Communication with joint
Wall composition
Cell lining
Contents
(Arthro)synovial cyst
Present
Continuous mesothelial lining
“True” synovial cells
Mucinous fluid
Ganglion (cyst)
May be present
Discontinuous mesothelial lining
Flattened pseudosynovial cells
Mucinous fluid
Bursitis de novo
Absent
Fibrous wall
No mesothelial lining
Fibrinoid necrosis
Bursa (permanent)
Absent
Continuous mesothelial lining
“True” synovial cells
Mucoid fluid
- 1.
The anatomical location and relationship with the adjacent joint, e.g., a communicating stalk with the joint. This communication can be visualized by imaging [109] or can be surgically proven.
- 2.
The histological composition of the cyst wall and the contents.
(Arthro)synovial Cyst
The term synovial cyst describes a continuation or herniation of the synovial membrane through the joint capsule. In the French literature, the term “arthrosynovial” cyst is preferred, which refers to their intimate relationship with the adjacent joint. Indeed, there is always a communication with the adjacent joint, and the histological composition is identical to that of the joint cavity; the wall consists of fibrous tissue lined with synovium continuous with the synovial membrane of the joint. It represents a collection of synovial fluid, lined by a continuous layer of “true” synovial cells, and is considered to be true cyst. The histological composition of a synovial cyst may change in time and as accumulated fluid becomes more viscous. This may result in increased pressure within the cyst and communication with the joint may become interrupted. Due to increased intracystic pressure, the layer of lining cells disappears and the cyst is transformed into a ganglion cyst (see infra) [81]. The presence of synovial cysts is always associated with increased joint effusion, which leads to increased intra-articular pressure, regardless of the underlying joint abnormality [66] that causes herniation of joint fluid and synovium through a “locus minoris resistentiae” of the joint capsule.
Baker’s cyst or popliteal cyst is the most characteristic example of a synovial cyst. It is a fluid-filled mass which represents a distention of a preexisting bursa in popliteal fossa, the medial gastrocnemius–semimembranosus bursa, which results from an extrusion of synovial fluid through a breach between the medial gastrocnemius muscle and semimembranosus tendon [30, 36] (Fig. 20.1). There is a joint connection as “ball-valve”-like mechanism, which is opened during knee flexion and closed during extension [2, 59, 79]. Other examples can be seen near other joints (spine, shoulder [98], elbow, hip [54, 85], hand [60], foot, and ankle [80]), but are less frequent. They are usually associated with joint diseases [8], such as labral tears [54, 85, 98], osteoarthrosis, and inflammatory and posttraumatic joint diseases [11, 25, 26, 34, 36, 63, 100, 108].


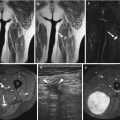
Fig. 20.1
(a–h) Synovial cyst – Baker’s cyst in different patients: (a) axial fat-suppressed turbo spin echo T2-weighted MR image; (b) sagittal fat-suppressed proton density MR image. (c) lateral radiography of the right knee; (d) computed tomography; (f) axial fat-suppressed proton density MR image; (e) sagittal fat-suppressed proton density MR image. (g) axial ultrasound of the popliteal fossa; (h) longitudinal ultrasound of the popliteal fossa in another patient. Soft tissue mass in the popliteal fossa with typical extension toward the joint which is well appreciated on the axial and sagittal MR images. Due to its fluid content, the lesion is of high signal intensity on T2-WI (a, b). Another patient with soft tissue mass in the popliteal fossa, with internal secondary osteochondromatosis, due to long-standing degenerative joint disease presented with calcifications at radiography (c) which is well depicted on computed tomography (d). Baker’s cyst on CT is shown as hypodense lesion with sharp delineated hyperdense borders (d). On axial and sagittal MR images, intralesional calcifications are of low signal intensity (e, f). In a third case, ultrasound shows an uncomplicated Baker’s cyst as an anechoic, well-demarcated lesion. The lesion has a deep and a superficial component and typically extends between the medial gastrocnemius muscle and semimembranosus tendon (g). In case of cyst rupture, ultrasound reveals volume decrease of the cyst compared to previous images and presence of fluid around the cyst extending to the calf (h). A Baker’s cyst represents a distended gastrocnemius–semimembranosus bursa and is lined by a normal synovial membrane. It may be the result of increased intra-articular pressure in cases of joint effusion. In the knee joint, these effusions are often associated with meniscal tears, rheumatoid disease, osteochondral lesions, or degenerative disease
Ganglion (Cyst)
Ganglia are benign cystic lesions that arise from the joint capsule or tendon sheath, most commonly from the limb joints, with rare occurrence at the spine. They contain mucinous fluid, which is highly viscous, proteinaceous material, rich in hyaluronic acid, glycosamine, albumin, and globulin [68], but their wall consists of a (discontinuous) layer of flattened pseudosynovial cells, surrounded by dense fibrous connective tissue (pseudocapsule) [41, 56, 61, 72, 102–104]. They are not true cysts because they lack a cellular lining and are made of a gelatinous, viscous material [13]. A communication with the adjacent joint is not always present (40–100 % of the cases) [88, 89, 112].
The pathogenesis of ganglion cysts is controversial. Several theories have been proposed, including displacement of the synovial tissue during embryogenesis, proliferation of pluripotential mesenchymal cells, mucoid degeneration of collagen, degeneration of connective tissues after trauma and repetitive microtraumas (degenerative theory), and migration of synovial fluid into the cyst (synovial herniation theory) [15, 29, 57, 101]. Pathogenesis is usually multifactorial.
Based upon the similar appearance on imaging and surgery and on the similar wall composition of synovial cysts and ganglion cysts, we believe that the synovial herniation hypothesis is the most satisfactory. According to this theory, both synovial cysts and ganglion cysts are formed by a herniation of synovium through a breach in the adjacent articulation. Ganglion cyst could represent an advanced stage of a synovial cyst which underwent histological changes due to increased intracystic pressure [81] which proved that both types of para-articular cysts are variants of the same disease spectrum. At one end of the spectrum, we have the pure (arthro)synovial cysts, which represent an extension of the joint cavity outside the joint, caused by herniation through a “locus minoris resistentiae” within the joint capsule. This explains why the histological composition of those cysts is exactly a copy of that of the adjacent joint and why the cellular lining consists of a continuous layer of “true” synovial cells. As those cysts grow and may extend further away from the joint into the soft tissues, they may undergo degenerative changes. First, the cellular lining may become discontinuous and individual cells may flatten, as they may be subject to fluctuations in intracystic pressure. This results in para-articular cysts, in which the wall composition consists of a discontinuous layer of pseudosynovial cells. Ultimately, the original communication with the joint may be obliterated. Therefore, at the other end of the disease spectrum, a ganglion cyst may represent an advanced degenerative stage of a synovial cyst, in which the continuous synovial lining and the communication with the joint may be lost during the process of degeneration (Fig. 20.2). Meniscal and ganglion cysts are commonly associated with degeneration of underlying anatomic structures [101].


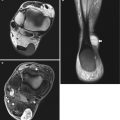
Fig. 20.2
(a–c) Pathogenesis according to the “synovial herniation hypothesis” of (a) (arthro)synovial cyst: this lesion originates from a herniation of the synovial membrane through the joint capsule. The histological composition is identical to the joint cavity, and the cellular lining consists of true synovial cells; (b, c) ganglion cyst: during the process of degeneration, and increased intracystic pressure, the cellular lining may change, partially disappear, and become discontinuous. Ultimately, the original communication with the joint may be obliterated
The following arguments support the “synovial” theory in their pathogenesis:
- 1.
The similar histological composition of synovial and ganglion cysts: both the contents (mucinous fluid) and the cellular lining are very similar (continuous layer of true synovial cells in arthrosynovial cysts versus a discontinuous lining of flattened pseudosynovial cells in ganglion cysts).
- 2.
The morphology of some ganglion cysts, e.g., their course along capsular arteries or capsular nerve branches, may explain a peculiar form. This is especially true for adventitial cystic disease and perineural cysts, which can be considered as variants of ganglion cysts [60, 79, 81] (Fig. 20.3).

Fig. 20.3
(a, b) Adventitial cystic disease of the popliteal artery. (a) Longitudinal and (b) axial Doppler ultrasound. Note anechoic lesion within the wall of the popliteal artery (asterisks on (a) and calipers on (b)). The lumen of the artery is patent and shows colored Doppler signal. Note also the presence of a small arterial branch communicating with the main artery on the longitudinal image (a). Adventitial cyst may result from dissection of fluid around articular branches of arteries, veins, or nerves. On ultrasound, it presents as an anechoic cystic lesion near by the colored arterial flow (a, b)
- 3.
The fluctuating volume of some cysts, sometimes complicated by rupture (Figs. 20.4 and 20.5), argues for a communication with the adjacent joint, which acts as a reservoir of synovial fluid [56, 69, 84, 103].



Fig. 20.4
(a–c) Ultrasound of a ruptured Baker’s cyst in a 68-year-old female with rheumatoid arthritis: (a) axial image shows a typical Baker’s cyst extending between the medial gastrocnemius muscle and semimembranosus tendon. The wall is thickened due to inflammation. Note also some intralesional septations and subtle vascularity due to inflammation; (b) longitudinal image shows pointing of the inferior border of Baker’s cyst in keeping with cyst rupture. (c) Longitudinal image of the calf shows diffuse edema within the subcutis

Fig. 20.5
(a–e) Ruptured ganglion cyst in the lower leg of a 54-year-old man: (a) ultrasound; (b) CT without contrast injection; (c) axial spin echo T1-weighted MR image; (d) axial turbo spin echo T2-weighted MR image; (e) axial spin echo T1-weighted MR image after gadolinium contrast injection. Ultrasound clearly shows a multiloculated cystic lesion in the lower leg (a). The image corresponds perfectly with the findings on nonenhanced CT (b). The lesion is clearly delineated with sharp borders. The adjacent fibular bone is not eroded. The MRI examination (c–e) was performed 2 weeks later. The cyst is ruptured, and there is fluid in the inter- and intramuscular fat planes (d). There is no evidence of hemorrhage (c). After gadolinium injection (e) enhancement is seen in the periphery of the lesion as a result of local inflammatory changes. This may lead to confusion in the differential diagnosis against other inflammatory soft tissue changes
Kumarasamy et al. reported a theory for explaining of the ganglion within the tendons; either mucinous degeneration of fibrous tissue or herniation of hypersecreting synovium of adjacent joints through a one-way valve type of mechanism may cause intratendinous cysts [2].
Ganglion cysts may be located anywhere around the joints. A para-articular location in fat layers (Figs. 20.6, 20.7, 20.8) or muscle (Fig. 20.9) is most frequently seen. Dissection of fluid around arteries or veins or nerves results in adventitial cystic disease [105] or peri- or intraneural cysts [52, 73, 106] where anatomic explanation is vicinity to neurovascular bundle. Adventitial cyst disease is found within a vessel wall (arteries or veins), and vascular branch would be the conduit from the joint, leading to dissection to the main parent vessel with accumulation of a mucinous substance within the adventitia (Fig. 20.3) [65, 74, 90]. Articular (synovial) theory explains intraneural ganglion cysts with joint fluid dissection within an articular branch and extending to the parent nerve [90, 94, 112], where joint connection was found in 40 % [88, 89] to 100 % of the cases, which was an explanation for the cyst recurrences [112]. High is the percentage (53 %) of the extraneural rupture of intraneural cysts [84]. The most common location of an intraneural ganglion cyst is in the peroneal nerve at the level of the fibular head [88–90], followed by the tibial nerve at the superior tibiofibular joint and ankle, the ulnar nerve at the elbow, the median nerve at the wrist, and the suprascapular nerve at the glenohumeral joint [93]. The presence of a combination of intraneural ganglia and vascular adventitial cysts in the same patient suggests that their content can dissect from a joint along neurovascular bundles [93].





Fig. 20.6
(a, b) Ganglion cysts in the subcutaneous fat of the dorsum of the foot: (a) sagittal fat-suppressed T2-weighted MR image; (b) short-axis T2-weighted MR image. Within subcutaneous tissue of the dorsum of the foot, there are multiple ganglion cysts which present ovoid, well-demarcated high signal intensity lesions (a, b). There is no obvious communication with the adjacent joints

Fig. 20.7
(a, b) Ganglion cyst on the wrist in tennis player: (a) longitudinal ultrasound; (b) longitudinal Doppler ultrasound. On ultrasound, note a polylobulated anechoic, relatively well-demarcated lesion (a). On Doppler ultrasound, there is distension of the ganglion cyst with displacement of an adjacent blood vessel (b)

Fig. 20.8
(a, b) Ganglion cysts of the proximal tibiofibular joint. (a) Coronal fat-suppressed proton density MR image; (b) sagittal fat-suppressed proton density MR image. Anterior to the proximal tibiofibular joint, there is polylobulated cystic lesion containing intralesional septa. The lesion is clearly demarcated from the surrounding tissue (a, b)

Fig. 20.9
Intramuscular ganglion cyst. CT scan of the left lower leg shows a sharply demarcated low-density lesion within the medial gastrocnemius muscle
A meniscal cyst (parameniscal ganglion cysts) is formed adjacent or within the menisci (Fig. 20.10) and is considered as a particular form of a ganglion cyst, in which synovial fluid is extruded through a horizontal meniscal tear (Fig. 20.10a), due to translocation of synovial cells or extravasation of synovial fluid into the meniscus [95], and accumulates at the menisco-capsular margin, resulting in an encapsulated mass around the meniscus [11, 31, 38]. Meniscal cysts are lined by flat spindle-shaped cells, have no synovial lining, and are characterized by myxoid contents [40], and the wall is formed of dense fibrous connective tissue (not synovium) as a distinguishing feature [36].


Fig. 20.10
(a–d) Meniscal cyst in different patients: (a) coronal T2-weighted fat-suppressed MR image; (b) axial T2-weighted fat-suppressed MR image; (c) longitudinal ultrasound; (d) coronal fat-suppressed proton density MR image. On coronal and axial MR image, multicystic lesion extruded from the peripheral border of the lateral meniscus, which is associated with horizontal meniscal tear (arrow) (a, b). In a second patient, meniscal cyst is well depicted on ultrasound as anechoic lesion adjacent to the posterior horn of medial meniscus (c). The transverse meniscal tear is seen on the MR image. (arrow) (d)
Other examples of intra-articular locations are paralabral (Figs. 20.11 and 20.12) (shoulder and hip) and cruciate ligament cysts (Fig. 20.13) [31, 115]. The full-thickness tears at the transitional zone of the labrum of the hip, which is with relative hypovascularity (“watershed zone”), as a weak point, may be a key factor in the development of paralabral cysts [55, 62]. On MR arthrography in 94 % of the cases, paralabral cysts of the hip are filled with intra-articular contrast material [55]. Arthrosynovial cyst of the hip joint can be developed after total hip arthroplasty as a sign of a deteriorating prosthesis surface [51]. A similar case was reported after primary total knee arthroplasty where popliteal cyst contains polyethylene debris, confirming joint communication [67].




Fig. 20.11
(a–c) Ganglion cyst in the spinoglenoid notch of the shoulder (paralabral cyst): (a) ultrasound axial section; (b) axial T2-weighted MR image; (c) coronal fat-suppressed T2-weighted MR image. On ultrasound, there is a well-demarcated anechoic lesion (a) which is of high signal intensity on T2-weighted MR image and is located at the spinoglenoid notch of the scapula (b, c)

Fig. 20.12
(a–c) Paralabral cyst of the left hip. (a) Standard radiograph; (b) axial fat-suppressed T2-weighted MR image; (c) coronal fat-suppressed TSE T2-weighted MR image. Plain radiography (a) reveals the presence of a sclerotic defined erosion at the superolateral aspect of the left acetabulum (arrows). On axial and coronal FS TSE T2-weighted MR images, there is a multicystic structure within the acetabular labrum, extending at the lateral aspect of the left acetabulum, causing pressure erosion (b, c). Note also the presence of internal bone debris on the standard radiographs (a), which appears as hypointense dot-like structures within the labral cyst on the FS TSE T2-weighted MR images. There is bone marrow edema at the lateral aspect of the left femoral head, as well as in the acetabulum, due to preexisting osteoarthrosis of the hip

Fig. 20.13
(a–c) Ganglion small cysts of anterior cruciate ligament. (a) Sagittal fat-suppressed proton density MR image; (b) coronal fat-suppressed proton density MR image; (c) axial fat-suppressed proton density MR image. The fibers of the anterior cruciate ligament are interspersed by elongated elliptic small areas of high signal intensity which are clearly delineated on sagittal image (a). On coronal and axial image may be difficult to distinguish anterior cruciate ligament cysts from partial tears of the ACL (b, c)
A possible cause of intra-articular ganglion cyst is repetitive minor trauma [6, 53, 68] and most commonly is associated with the anterior cruciate ligament (Fig. 20.13), but can also occur at the posterior cruciate ligament, posterior joint capsule, and infrapatellar fat pad, from chondral fractures or with subchondral bone cysts [3, 6, 19, 31, 42, 47, 53, 68, 86, 111].
Recent reports indicate that all juxtafacet cysts (either synovial, ganglion, and flavum ligament cysts) arise from degenerated facet joints [27, 48, 71, 92] with increased segmental motion as a trigger for herniation of the facet joint synovium [4, 16].
Rare localizations include temporomandibular joint [35], ganglia arising from the transverse acetabular ligament [10], and a ganglion cyst arising from the anterior horn of the medial meniscus impinged between the medial meniscus and the anterior cruciate ligament [31].
Extracapsular ganglia may arise from the medial or from the lateral head of the gastrocnemius muscle with “bunch of grapes” appearance [23, 39] or intramuscular ganglia within the peroneus longus muscle [58] or within the tendon of semimembranosus muscle, few centimeters above the insertion of the muscle without communication with the knee joint or any adjacent bursae [2, 44]. The bicipital intertubercular groove very rarely serves as the origin of an intra-articular ganglion cyst of the long head of the biceps tendon, which on MRI can be presented as cyst of the biceps tendon in the intertubercular groove with extension to the shoulder joint [83].
Other para-articular locations such as the subperiosteal area of the diaphyses of the long bones (periosteal ganglion) are rare [46, 57] (Fig. 20.14), while intraosseous ganglia are frequent.




Fig. 20.14
(a–f) Subperiosteal ganglion cyst of different patients: (a) radiography; (b) ultrasound, longitudinal section; (c) ultrasound, axial section; (d) axial T1-weighted MR image; (e) axial T1-weighted fat-suppressed gadolinium-enhanced MR image; (f) axial T2-weighted fat-suppressed MR image. At radiography a discrete elevation of the periosteum can be seen at the medial aspect of tibia (arrow) (a). On ultrasound, ganglion cyst is presented as well-demarcated anechoic lesion (measurements) adjacent to outer hyperechoic cortex of the tibia (b, c). On T1-weighted image, the lesion is with intermediate signal intensity with broad base at the outer aspect of the tibial cortex elevating the periosteum (arrow) and extruding to the subcutaneous tissue (near skin marker) (d). The lesion is with low signal intensity on fat-suppressed T1-weighted image after gadolinium contrast enhancement (e) and with very high signal intensity on fat-suppressed T2-weighted image, presented in another patient, where elevated periosteum can be seen (arrows) (f)
Bursa De Novo (Adventitious Bursa)
Inflammation of connective tissue in areas subject to chronic frictional irritation may result in fibrinoid necrosis, with formation of a bursa de novo or an adventitious bursa. This consists of a cystic structure filled with cellular debris, extracellular fluid, altered ground substance, and inflammatory exudate [107]. The first metatarsophalangeal joint is the most typical location, although other areas of chronic friction may provoke formation of an adventitious bursa (e.g., bursitis de novo at the medial side of medial malleolus in skaters due to chronic friction) (Fig. 20.15) [18].




Fig. 20.15
(a–e) Adventitious bursa due to chronic friction at the medial malleolus in a skater: (a) clinical picture; (b) radiography Figure part a and are lacking. Please add, will send it by e-mail. (c) ultrasound; (d) axial fat-suppressed proton density MR image; (e) coronal fat-suppressed proton density MR image. On clinical examination a soft tissue swelling at the medial aspect of the ankle can be seen (a) which is seen also at radiography (arrow) (b). On ultrasound, a well-demarcated heterogeneously hypoechoic structure is seen in the subcutaneous tissue near the medial malleolus with intralesional hyperechoic debris (c). MR reveals a clearly demarcated cystic lesion (arrow), with intralesional strands (d, e) (Image used with permission from De Keersmaeker et al. [18, 83])
Bursa
Bursae are enclosed flattened sacs, synovium-lined structures, which are normally interposed between ligaments or tendons and adjacent bony surfaces. Its main function is to reduce friction between adjacent moving structures. They have an anatomically predisposed topography, with or without connection to joint spaces. Containing a small amount of lubricating, mucinous fluid normally is quiescent and is normal not to be visualized on MR images [6, 14, 61]. Bursitis is an inflammation of a bursa, and/or filled with abnormal accumulation of fluid [7, 14], usually due to chronic mechanical friction, but may be also caused by an infectious or rheumatoid disease, overuse, trauma, and hemorrhage [37]. The presence of internal joint derangement, and collagen vascular diseases, may cause thickening of the synovial lining with increasing of fluid content within bursa [7] (Figs. 20.16, 20.17, and 20.18), and the presence of internal loose bodies, synovial debris, or bleeding may give heterogeneous appearance to bursa (Fig. 20.15c).