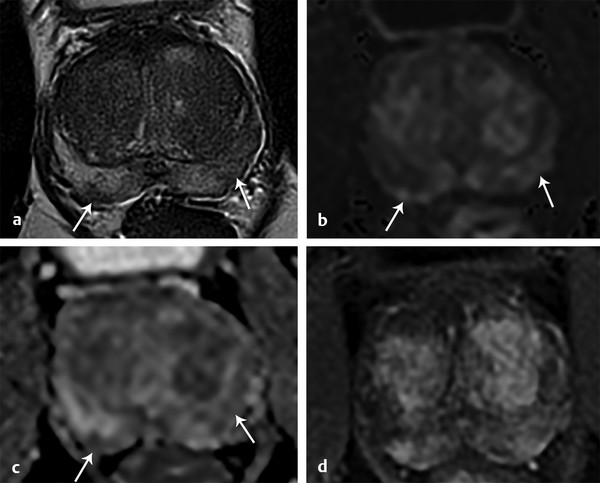
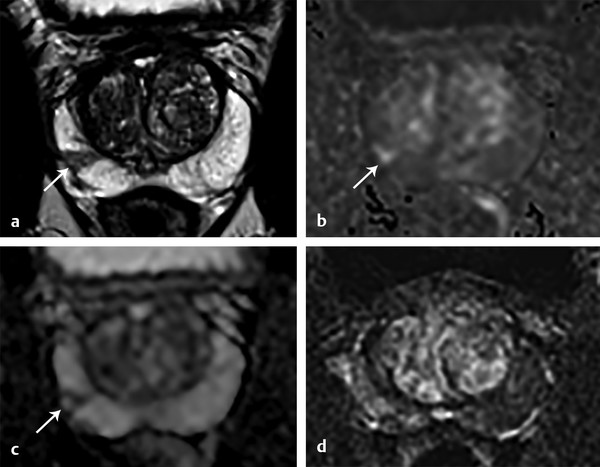
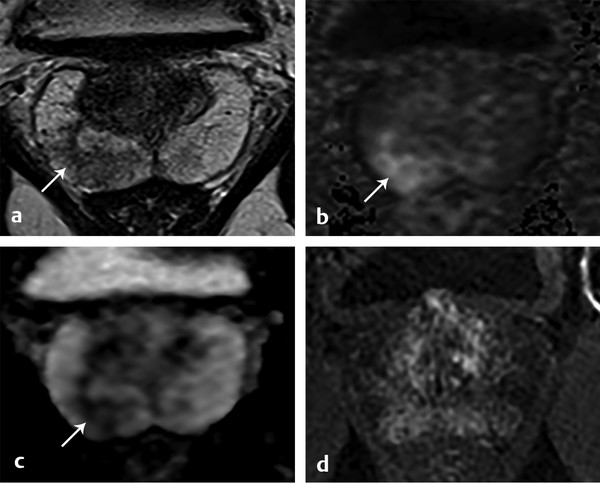
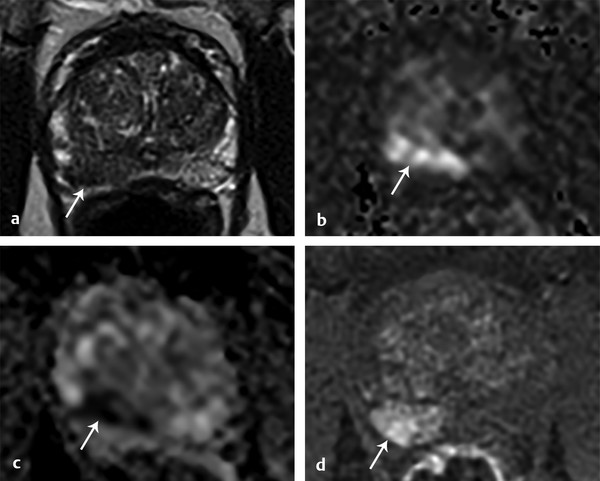
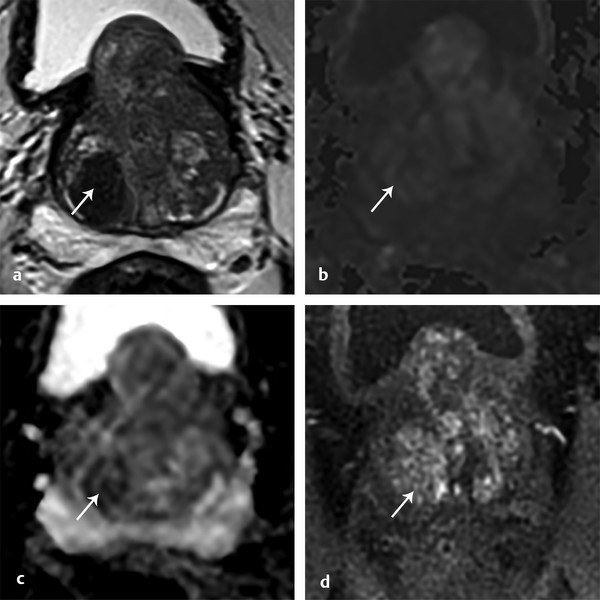
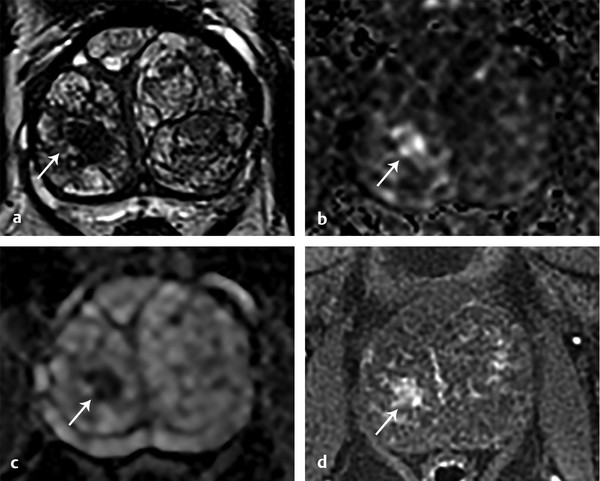
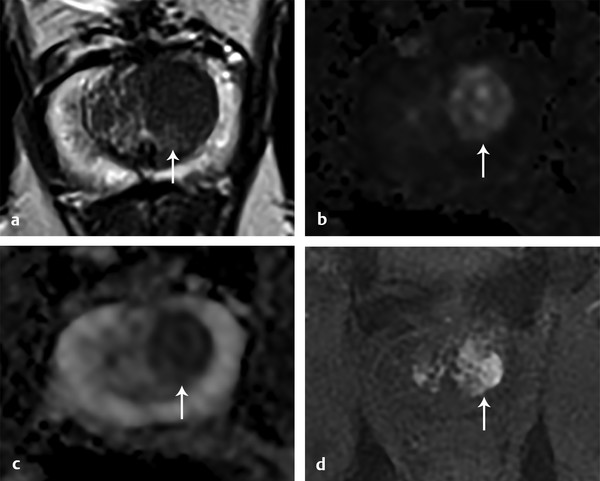
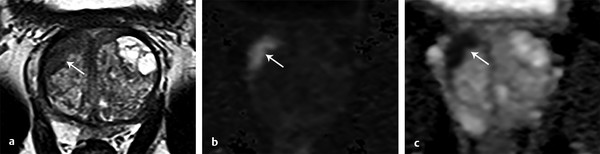
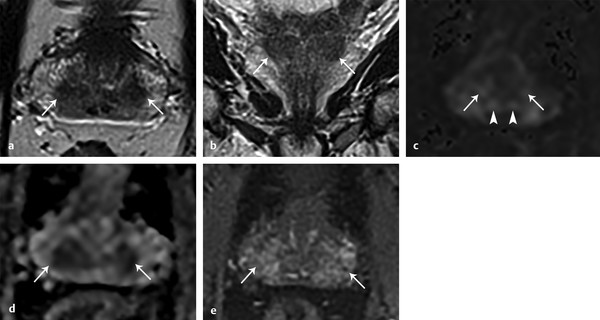
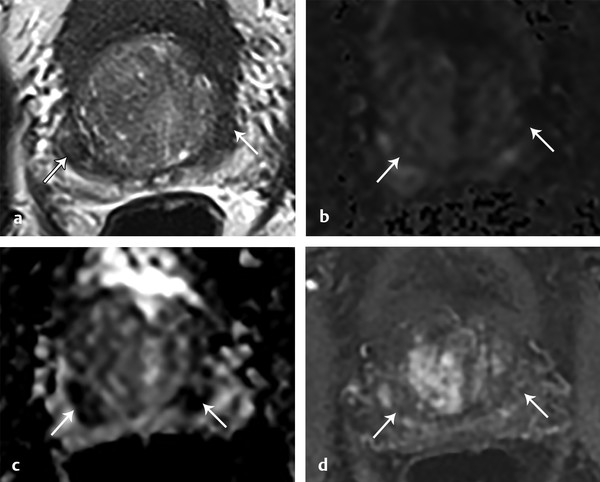
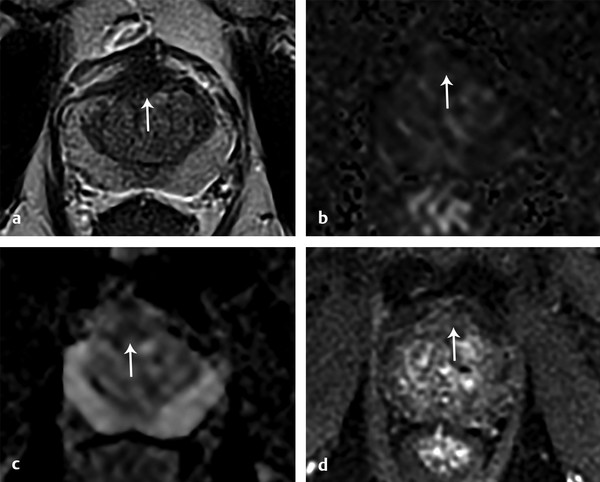
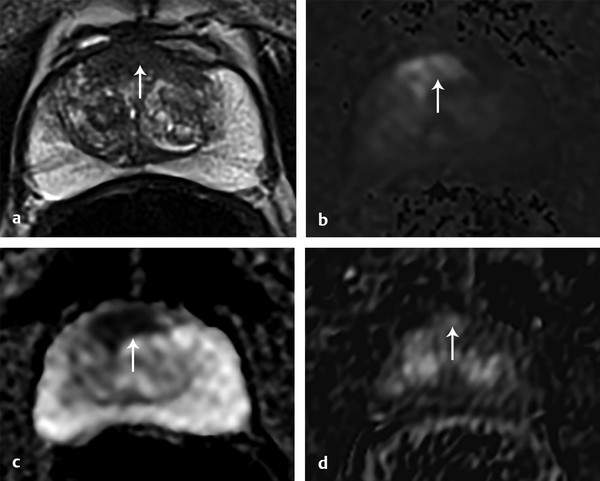
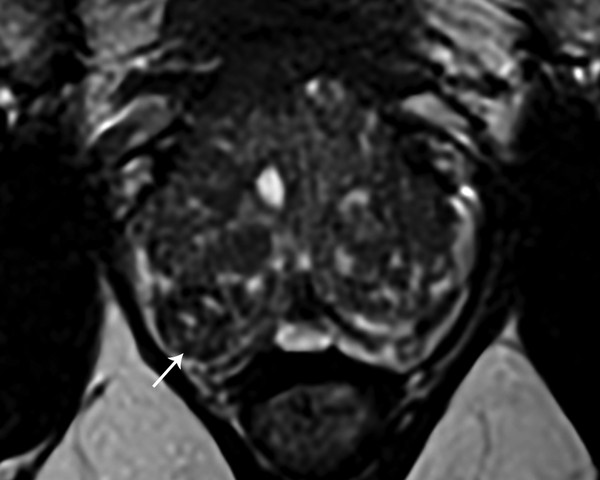
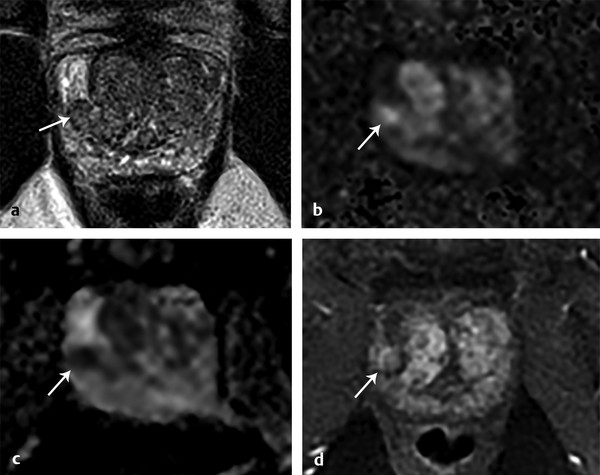
Case 1: PI-RADS 2 Lesion Corresponding to High-Grade Prostatic Intraepithelial Neoplasia A 58-year-old man with a rising PSA level (4.1 ng/mL) and no prior prostate biopsy ( ▶ Fig. 12.1). Fig. 12.1 PI-RADS v2 lesion corresponding to high-grade prostatic intraepithelial neoplasia. T2WI: Diffuse T2 hypointensity in the left base-to-midgland peripheral zone DWI (b = 1500 s/mm2): Indistinct mild hyperintensity ADC: Indistinct mild hypointensity DCE: Diffuse bilateral early enhancement (negative DCE) PI-RADS v2 assessment category: 2 High-grade prostatic intraepithelial neoplasia (HGPIN) in multiple bilateral cores. Teaching points: HGPIN is considered a premalignant lesion and is a potential cause of false-positive MRI interpretations. Management entails a combination of repeat PSA measurements and prostate biopsies, although there is variation across protocols in the timing and number of follow-up biopsies. [1] Ramaswamy K, Lepor H, Taneja SS. Management of High-Grade Prostatic Intraepithelial Neoplasia (HGPIN). Prostate Cancer Diagnosis: Springer; 2013:241–254. [2] Rosenkrantz AB, Mussi TC, Borofsky MS, Scionti SS, Grasso M, Taneja SS. 3.0 T multiparametric prostate MRI using pelvic phased-array coil: utility for tumor detection prior to biopsy. Urol Oncol 2013; 31(8): 1430‐1435 A 65-year-old man with an elevated PSA level of 7.5 ng/mL and prior negative prostate biopsy ( ▶ Fig. 12.2). Fig. 12.2 PI-RADS 3 lesion corresponding to prostatitis. T2WI: Linear and wedge-shaped T2 hypointensity in bilateral midgland peripheral zones DWI (b = 1500 s/mm2): Mild hyperintensity bilaterally ADC: Mild low signal bilaterally DCE: Diffuse bilateral enhancement (negative DCE) PI-RADS v2 assessment category: 3 for both lesions MRI-TRUS fusion biopsy revealed prostatitis. Teaching Points: Prostatitis is often asymptomatic and can show decreased T2 signal, restricted diffusion, and early enhancement, which are also MRI features seen in cancer. However, the morphology of prostatitis is linear, wedge-shaped, or diffuse, and the degree of T2 hypointensity and diffusion signal abnormality is often mild. [1] American College of Radiology (ACR) Prostate Imaging–Reporting and Data System (PI-RADS), Version 2. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/PIRADS/PIRADS%20V2.pdf. Published 2015. Accessed on October 30, 2015. A 62-year-old man with a PSA level of 5.2 ng/mL and no prior prostate biopsy ( ▶ Fig. 12.3). Fig. 12.3 PI-RADS 3 lesion corresponding to benign prostate tissue. T2WI: Wedge-shaped hypointensity in the right midgland peripheral zone DWI (b = 1500 s/mm2): Mild hyperintensity ADC: Mild low ADC DCE: No focal early enhancement matching the edges of the T2WI or DWI abnormality (negative DCE) PI-RADS v2 assessment category: 3 MRI-TRUS fusion biopsy revealed benign prostatic tissue. Teaching point: Wedge-shaped lesion morphology on T2WI warrants a T2WI score of 2 and can be seen with prostatitis, atrophy, or fibrosis. However, this case was considered to show focal low ADC and DWI hyperintensity, thus warranting both a DWI score of 3 and overall PI-RADS assessment category of 3. [1] American College of Radiology (ACR) Prostate Imaging–Reporting and Data System (PI-RADS), Version 2. 2015. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/PIRADS/PIRADS%20V2.pdf. Published 2015. Accessed on October 30, 2015. A 56-year-old man with an elevated PSA level of 7.5 ng/mL and no prior prostate biopsy ( ▶ Fig. 12.4). Fig. 12.4 PI-RADS 3 lesion corresponding to low-grade prostate cancer. T2WI: Noncircumscribed moderate hypointensity in the right posterior base peripheral zone DWI (b = 1500 s/mm2): Focal mild hyperintensity ADC: Focal moderate low ADC DCE: Diffuse bilateral early enhancement (negative DCE) PI-RADS v2 assessment category: 3 MRI-TRUS fusion biopsy revealed Gleason score 3+3 prostate cancer. Teaching points: The histologic diagnosis in this PI-RADS 3 lesion is consistent with published literature demonstrating the majority of PI-RADS 3 lesions to be benign or to harbor low-grade cancer. [1] Vargas HA, Hötker AM, Goldman DA et al. Updated prostate imaging reporting and data system (PIRADS v2) recommendations for the detection of clinically significant prostate cancer using multiparametric MRI: critical evaluation using whole-mount pathology as standard of reference. Eur Radiol 2016; 26(6): 1606‐1612 A 55- year-old man with a PSA level of 19 ng/mL and no prior prostate biopsy ( ▶ Fig. 12.5). Fig. 12.5 PI-RADS 4 lesion corresponding to intermediate-grade prostate cancer. T2WI: 1-cm circumscribed, homogeneous, moderately hypointense mass in the left posteromedial midgland peripheral zone DWI (b = 1500 s/mm2): Focal marked hyperintensity measuring < 1.5 cm ADC: Focal marked hypointensity DCE: Focal early enhancement matching the edges of the lesion on other sequences (positive DCE) PI-RADS v2 assessment category: 4 Gleason score 3+4 prostate cancer. Teaching points: A homogenous circumscribed mass in the peripheral zone with markedly abnormal DWI/ADC signal intensity likely represents clinically significant cancer. A 63-year-old man with an elevated PSA level of 29.3 ng/mL and no prior prostate biopsy ( ▶ Fig. 12.6). Fig. 12.6 PI-RADS 5 lesion corresponding to high-grade prostate cancer. T2WI: 1.7-cm circumscribed, homogeneous, markedly hypointense mass in the right posteromedial midgland peripheral zone DWI (b = 1500 s/mm2): Focal marked hyperintensity measuring ≥ 1.5 cm ADC: Focal marked hypointensity. ADC value was 450 µm2/s DCE: Focal early enhancement matching the edges of the lesion on other sequences (positive DCE) PI-RADS v2 assessment category: 5 Gleason score 4+5 prostate cancer. Teaching points: Assessment of lesion ADC is generally performed using qualitative visual inspection. While lower ADC values have been shown to be associated with higher-grade tumor, ADC values overlap between benign prostate tissue and low- and high-grade cancer. Additionally, quantitative ADC values vary based on scanner platform as well as acquisition and measurement technique. Allowing for these caveats, an ADC value below 750 to 900 μm2/s has been proposed as a threshold for clinically significant cancer. [1] American College of Radiology (ACR) Prostate Imaging–Reporting and Data System (PI-RADS), Version 2. 2015. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/PIRADS/PIRADS%20V2.pdf. Published 2015. Accessed on October 30, 2015. A 69-year-old man with an elevated PSA level of 6.9 ng/mL and no prior biopsy ( ▶ Fig. 12.7). Fig. 12.7 PI-RADS 2 lesion corresponding to atypical benign prostatic hyperplasia nodule. T2WI: 1.9-cm oval, well-circumscribed, homogeneously T2 hypointense nodule in the right posterior midgland transition zone DWI: Isointense to the remainder of the transition zone ADC: Mild focal hypointensity on ADC DCE: Focal early enhancement matching the edges of the T2WI and ADC abnormality (positive DCE) PI-RADS v2 assessment category: 2 MRI-TRUS fusion biopsy was benign. This is a minimally atypical, stromal benign prostatic hyperplasia (BPH) nodule. Teaching points: In the transition zone, the T2WI appearance is the predominant driver of the overall PI-RADS category. Since the T2WI appearance of this lesion warranted a score of 2, the overall PI-RADS category was 2, regardless of the DWI and DCE findings. This scheme reflects the fact that BPH nodules commonly show restricted diffusion and positive DCE. BPH nodules that are mostly comprised of glandular components are T2 hyperintense, while those that are mostly stromal appear T2 hypointense. BPH nodules typically show a mixture of signal intensities, giving a heterogeneous appearance. A round or oval shape, well-circumscribed border, and capsule are features suggesting a BPH nodule rather than transition zone tumor. [1] American College of Radiology (ACR) Prostate Imaging–Reporting and Data System (PI-RADS), Version 2. 2015. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/PIRADS/PIRADS%20V2.pdf. Published 2015. Accessed on October 30, 2015. A 77-year-old man with a PSA level of 2.4 ng/mL and high-grade prostatic intraepithelial hyperplasia (HGPIN) on prior prostate biopsy ( ▶ Fig. 12.8). Fig. 12.8 PI-RADS 3 lesion in the transition zone corresponding to low-grade prostate cancer. T2WI: 1.1 cm T2 hypointense lesion in the right anterior transition zone that is slightly heterogeneous with obscured margins. Notice the irregular shape and absence of a complete, smooth, well-defined capsule. DWI (b = 1500 s/mm2): Marked hyperintensity ADC: Moderate hypointensity DCE: Focal early enhancement matching the edges of the lesion on the other sequences (positive DCE) PI-RADS v2 assessment category: 3 Gleason score 3+3 prostate cancer Teaching points: Differentiation of atypical benign prostatic hyperplasia nodules and transition zone tumors is challenging. Signal abnormality on T2WI and DWI/ADC should be assessed relative to the remainder of the TZ in the same patient. Obscured margins raise suspicion for TZ tumor. A 67-year-old man with a PSA level of 3.1 ng/mL and negative prior prostate biopsy ( ▶ Fig. 12.9). Fig. 12.9 PI-RADS 4 lesion in the transition zone corresponding to intermediate-grade prostate cancer. T2WI: 1.3-cm noncircumscribed, moderate T2 hypointense lesion in the right anterior transition zone measuring 1.3 cm. DWI (b = 1500 s/mm2): Marked hyperintensity measuring < 1.5 cm ADC: Marked hypointensity measuring < 1.5 cm DCE: Focal early enhancement matching the edges of the lesion on the other sequences (positive DCE) PI-RADS v2 assessment category: 4 Gleason score 3+4 prostate cancer Teaching points: This transition zone lesion is visually most striking on DWI/ADC. Although DWI is not the primary determinant of the PIRADS v2 assessment category for transition zone lesions, it can be helpful for initial identification of lesions and for calling the reader’s attention to areas to scrutinize more closely on T2WI. A 65-year-old man with an elevated PSA level of 16 ng/mL and negative prior prostate biopsy ( ▶ Fig. 12.10). Fig. 12.10 PI-RADS 5 transition zone lesion corresponding to high-grade prostate cancer. T2WI: Homogenous, moderately hypointense lesion with noncircumscribed partially obscured margin measuring 1.7 cm DWI (b = 1500 s/mm2): Focal marked hyperintensity measuring > 1.5 cm ADC: Focal marked hypointensity measuring > 1.5 cm DCE: Focal early enhancement matching the edges of the lesion on the other sequences (positive DCE) PI-RADS v2 assessment category: 5 Gleason score 4 + 4 prostate cancer. Teaching points: The “erased charcoal” sign on T2WI can help identify transition zone tumors. This sign refers to a lesion that is T2 hypointense with blurred, indistinct margins. This appearance has also been described as resembling a smudged fingerprint. [1] American College of Radiology (ACR) Prostate Imaging–Reporting and Data System (PI-RADS), Version 2. 2015. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/PIRADS/PIRADS%20V2.pdf. Published 2015. Accessed on October 30, 2015. A 67-year-old man with an elevated PSA level of 5.1 ng/mL and negative prior prostate biopsy ( ▶ Fig. 12.11). Fig. 12.11 PI-RADS 5 lesion in the transition zone corresponding to low-grade prostate cancer. T2WI: 2.1-cm crescentic-shaped lesion in the right anterior midgland transition zone that is homogenous and moderately T2 hypointense DWI (b = 1500 s/mm2): Focal marked hyperintensity measuring ≥ 1.5 cm ADC: Focal marked hypointensity measuring ≥ 1.5 cm. The ADC value was 480 µm2/s PI-RADS v2 assessment category: 5 Gleason score 3 + 3 prostate cancer. Teaching points: Although this lesion is markedly hypointense on ADC, the tumor was found to be low grade. The association between ADC values and Gleason score assessment category in the transition zone is not as strong as their association in the peripheral zone. [1] Hambrock T, Somford DM, Huisman HJ et al. Relationship between apparent diffusion coefficients at 3.0-T MR imaging and Gleason grade in peripheral zone prostate cancer. Radiology 2011; 259(2): 453‐461 [2] Tamada T, Sone T, Jo Y et al. Apparent diffusion coefficient values in peripheral and transition zones of the prostate: comparison between normal and malignant prostatic tissues and correlation with histologic grade. J Magn Reson Imaging 2008; 28(3): 720‐726 [3] Verma S, Rajesh A, Morales H et al. Assessment of aggressiveness of prostate cancer: correlation of apparent diffusion coefficient with histologic grade after radical prostatectomy. AJR Am J Roentgenol 2011; 196(2): 374‐381 A 68-year-old man with an elevated PSA level of 5.5 ng/mL ( ▶ Fig. 12.12). Fig. 12.12 Normal central zone. Axial T2WI: Symmetric, dumbbell–shaped, T2 hypointensity at the base of the prostate surrounding the ejaculatory ducts Coronal T2WI: Symmetric T2 hypointensity at the base of the prostate DWI (b = 1500 s/mm2): Minimal hyperintensity (long arrow). Note the increased signal within the ejaculatory ducts (arrowheads). ADC: Moderately hypointense DCE: Mild, delayed enhancement Characteristic symmetric appearance of the central zone (benign). Teaching points: The central zone surrounds the ejaculatory ducts and is located predominantly at the base of the prostate and extends to the verumontanum. It can be distinctly visualized in the large majority of patients. The central zone typically appears as a symmetric band of T2 hypoinensity at the base of the prostate that shows decreased ADC. One study reported that the normal CZ shows progressive (type 1) or plateau (type 2) enhancement on DCE. Coronal images can help show the symmetric, triangular appearance of the central zone. [1] Hansford BG, Karademir I, Peng Y et al. Dynamic contrast-enhanced MR imaging features of the normal central zone of the prostate. Acad Radiol 2014; 21(5): 569‐577 [2] Vargas HA, Akin O, Franiel T et al. Normal central zone of the prostate and central zone involvement by prostate cancer: clinical and MR imaging implications. Radiology 2012; 262(3): 894‐902 [3] Yu J, Fulcher AS, Turner MA, Cockrell CH, Cote EP, Wallace TJ. Prostate cancer and its mimics at multiparametric prostate MRI. Br J Radiol 2014; 87(1037): 20130659 A 60-year-old man with a PSA level of 2.9 ng/mL and Gleason score 3+3 prostate cancer at the right apex on active surveillance ( ▶ Fig. 12.13). Fig. 12.13 Central zone displaced laterally. T2WI: Symmetric, bandlike, crescentic T2 hypointensity at the base of the prostate, positioned between the transition and peripheral zones bilaterally DWI (b = 1500 s/mm2): No hyperintensity ADC: Marked hypointensity DCE: No early enhancement Benign central zone displaced laterally Teaching points: The two lobes of the normal central zone can be displaced laterally. The symmetric appearance and lack of DWI hyperintensity helps establish the finding as the central zone. A 60-year-old man with an elevated PSA level of 6.1 ng/mL and no prior biopsy ( ▶ Fig. 12.14). Fig. 12.14 Central zone tumor. (Reproduced with permission from the American Journal of Roentgenology. Rosenkrantz AB et al. Prostate Cancer: Top Places Where Tumors Hide on Multiparametric MRI. Amer J Roentgenol 2015;204:W449-W456.) T2WI: Asymmetric prominence of the right central zone within the right posteromedial base DWI (b = 1500 s/mm2): Marked hyperintensity measuring ≥ 1.5 cm. ADC: Marked hypointensity measuring ≥ 1.5 cm DCE: Focal early enhancement with edges matching the T2 and DWI abnormality PI-RADS v2 assessment category: 5 MRI-TRUS fusion biopsy revealed Gleason score 3+4 prostate cancer. Concurrent standard 12-core biopsy was negative. Teaching points: Although less than 5% of tumors occur in the central zone, they tend to be more aggressive. Normal central zone is hypointense on T2WI and ADC and typically has a symmetric appearance. A central zone tumor can be suspected in the presence of central zone asymmetry with greater T2WI and ADC hypointensity compared to the contralateral side and early enhancement with washout (type 3 enhancement). [1] Vargas HA, Akin O, Franiel T et al. Normal central zone of the prostate and central zone involvement by prostate cancer: clinical and MR imaging implications. Radiology 2012; 262(3): 894‐902 A 74-year-old man undergoing work-up for hematuria found to have an abnormality of the prostatic urethra during cystoscopy. Biopsy revealed Gleason score 4+3 prostate cancer ( ▶ Fig. 12.15). Fig. 12.15 Benign thickening of the anterior fibromuscular stroma. T2WI: Noncircumscribed, convex T2 hypointense lesion involving the anterior fibromuscular stroma (AFMS) DWI (b = 1500 s/mm2): No abnormality ADC: Mild hypointensity DCE: No focal early enhancement matching the T2 or ADC abnormality Benign thickening of the AFMS. The patient underwent radical prostatectomy for tumor elsewhere in the gland, and no tumor was found in the AFMS or elsewhere in the anterior prostate. Teaching points: Although the appearance on T2WI is suspicious for tumor in this case, the lack of DWI hyperintensity or positive DCE indicate this is benign thickening of the anterior fibromuscular stroma. A 67-year-old with an elevated PSA level of 14.8 ng/mL and prior biopsy revealing high-grade prostatic intraepithelial neoplasia (HGPIN)( ▶ Fig. 12.16). Fig. 12.16 Tumor involving the anterior fibromuscular stroma. T2WI: Homogenous, crescentic T2 hypointense mass involving the midline anterior transition zone and anterior fibromuscular stroma DWI (b = 1500 s/mm2): Marked hyperintensity measuring ≥ 1.5 cm ADC: Marked hypointensity measuring ≥ 1.5 cm DCE: Mild early enhancement PI-RADS v2 assessment category: 5 MRI-TRUS fusion biopsy revealed Gleason score 3+4 prostate cancer Teaching points: The anterior fibromuscular stroma (AFMS) forms the anterior border of the prostate gland and is composed of T2 hypointense fibrous and smooth muscle tissue. Although the AFMS does not have glandular tissue, it has been recognized that tumors may grow predominantly within this region after arising from the margin of the transition zone. The tumors can expand the AFMS as they extend anteriorly and often have a lenticular shape. The presence of positive DCE can be helpful for tumor detection in this region, as the normal AFMS is hypovascular. [1] Rosenkrantz AB, Verma S, Turkbey B. Prostate cancer: top places where tumors hide on multiparametric MRI. AJR Am J Roentgenol 2015; 204(4): W449–W456 A 66-year-old man with an elevated PSA level of 8 ng/mL( ▶ Fig. 12.17). Fig. 12.17 Extruded benign prostatic hyperplasia (BPH) nodule in the peripheral zone. Axial T2WI: Round, heterogeneous, circumscribed, encapsulated lesion in the right posterolateral peripheral zone abutting the interface with the transition zone. The nodule contains areas of internal T2 hyperintensity and a thin, peripheral hypointense capsule. Extruded benign prostatic hyperplasia (BPH) nodule. Teaching points: Extruded BPH nodules may occur in the peripheral zone. A round, encapsulated nodule in the peripheral zone can be given an assessment category of 2 despite low ADC. Heterogeneous T2 signal resembling other typical BPH nodules in the transition zone, presence of a peripheral capsule, and location along the transition zone are reassuring features that support a diagnosis of an extruded BPH nodule. A 57-year-old man with an elevated PSA level of 5.9 ng/mL and negative prior prostate biopsy ( ▶ Fig. 12.18). Fig. 12.18 Extruded benign prostatic hyperplasia (BPH) nodule in the peripheral zone. Axial T2WI: Round, circumscribed T2 hypointense lesion in the right anterolateral midgland peripheral zone abutting the interface with the transition zone DWI (b = 1500 s/mm2): Marked hyperintensity measuring < 1.5 cm ADC: Marked hypointensity measuring < 1.5 cm DCE: Focal early enhancement matching the edges of the T2WI and DWI abnormality PI-RADS v2 assessment category: 2 MRI-TRUS fusion biopsy revealed benign prostate tissue. This represents an extruded benign prosatic hyperplasia (BPH) nodule. Teaching points: Extruded BPH nodules may be found in the peripheral zone. A round, encapsulated nodule in the peripheral zone can be assigned a PI-RADS assessment category of 2 despite low ADC. As with BPH nodules in the transition zone, these extruded nodules can show restricted diffusion and positive DCE. [1] American College of Radiology (ACR) Prostate Imaging–Reporting and Data System (PI-RADS), Version 2. 2015. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/PIRADS/PIRADS%20V2.pdf. Published 2015. Accessed on October 30, 2015. A 66-year-old man with an elevated PSA level of 6.4 ng/mL and two negative prior prostate biopsies ( ▶ Fig. 12.19). Fig. 12.19 Midline pseudolesion.
12.1.1 History
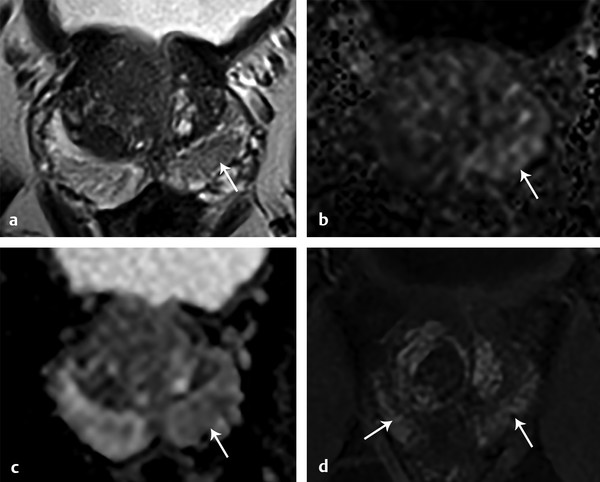
12.1.2 Prostate MRI Findings
12.1.3 Diagnosis
12.1.4 Suggested Reading
12.2 Case 2: PI-RADS 3 Lesion Corresponding to Prostatitis
12.2.1 History
12.2.2 Prostate MRI Findings
12.2.3 Diagnosis
12.2.4 Suggested Reading
12.3 Case 3: PI-RADS 3 Lesion Corresponding to Benign Prostate Tissue
12.3.1 History
12.3.2 Prostate MRI Findings
12.3.3 Diagnosis
12.3.4 Suggested Reading
12.4 Case 4: PI-RADS 3 Lesion Corresponding to Low-Grade Prostate Cancer
12.4.1 History
12.4.2 Prostate MRI Findings
12.4.3 Diagnosis
12.4.4 Suggested Reading
12.5 Case 5: PI-RADS 4 Lesion Corresponding to Intermediate-Grade Prostate Cancer
12.5.1 History

12.5.2 Prostate MRI Findings
12.5.3 Diagnosis
12.6 Case 6: PI-RADS 5 Lesion Corresponding to High-Grade Prostate Cancer
12.6.1 History
12.6.2 Prostate MRI Findings
12.6.3 Diagnosis
12.6.4 Suggested Reading
12.7 Case 7: PI-RADS 2 Lesion Corresponding to Atypical Benign Prostatic Hyperplasia Nodule
12.7.1 History
12.7.2 Prostate MRI Findings
12.7.3 Diagnosis
12.7.4 Suggested Reading
12.8 Case 8: PI-RADS 3 Lesion in the Transition Zone Corresponding to Low-Grade Prostate Cancer
12.8.1 History
12.8.2 Prostate MRI Findings
12.8.3 Diagnosis
12.9 Case 9: PI-RADS 4 Lesion in the Transition Zone Corresponding to Intermediate-Grade Prostate Cancer
12.9.1 History

12.9.2 Prostate MRI Findings
12.9.3 Diagnosis
12.10 Case 10: PI-RADS 5 Transition Zone Lesion Corresponding to High-Grade Prostate Cancer
12.10.1 History
12.10.2 Prostate MRI Findings
12.10.3 Diagnosis
12.10.4 Suggested Reading
12.11 Case 11: PI-RADS 5 Lesion in the Transition Zone Corresponding to Low-Grade Prostate Cancer
12.11.1 History:
12.11.2 Prostate MRI Findings
12.11.3 Diagnosis
12.11.4 Suggested Reading
12.12 Case 12: Normal Central Zone
12.12.1 History
12.12.2 Prostate MRI Findings
12.12.3 Diagnosis
12.12.4 Suggested Reading
12.13 Case 13: Central Zone Displaced Laterally
12.13.1 History
12.13.2 Prostate MRI Findings
12.13.3 Diagnosis
12.14 Case 14: Central Zone Tumor
12.14.1 History

12.14.2 Prostate MRI Findings
12.14.3 Diagnosis
12.14.4 Suggested Reading
12.15 Case 15: Benign Thickening of the Anterior Fibromuscular Stroma.
12.15.1 History
12.15.2 Prostate MRI Findings
12.15.3 Diagnosis
12.16 Case 16: Tumor Involving the Anterior Fibromuscular Stroma
12.16.1 History
12.16.2 Prostate MRI Findings
12.16.3 Diagnosis
12.16.4 Suggested Reading
12.17 Case 17: Extruded Benign Prostatic Hyperplasia Nodule in the Peripheral Zone
12.17.1 History
12.17.2 Prostate MRI Findings
12.17.3 Diagnosis
12.18 Case 18: Extruded Benign Prostatic Hyperplasia Nodule in the Peripheral Zone
12.18.1 History
12.18.2 Prostate MRI Finding
12.18.3 Diagnosis
12.18.4 Suggested Reading
12.19 Case 19: Midline Pseudolesion
12.19.1 History

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree