The Chest in Trauma, Postoperative, and Intensive Care
Jannette Collins
J. Collins: Department of Radiology, University of Wisconsin Medical School, Madison, Wisconsin 53792-3252.
ACUTE CHEST TRAUMA
Trauma is the leading cause of death in patients between the ages of 1 and 45 years, and it is the fifth most common cause of death in adults over the age of 65 years.73,114 In the United States alone, more than 300,000 patients are hospitalized annually because of chest injuries.108 Thoracic injury accounts for 25% of all traumatic deaths, and significant chest trauma is present in 50% of fatal traffic accidents.17 Most of the chest trauma seen in civilian populations is blunt chest trauma (90%), and most blunt chest trauma is the result of motor vehicle accidents and falls.68
After adequacy of the patient’s airway, breathing, and circulation (ABC) have been ensured and the patient has been evaluated and stabilized clinically, a chest radiograph is usually the first imaging study obtained in the evaluation of trauma patients. This study is often compromised by limited exposure capability, expiratory views, poor or absent patient cooperation, suboptimal patient positioning, and magnification and distortion of the mediastinum on the supine chest radiograph. The role of chest computed tomography (CT) in the management of trauma patients is evolving. Although studies have shown CT to be superior to supine chest radiography in revealing findings of chest trauma, these same studies reported minimal if any change in management based on observation of these additional findings on CT.76,122,143,156,183
Aortic Injury
Traumatic rupture of the aorta alone accounts for 16% of fatalities resulting from motor vehicle accidents, and 85% to 90% of patients with traumatic aortic rupture die before reaching a medical facility.187 In clinical series, 90% of aortic ruptures occur at the aortic isthmus, just distal to the origin of the left subclavian artery.27,31,104,118 Chest radiographic signs of aortic injury include (1) widening of the mediastinum, (2) blurring of the aortic knob or contour, (3) hemothorax, (4) rib fractures, (5) tracheal shift to the right, (6) left apical cap, (7) depression of the left main stem bronchus below 40°, (8) nasogastric tube displacement to the right, (9) pneumothorax, (10) pulmonary contusion, (11) widened left paraspinous line, and (12) abnormal mediastinal to chest width ratio, but they lack sensitivity and specificity. No single radiographic sign or combination of signs demonstrates sufficient sensitivity to indicate all cases of traumatic aortic rupture on plain-film chest radiographs without the performance of a large number of aortographically negative studies.131
The role of CT in the evaluation of aortic injury is controversial. Contrast-enhanced CT scans with 5-mm slices can help exclude mediastinal hemorrhage and reduce the angiography rate in low- to moderate-risk patients with a widened or indeterminate mediastinum on chest radiography.137 A review of studies, however, shows that a negative conventional CT scan does not exclude the possibility of an aortic laceration.90,120,127,132,162 CT aortography may prove to be an alternative to conventional CT and traditional angiography. In one study, technically adequate axial helical CT detected and defined all injuries of the thorax, and CT angiography supplemented the conventional examination and could have replaced transcatheter aortography except for small tears or indeterminate studies.54
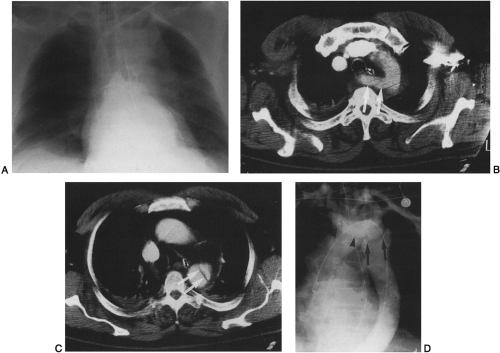
A CT aortography protocol consisting of spiral scanning beginning at the top of the diaphragm and extending up through the aorta with a collimation of 5 mm, a pitch of 2:1, and 3-mm reconstruction after administration of 150 mL of nonionic intravenous contrast material can be used to evaluate for aortic injury. If mediastinal hemorrhage is present without any direct signs of aortic injury, and no other
explanation for the hemorrhage is shown on CT, the patient is usually referred for conventional angiography. If direct signs of aortic injury are confirmed on CT, including aortic caliber change at the site of injury, focal outpouching of contrast material consistent with pseudoaneurysm, and intraluminal flap, the patient may or may not proceed to confirmatory conventional angiography, at the discretion of the surgeon (Fig. 31-1). Not only is CT useful for detecting direct signs of aortic injury, but CT can also show other causes of a wide mediastinum, including excessive mediastinal fat, adjacent lung contusion, artifact resulting from supine positioning, vascular tortuosity, and persistent left-sided superior vena cava.121 CT has been shown to be falsely negative in a patient with injury of the left subclavian artery16 and falsely positive in patients with atypical ductus diverticulum.138 Another contender for replacing conventional aortography is transesophageal echocardiography, which in experienced hands has a reported sensitivity of 100% and a specificity of 98% for diagnosis of acute aortic injury.68
explanation for the hemorrhage is shown on CT, the patient is usually referred for conventional angiography. If direct signs of aortic injury are confirmed on CT, including aortic caliber change at the site of injury, focal outpouching of contrast material consistent with pseudoaneurysm, and intraluminal flap, the patient may or may not proceed to confirmatory conventional angiography, at the discretion of the surgeon (Fig. 31-1). Not only is CT useful for detecting direct signs of aortic injury, but CT can also show other causes of a wide mediastinum, including excessive mediastinal fat, adjacent lung contusion, artifact resulting from supine positioning, vascular tortuosity, and persistent left-sided superior vena cava.121 CT has been shown to be falsely negative in a patient with injury of the left subclavian artery16 and falsely positive in patients with atypical ductus diverticulum.138 Another contender for replacing conventional aortography is transesophageal echocardiography, which in experienced hands has a reported sensitivity of 100% and a specificity of 98% for diagnosis of acute aortic injury.68
Lung Parenchymal Injury
Abnormal lung parenchymal opacification in trauma patients can result from atelectasis, aspiration, edema, pneumonia, contusion, or laceration and is commonly multifactorial in origin. Pulmonary contusion, resulting in leakage of blood and edema fluid into the interstitial and alveolar spaces, has been accepted as the primary lung injury in nonpenetrating chest trauma. Pulmonary laceration is a more severe injury, resulting in disruption of the lung architecture. Wagner and associates205 proposed that pulmonary laceration is the basic component in the mechanism of injury in pulmonary contusion, pulmonary hematoma, pulmonary cyst or pneumatocele, and cavitation in pulmonary contusion. They classified
lacerations into four types: (1) those involving an air-filled intraparenchymal cavity or an air–fluid level in an intraparenchymal cavity; (2) those involving an air-containing cavity or intraparenchymal air–fluid level within the paravertebral lung; (3) those involving a small peripheral cavity or peripheral linear radiolucency, which is always close to the chest wall where a rib has been fractured; and (4) those resulting from a previously formed, firm pleuropulmonary adhesion that causes the lung to tear when the overlying chest wall is violently moved inward or fractured and is diagnosed only at surgery or autopsy.
lacerations into four types: (1) those involving an air-filled intraparenchymal cavity or an air–fluid level in an intraparenchymal cavity; (2) those involving an air-containing cavity or intraparenchymal air–fluid level within the paravertebral lung; (3) those involving a small peripheral cavity or peripheral linear radiolucency, which is always close to the chest wall where a rib has been fractured; and (4) those resulting from a previously formed, firm pleuropulmonary adhesion that causes the lung to tear when the overlying chest wall is violently moved inward or fractured and is diagnosed only at surgery or autopsy.
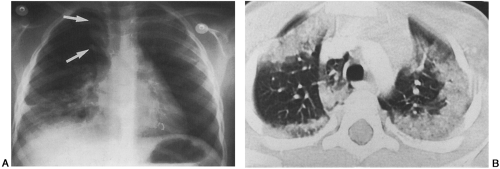
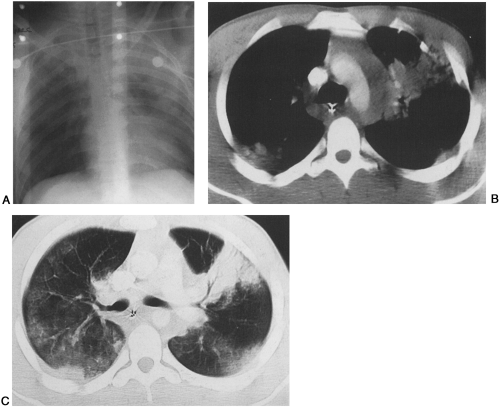
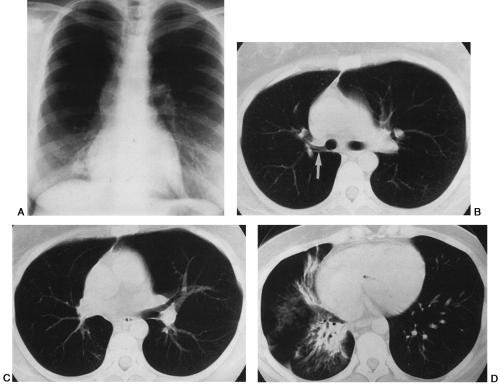
CT is more sensitive than radiography in demonstrating contusions and lacerations.122,156,160,172,183,197,200,205 On both chest radiographs and chest CT, pulmonary contusions appear as areas of consolidation or ground-glass opacification, or both, that tend to be peripheral, nonsegmental, and geographic in distribution (Figs. 31-2 and 31-3). Isolated pulmonary contusion in young, healthy patients is not associated with increased mortality.84 Contusions are evident at presentation or within 6 hours, and they resolve, often without permanent sequelae, within days to weeks. Pulmonary laceration, on the other hand, may initially be masked by coexistent contusion and other forms of chest injury on the chest radiograph or CT scan and generally takes weeks to months to resolve, sometimes with residual scarring (Fig. 31-4). Lung laceration results in disruption of alveolar spaces and formation of a cavity, usually filled with blood or air, and with consequent production of hematoma or pneumatocele. The CT diagnosis of lung laceration is based on the presence of a localized air collection within an area of consolidation after trauma.197
Tracheobronchial Injury
The incidence of tracheobronchial injury is reported to be 0.4% to 1.5% in clinical series of major blunt trauma and 2.8% to 5.4% in autopsy series of trauma victims.75 There is no initial radiographic evidence of tracheobronchial injury in 10% of patients.212 Failure to recognize tracheobronchial injury may result in death or allow cicatrization to occur, with airway obstruction arising days or months after initial injury (Fig. 31-5). More than 80% of tracheobronchial injuries occur within 2.5 cm of the carina.103,185 Rupture of the cervical trachea can occur as a “clothesline injury” when the neck is extended on high-speed contact with ropes, wires, or cables (e.g., in persons riding recreational vehicles or running). Tracheal laceration may also occur in a motor vehicle accident when the neck of a restrained driver strikes the top of the steering wheel, compressing the airway against the spine.
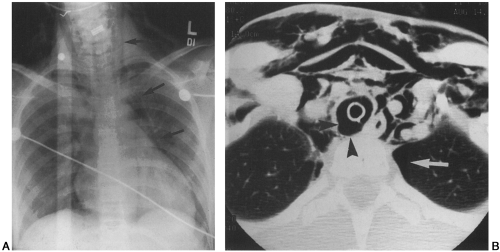
Injury to the mediastinal trachea or major bronchi produces mediastinal emphysema that rapidly extends into the neck and face and down to the shoulders and chest wall. When the thoracic trachea or bronchi are injured, the aorta is the most commonly associated injured structure.123 The most common radiographic findings of tracheobronchial injury
are subcutaneous and mediastinal emphysema (Fig. 31-6). A pneumothorax that does not resolve with functioning tube drainage is the sine qua non of mediastinal tracheal and major bronchial injury.102 The “fallen lung sign”145 is pathognomonic of bronchial tear and may be seen on chest radiographs and chest CT scans. This sign refers to the lung’s falling laterally and posteriorly in supine positioning and inferiorly away from the hilum in the erect position, as opposed to what occurs in pneumothorax without tracheobronchial injury, where the lung collapses toward the hilum. An indication of tracheal tear is elevation of the
hyoid bone above the level of C3 as seen on a lateral radiograph of the cervical spine.155 This is caused by injury to the infrahyoid musculature, which results in unopposed elevation of the hyoid bone by the suprahyoid musculature. Another sign of tracheal transection is acute overdistention of the endotracheal tube cuff. In tracheal rupture, the balloon may approach the endotracheal tube tip owing to distal expansion of the balloon in the tear, with partial herniation of the balloon in the tear as the tube moves in the airway or is repositioned.164 Another cause of acute overdistention of an endotracheal tube balloon is esophageal intubation.
are subcutaneous and mediastinal emphysema (Fig. 31-6). A pneumothorax that does not resolve with functioning tube drainage is the sine qua non of mediastinal tracheal and major bronchial injury.102 The “fallen lung sign”145 is pathognomonic of bronchial tear and may be seen on chest radiographs and chest CT scans. This sign refers to the lung’s falling laterally and posteriorly in supine positioning and inferiorly away from the hilum in the erect position, as opposed to what occurs in pneumothorax without tracheobronchial injury, where the lung collapses toward the hilum. An indication of tracheal tear is elevation of the
hyoid bone above the level of C3 as seen on a lateral radiograph of the cervical spine.155 This is caused by injury to the infrahyoid musculature, which results in unopposed elevation of the hyoid bone by the suprahyoid musculature. Another sign of tracheal transection is acute overdistention of the endotracheal tube cuff. In tracheal rupture, the balloon may approach the endotracheal tube tip owing to distal expansion of the balloon in the tear, with partial herniation of the balloon in the tear as the tube moves in the airway or is repositioned.164 Another cause of acute overdistention of an endotracheal tube balloon is esophageal intubation.
Diaphragm Rupture
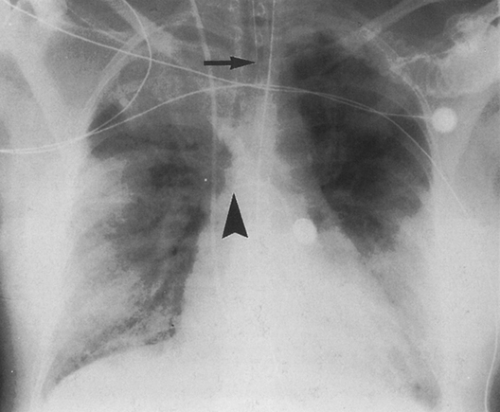
Acute diaphragmatic rupture occurs in 1% to 7% of patients after major blunt trauma,45,126,203 and the diagnosis is missed on initial presentation in up to 66% of these patients.7,44,62,85,100,210,213 Seventy-five percent to 95% of patients with acute rupture of the diaphragm have abnormal chest radiographs, but only 17% to 40% have highly suggestive radiographic findings.55,129,152 Plain-film findings of rupture include displacement of stomach, colon, or small bowel into the thorax (Fig. 31-7), superior displacement of an intragastric nasogastric tube, pleural effusion, basilar opacity causing inability to visualize the diaphragm, irregular or lumpy diaphragm contour, and fractures of the lower ribs.67 Rupture of the right hemidiaphragm, once thought to account for only 10% of all diaphragmatic ruptures, probably occurs with almost the same frequency as rupture of the left hemidiaphragm.67 If diaphragm rupture is not promptly diagnosed, the patient may remain asymptomatic or develop incarceration of herniated abdominal viscera, which can occur at a time remote from the incidence of trauma.
Helical CT has been shown to be useful in making the diagnosis of acute diaphragm rupture, and it is superior to conventional CT because volumetric data acquisition allows high-quality sagittal and coronal reformations. Acquisition
of data during a single breath hold decreases slice misregistration.91 Individual diagnostic sensitivity for detecting diaphragmatic rupture is 54% to 73%, and specificity is 86% to 90%.139 Direct CT findings associated with acute rupture include diaphragmatic discontinuity, intrathoracic herniation of abdominal contents, and waist-like constriction of bowel (the “collar sign”) (Fig. 31-8). Associated CT findings include liver laceration, hemoperitoneum, hemothorax, splenic laceration, renal contusion, lower-lobe atelectasis, and lower rib fractures. Although local discontinuity of the diaphragm is said to be the most common finding in patients with a diaphragmatic tear, it should be noted that there is a normal increase in diaphragmatic defects with age, not related to trauma. Caskey and colleagues23 found these normal localized defects in 13 patients (11% of patients studied). When the diagnosis of diaphragm rupture remains uncertain after CT or for delayed, nonacute, clinical, or radiologic presentation that suggests diaphragmatic injury, MRI should be done with T1-weighted sagittal and coronal sequences.174
of data during a single breath hold decreases slice misregistration.91 Individual diagnostic sensitivity for detecting diaphragmatic rupture is 54% to 73%, and specificity is 86% to 90%.139 Direct CT findings associated with acute rupture include diaphragmatic discontinuity, intrathoracic herniation of abdominal contents, and waist-like constriction of bowel (the “collar sign”) (Fig. 31-8). Associated CT findings include liver laceration, hemoperitoneum, hemothorax, splenic laceration, renal contusion, lower-lobe atelectasis, and lower rib fractures. Although local discontinuity of the diaphragm is said to be the most common finding in patients with a diaphragmatic tear, it should be noted that there is a normal increase in diaphragmatic defects with age, not related to trauma. Caskey and colleagues23 found these normal localized defects in 13 patients (11% of patients studied). When the diagnosis of diaphragm rupture remains uncertain after CT or for delayed, nonacute, clinical, or radiologic presentation that suggests diaphragmatic injury, MRI should be done with T1-weighted sagittal and coronal sequences.174
Injuries to the Bony Thorax
Significant injury to ribs, clavicles, scapulae, sternum, and spine can occur as a result of blunt chest trauma. Thoracic spine fractures account for 16% to 30% of all spine fractures and lead to complete neurologic deficits in 62% of patients.125,149 A supine chest radiograph provides an opportunity to evaluate the thoracic spine, but optimal evaluation requires frontal and lateral collimated films. Seventy percent to 90% of spine fractures can be seen on plain-film radiographs; CT and MRI may show otherwise occult fractures and are the only techniques to evaluate the integrity of the spinal cord and the intervertebral ligaments directly.68 CT and MRI are more helpful in distinguishing unstable burst fractures from stable, simple, anterior wedge compression fractures.8 Fractures to the upper ribs, clavicle, and upper sternum are significant in that they may be accompanied by brachial plexus or vascular injury in 3% to 15% of patients.65 Fractures of the lower ribs should increase suspicion of splenic, hepatic, or renal injury, which can be confirmed with CT. Double fractures of three or more adjacent ribs can result in the paradoxical motion of a “flail” segment during the respiratory cycle; this can impair respiratory mechanics and result in atelectasis and pulmonary infection. Rarely, a segment of lung herniates through a defect in the chest wall created by a flail segment. The diagnosis may be made by plain radiographs, but it is easier to detect by CT.133 Sternal fractures occur in 8% of major thoracic trauma admissions.77 The incidence of sternal fracture increases by 100% for drivers and 150% for front-seat passengers wearing seat belts compared with those not wearing seat belts,168 although the avoidance of other injuries is such that the use of seat belts is advocated. Sternal fracture may be associated with myocardial contusion, which is often clinically silent. Posterior dislocation of the clavicle can result in injury to the great vessels, superior mediastinal nerves, trachea, and esophagus. Although sternoclavicular dislocations are demonstrable using angled chest radiographs, they are more easily detected by CT (Fig. 31-9).133
Scapular fractures are diagnosed on the initial chest radiograph in only 57% of patients, according to one study.79 In the group of patients in whom the fractures were not recognized, the fracture was visible and overlooked in 72%, not included on the examination in 19%, and obscured by superimposed structures or artifacts in 9%. CT of the chest should demonstrate most scapular fractures, especially if it is used in combination with plain films. Scapulothoracic dissociation is a rare injury characterized by lateral displacement of the entire forequarter with intact overlying skin, complete acromioclavicular separation, and usually multiple fractures of the ipsilateral upper extremity; it usually is accompanied
by avulsion injuries of the brachial plexus and subclavian vessels.146
by avulsion injuries of the brachial plexus and subclavian vessels.146
Pleural Manifestations of Chest Trauma
Pneumothorax, as seen radiographically, occurs in almost 40% of patients with blunt chest trauma and in up to 20% of patients with penetrating chest injuries.6,29 All pneumothoraces in trauma patients should be considered potentially life-threatening, and chest tube placement should be considered. Even small pneumothoraces can rapidly enlarge and become clinically significant with positive pressure ventilation or general anesthesia. CT is much more sensitive for diagnosing pneumothorax in the supine patient than is chest radiography.198,206 CT scanning identifies pneumothoraces that cannot be seen on conventional supine radiographs in 10% to 50% of patients sustaining blunt trauma to the chest.198,206,214 Pneumomediastinum may occur in association with pneumothorax and can be diagnosed on chest radiography by the presence of streaky lucencies in the mediastinum that highlight the contours of the aorta and left main pulmonary artery and displace the mediastinal pleura laterally, and by the “continuous diaphragm sign” produced by the presence of air between the pericardium and the diaphragm. Pneumomediastinum can easily be identified on chest CT and may signal the presence of an underlying laceration of the pharynx, esophagus, or tracheobronchial airway.
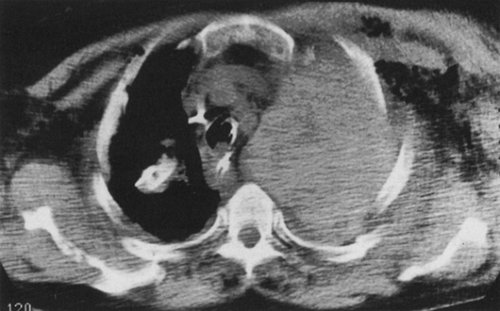
Pleural effusions developing in the acute post-traumatic setting usually represent hemothorax, and a rapidly expanding pleural effusion is most likely to be caused by arterial bleeding. CT can be helpful in distinguishing hematoma from other pleural collections by showing the high CT attenuation of blood134 (Fig. 31-10). CT can best distinguish pleural fluid from other causes of radiographic density such as atelectasis, parenchymal injury, or pneumonia and can show loculation of pleural fluid and better delineate complex pleuroparenchymal opacities.
Cardiac Trauma
Rapid accumulation of blood in the pericardial space often causes cardiac tamponade and severe hemodynamic compromise. Bedside sonographic evaluation of the heart is the study of choice to quickly and noninvasively detect pericardial fluid. CT is also very sensitive for detecting pericardial-space fluid, and pericardial hemorrhage may be indicated by the high CT attenuation of the fluid. Cardiac tamponade can be detected on CT by the distention of the inferior vena cava, hepatic veins, and renal veins and by development of periportal edema within the liver.133 Pericardial rupture is a rare consequence of thoracic trauma, with an incidence of only 0.11% in one series.52 The diagnosis can be made with chest radiography or CT when herniation of air-containing abdominal viscera into the pericardium accompanies diaphragmatic rupture. Pneumopericardium can occur when air enters through a pericardial disruption in the presence of pneumothorax.
Cardiac contusion results from blunt chest trauma in 8% to 76% of patients.87,165 The diagnosis usually is made by electrocardiography, nuclear cardiac imaging, or echocardiography. The right ventricle is most frequently injured, because it comprises almost three times more exposed anterior surface of the heart than does the left ventricle.133 Chest radiography and CT scanning may show evidence of congestive heart failure, ventricular aneurysm, or massive cardiac enlargement.
Soft-Tissue Injuries of the Chest Wall
CT scanning can easily distinguish chest-wall from parenchymal or mediastinal injury, whereas this differentiation may not be possible with chest radiography. Soft-tissue hematomas of the chest wall are readily differentiated from parenchymal injury, and subcutaneous emphysema is not confused with pneumothorax on CT scanning. Trauma to the female breast can be caused by a combination of compression and shearing stress produced by a seat belt. Subcutaneous rupture of breast tissue has been reported.40 CT scanning can show massive breast hematomas and rupture of silicone prostheses with silicone extravasation.153
Esophageal Injury
Esophageal disruption can occur from crushing of the esophagus between the spine and trachea, traction caused by hyperextension, and direct penetration by cervical spine fracture fragments.130 Chest radiography can show persistent severe pneumomediastinum or pneumothorax, left pleural effusion, a widened paraspinal line, and retrocardiac opacification. CT scanning can show similar findings in addition to leakage of oral contrast material from the disrupted esophagus into the mediastinum or pleural space and changes of mediastinitis.
Role of Computed Tomography in Chest Trauma
CT scanning has been shown to be superior to chest radiography in demonstrating many injuries to the chest from blunt and penetrating trauma. The identification of more pneumothoraces, hemothoraces, pulmonary contusions, and fractures on chest CT has not significantly affected the clinical management of patients in some series. CT has obviated the need for conventional aortography in a significant number of patients, and CT angiography may become the standard for the diagnosis of acute aortic injury. Further studies on a larger population of trauma patients is required to determine the sensitivity and specificity of CT for this diagnosis. CT scanning provides a look at the entire chest in addition to the aorta, which is a distinct advantage over transesophageal echocardiography or conventional aortography. In addition to showing fractures, CT also shows related soft-tissue injuries, such as great-vessel injury from fracture-dislocation of the clavicle or splenic laceration from adjacent rib fractures. CT of the chest can be performed in 30 seconds or less with helical scanners and reveals most injuries to the chest that are caused by acute trauma. Chest CT could be performed quickly on all trauma patients who are referred for abdominal or head CT, as a way of detecting serious chest injuries early.
PATIENTS IN THE INTENSIVE CARE UNIT: RADIOGRAPHIC CONSIDERATIONS
Patients hospitalized in intensive care units (ICUs) represent a population with unique and challenging medical problems. Because of the critical nature of the medical condition of patients in the ICU, radiographic studies usually are limited to portable, bedside examinations. Portable anteroposterior chest radiographs can be suboptimal owing to (1) poor patient positioning, including patient rotation; (2) inconsistent exposure technique, making comparison between serial radiographs difficult; (3) obscuration of pulmonary anatomy caused by portions of external monitoring and support devices overlying the patient; (4) limited exposure capability; (5) expiratory views; and (6) magnification and distortion of the mediastinum. Consistency in technique and positioning is important for optimal evaluation of patients on serial examinations. ICU nurse assistance in removing extrinsic tubing and other monitoring devices from the patient’s chest is critical to produce a satisfactory radiograph for evaluation of the lungs and mediastinum. Successful imaging in the ICU depends on the cooperative efforts of the nursing staff, radiology technologist, clinician, radiologist, and everyone involved in the ordering and transport of the radiograph.
Portable Film Technique
Optimal radiographic technique for anteroposterior chest radiographs includes upright positioning (when possible), exposure at deep-end inspiration, and a target-to-film distance of 40 to 50 inches for supine patients or 72 inches for erect patients.4,82 The kilovoltage should be between 72 and 100 kVp to optimize penetration and minimize the effects of scattered radiation. To minimize patient motion, mobile equipment should have adequate capacity to make a radiographic exposure in less than 0.1 second. Most constant-potential, battery-operated, or capacitor-discharge mobile units are capable of a 100- to 400-milliamperage (mA) output, and most chest exposures can be made at between 2 and 4 milliampere-seconds (mAs).59 A high-kilovoltage grid technique (125 kV, 10:1 grid, 40 line pairs/cm) can provide a longer scale of contrast and reduced repeat examinations by a factor of 6.157 Digital or computed radiography is becoming more popular as a portable chest radiography technique because of the consistent film quality and the wide latitude of exposure that is possible. The spatial resolution with computed radiography is inferior to that obtained with conventional radiography, but it is thought to be sufficient for the purposes of portable chest radiography.119
Accuracy and Efficacy of Portable ICU Films
The American College of Radiology (ACR) has provided working guidelines to improve the use of portable radiographs, embodied in the updated ACR Appropriateness Criteria.4 In addition, the ACR has defined efficacy of a test in terms of three components115: (1) diagnostic efficacy, or the utility of a test in assisting in diagnosis (e.g., evaluation of malposition of devices as well as cardiopulmonary findings); (2) therapeutic efficacy, or the effect of test results on patient management; and (3) outcome efficacy, or the ultimate contribution
of the test and its results to patient morbidity and mortality. Therapeutic (management) efficacy is difficult to evaluate, because patient management decisions often reflect clinical factors in addition to imaging findings. No studies exist on long-term outcome efficacy.
of the test and its results to patient morbidity and mortality. Therapeutic (management) efficacy is difficult to evaluate, because patient management decisions often reflect clinical factors in addition to imaging findings. No studies exist on long-term outcome efficacy.
Numerous studies have reported contradictory results regarding the efficacy of portable chest radiography,13,50,63,64,72,81,94,106,180 and a thorough review of efficacy studies was published by Henschke and colleagues.82 Reasons for contradictory results included differences in patient populations (e.g., surgical ICU, medical ICU, underlying patient medical condition and reason for hospitalization); number of studies and patients studied; types of films included in the study (e.g., all radiographs taken versus “routine” morning radiographs versus postprocedural radiographs); and criteria for determining whether an abnormality was present on a radiograph. Few studies attempted to address the issue of management efficacy, and in those that did there were differences in study design regarding how the clinical information was obtained and how it affected management apart from the influence of the radiographic findings. Although it seems intuitive that daily clinical conferences with experienced thoracic radiologists would contribute to the optimal utilization and interpretation of ICU radiographs, this has not been evaluated scientifically. In the ACR Standards, it is stated that “The radiologist should establish daily conferences or frequent consultations with attending physicians caring for ICU patients; in addition to the exchange of radiographic and clinical information, the appropriateness of the examination, as well as the accuracy of radiographic interpretation, should be evaluated during these sessions.”4
The overall incidence of abnormalities found on chest films in the ICU has been reported to be as high as 65%.81 Henschke and colleagues81 reviewed 1,132 chest films obtained from medical and surgical ICU patients, including routine morning radiographs as well as films taken for various clinical indications. New diagnostic information was revealed in more than 65% of the radiographs—including malpositioned endotracheal tubes (12%), malpositioned central venous catheters (9%), and changes regarding cardiopulmonary findings (44%)—which were thought to have a meaningful effect on patient management, although management efficacy was not formally evaluated. More recent studies have questioned the need for routine ICU chest radiographs. Fong and coworkers50 prospectively evaluated 1,003 chest radiographs obtained from 157 consecutive patients admitted to a surgical ICU and found that the likelihood of a clinically important finding was 17% for radiographs obtained for no clear clinical indication (routine), 26% for those obtained to verify the position of a medical device, and 30% for those obtained for suspected clinical conditions. Based on their findings, the authors concluded that chest radiographs should be obtained from surgical ICU patients only for specific indications, and that routine radiographs for ICU patients are justified only for patients with indwelling Swan-Ganz catheters. The radiologist’s interpretation was not a part of the study, and patient management decisions were based on both clinical and radiographic data. In a review of 525 routine morning chest radiographs of patients admitted to the surgical ICU of a university trauma center during a 1-month period, Silverstein and coworkers180 found a low yield of new findings for both medical device placement and cardiopulmonary pathologic processes. The design of the study did not include correlation of new or worsened radiographic findings with therapeutic changes. Based on available studies, the role of portable chest radiographs in the ICU needs further evaluation, especially regarding patient management and outcome efficacy.
Cardiopulmonary Abnormalities
Pulmonary parenchymal disease in the ICU is a common and challenging problem. The chest radiographic pattern is usually nonspecific, and the clinical causes of pulmonary opacities in a given patient are often multiple. For this reason, radiographic interpretation should be performed in conjunction with current clinical information.
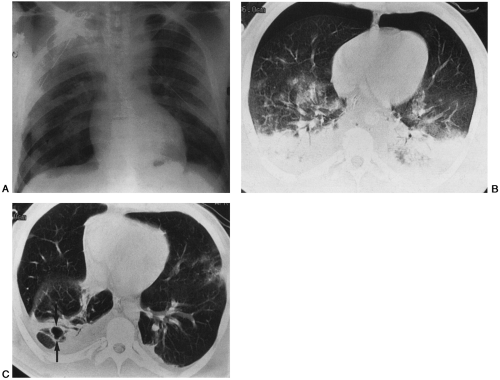
Pneumonia
The diagnosis of pneumonia is often made on the basis of fever and elevated leukocyte count in addition to new pulmonary opacification on chest radiograph. These findings may not be reliable in the ICU. The radiographic appearance of pneumonia in the ICU setting depends on patient age, duration of illness, underlying disorders (e.g., pregnancy, emphysema, malignancy), recent surgery, drug administration (e.g., antibiotics, steroids), and immune status.166 Previous chest radiographs are invaluable for assessing serial changes and help predict the cause of abnormal parenchymal opacification. Acute processes generally exclude neoplasm, and quickly resolving processes suggest atelectasis, hemorrhage, or edema as opposed to pneumonia. Even so, the overall accuracy of chest radiography for diagnosing pneumonia is only 0.50, and neither review of previous chest radiographs nor knowledge of clinical data improves this accuracy.211 Most hospital-acquired pneumonias are caused by gram-negative bacilli such as Pseudomonas aeruginosa or Serratia marcescens or by gram-positive cocci.170 ICU patients who develop pneumonia often have diffuse parenchymal opacification on chest radiographs, with either interstitial, alveolar, or mixed patterns (Fig. 31-11). This nonspecific appearance is seen with viral, bacterial, tuberculous, fungal, or protozoal infections. The pattern of disease is affected by underlying chronic lung disease such as emphysema or fibrosis. Resolution after therapy in these patients is often delayed.
Bronchopneumonia may result from aspiration of infected nasal, oral, or tracheal secretions; it often begins as acute bronchitis and bronchiolitis. The infection spreads through the walls of infected bronchioles into the alveoli. Most hospital-acquired pneumonias begin as bronchopneumonia and
are caused by a variety of gram-positive and gram-negative bacteria. Intubation leads to colonization of the proximal airways with a variety of bacteria, which can be spread throughout the bronchial tree with mechanical ventilation. The radiographic appearance of bronchopneumonia is that of multifocal, ill-defined opacities which may cause both narrowing of the bronchi and mucus plugging.166
are caused by a variety of gram-positive and gram-negative bacteria. Intubation leads to colonization of the proximal airways with a variety of bacteria, which can be spread throughout the bronchial tree with mechanical ventilation. The radiographic appearance of bronchopneumonia is that of multifocal, ill-defined opacities which may cause both narrowing of the bronchi and mucus plugging.166
In patients with bacteremia, hematogenous pulmonary dissemination appears radiographically as multiple, patchy, ill-defined, peripheral regions of consolidation that may show evidence of cavitation. CT scanning can be useful to show evidence of septic emboli, such as peripheral cavitary nodules, often with identifiable feeding vessels.
Interstitial pneumonia is often of viral origin and appears radiographically as increased reticular or linear markings, peribronchial cuffing, or nodules. A small nodular pattern can also be seen with disseminated tuberculosis or fungal infection. This pattern of disease can progress to diffuse involvement of both lungs, making etiologic predictions challenging.
CT scanning offers superior resolution and sensitivity for evaluating chest conditions in ICU patients154; CT can distinguish chest-wall from pleural, parenchymal, and mediastinal abnormalities much better than can chest radiography. In patients with suspected pulmonary infection, CT scanning can identify parenchymal abscesses and empyemas. The distinction between the two is important, because empyema requires chest tube drainage, whereas pulmonary abscess usually responds to antibiotic therapy. Chest CT scanning should be considered for ICU patients when the clinical course does not correlate with the chest radiograph and the patient is sufficiently stable to tolerate transportation to the radiology suite.