George M. Bridgeforth and Mark Nolden
A 40-year-old obese woman presents with hematuria and left flank pain. she denies any numbness, weakness, or bowel or bladder incontinence.
CLINICAL POINTS
- Spondylolysis
- Most cases are asymptomatic.
- This stable injury is characterized by a fracture of the pars interarticularis.
- The condition may be unilateral or bilateral.
- Most cases are asymptomatic.
- Spondylolisthesis
- Patients are usually asymptomatic.
- Symptomatic patients may complain of “something moving in my lower back.”
- Most injuries are stable and are characterized by a bilateral defect in the pars interarticularis.
- Patients are usually asymptomatic.
Clinical Presentation
Most cases of spondylolysis and spondylolisthesis are asymptomatic. They are an incidental finding on detected lumbar sacral radiographs of patients with acute trauma or persistent low back pain. Degenerative spondylolysis or spondylolisthesis usually occurs in patients who are older than 50 years. However, nondegenerative forms may occur in adolescents from contact sports (football) or in gymnasts.
Spondylosis is characterized by a defect in the pars interarticularis (which joins the laminae, the pedicles, and the facets in the posterior vertebral spine) without displacement. Most cases without acute trauma are asymptomatic.
Spondylolisthesis is characterized by anterior displacement of the vertebrae secondary to a defect in the pars interarticularis. Most cases are asymptomatic, but patients with unstable injuries from preexisting trauma or degeneration can develop unstable deficits leading to significant spinal cord damage. Most cases affect the L4–L5 level. Moreover, degenerative spondylolisthesis can be associated with spinal stenosis, neurogenic claudication, radicular pain, or facet arthropathy.
Spinal stenosis may occur as a solo entity without a concomitant spondylolisthesis. Patients with associated neurogenic claudication and spinal stenosis complain of pain, numbness, and weakness affecting both legs. Those with neurogenic claudication are usually older than 50 years. Unlike patients with disc disease, who usually present with unilateral numbness and weakness (affecting one lower extremity), older patients with spinal stenosis present with complaints of bilateral numbness and weakness (affecting both lower extremities). In addition, patients with radicular disc problems have pronounced pain with flexion, which results in increased pressure on the damaged discs. However, patients with spinal stenosis have decreased pain with flexion, which opens the foraminal spaces. Furthermore, unlike patients with disc injuries, patients with spinal stenosis complain of pain with extension. This may be due to narrowing of the foramen or associated facet arthropathies. Another key clinical clue is that radicular pain from disc injuries is generally aggravated by straight leg raising. With spinal stenosis, the findings are variable and depend on whether there is underling disc pathology. A negative straight leg raising test in an older patient with bilateral radicular symptoms points toward spinal stenosis.
PATIENT ASSESSMENT 
- Low back pain, aching, and stiffness
- Nontraumatic spondylolysis: usually asymptomatic radiographic finding
- Spondylolisthesis: usually does not cause radicular symptoms (numbness and weakness) unless unstable
An abdominal examination should be performed initially on all patients with low back pain (e.g., aneurysm, cholecystitis, pancreatitis) Also, the presence of good pulses would point away from vascular claudicating, which is usually seen in heavy smokers. Finally, it is important to note that spinal stenosis may also occur in the cervical spine.
Radiographic Evaluation
Anteroposterior, lateral, and oblique (two views) radiographs should be ordered. For severe spinal trauma, a computed tomography scan is necessary. With chronic spondylolisthesis, flexion and extension views should also be obtained.
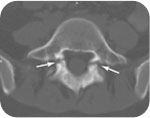
A spondylolysis is characterized by a separation of the pars interarticularis without displacement. The pars interarticularis is the bony isthmus that connects the superior and inferior facets of each individual vertebra. However, if there is displacement of the vertebral body (best identified on the lateral radiographs), the condition is called a spondylolisthesis (Fig. 2.1).

FIGURE 2.1 Lateral radiograph focused over the L5-S1 disc level in the patient described in the case presentation demonstrates the pars interarticularis defect with minimal anterior displacement of L5 over S1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








