine injuries are important to identify as significant neurological damage can occur if an unstable injury is unrecognized. Plain films are the commonest initial investigation for trauma to the spine and will usually comprise a lateral, anteroposterior and open mouth or peg view (Fig. 13.10). The following should be looked for:
- Alignment of the vertebral bodies and facet joints.
- Fractures of the vertebral bodies, pedicles, laminae and spinous processes.
- Indirect signs of fracture such as prevertebral soft tissue swelling.
Fig. 13.10 Normal cervical spine radiographs. (a) Anteroposterior, (b) lateral and (c) open mouth (peg) views. Note the lateral view includes the C7/T1 junction.
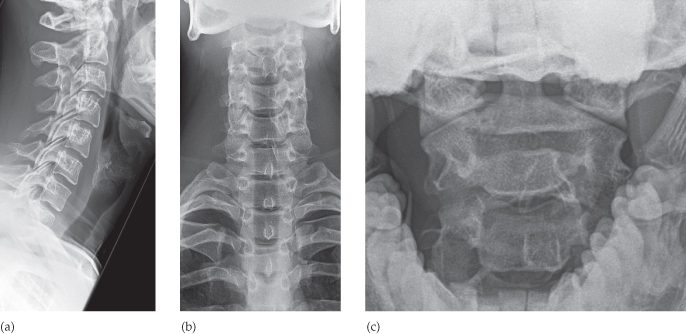
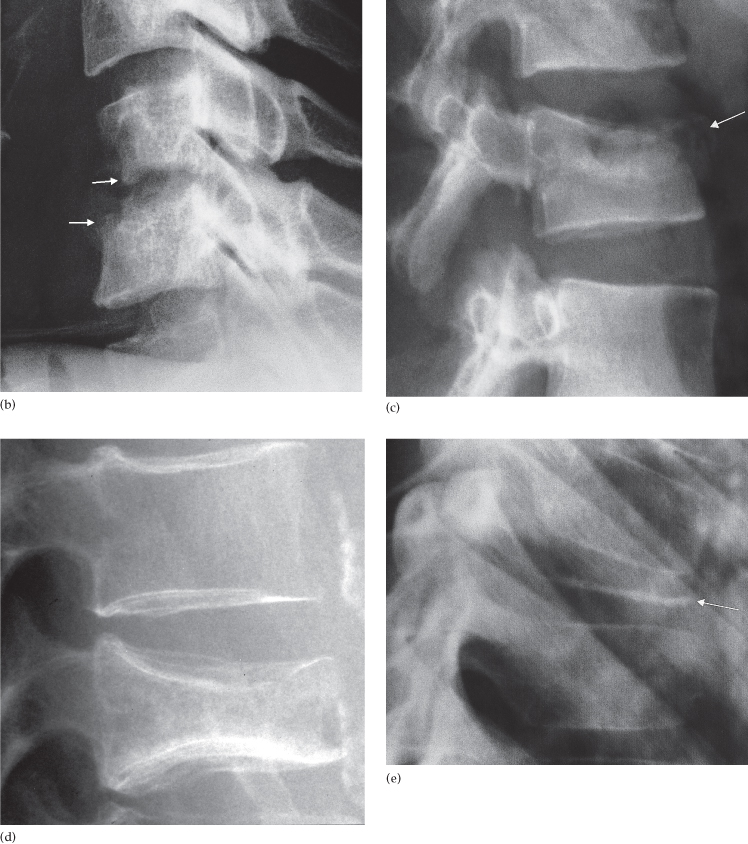
It is important that the entire cervical spine from the craniocervical to the cervicothoracic junction has been imaged otherwise a low unstable injury may be missed. Adequate imaging of the C7/T1 junction on the lateral film may be facilitated by gentle traction on the arms to depress the shoulders or by obtaining a view through the axilla (swimmer’s view). However, it may remain difficult to obtain satisfactory films, particularly in severely ill patients, and then a CT is indicated so the entire spine segment can be imaged. CT is also indicated as the primary imaging for patients with high risk of spinal injury, unexplained soft tissue swelling or if a fracture is seen on the radiographs. MRI is indicated in any patient where a potential spinal cord injury is suspected clinically or there are progressive neurological defects such as due to a contusion of the cord (Fig. 13.11). Children may suffer a significant ligamentous injury without evidence of any fractures on radiographs or CT, called SCIWORA (spinal cord injury without radiological abnormality), and are best imaged with MRI.
Fig. 13.11 Spinal cord injury. T2-weighted MRI showing high signal in the spinal cord due to oedema and haemorrhage (arrow).

After ensuring the entire cervical spine has been adequately imaged it is important to first assess the alignment of the vertebral bodies by drawing lines on the lateral film along the anterior and posterior surface of the vertebral bodies (which equates to the anterior and posterior longitudinal ligaments, respectively). A line drawn at the junction of the lamina and spinous process indicates the posterior border of the spinal canal (Fig. 13.12) and represents the ligamentum flavum. Any interruption of these lines or significant angulation between endplates indicates there may be serious injury (Fig. 13.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree