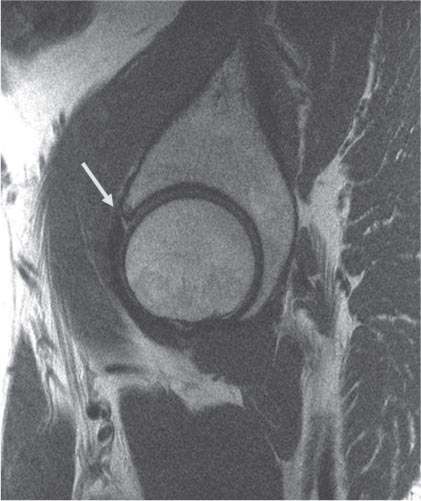
7 The Hip As with MRI of any anatomic region, accurate MRI assessment of the hip requires attention to technical detail. Traditionally, MRI of the hip performed for suspicion of osteonecrosis or an occult fracture used a large body coil within the magnet bore, which provided very poor in-plane resolution and little to no detail of the articular cartilage or labrum. More recently, surface coils have been used to evaluate the hip, providing much higher spatial resolution. However, initial body coil sequences of the entire pelvis are still helpful for screening for other etiologies of pain, such as the following: • Muscle strains • Pelvic masses • Hernias • Spine and sacroiliac joint pathology • Occult fractures At the authors’ institution, coronal inversion recovery and axial proton-density sequences are obtained using a body coil, followed by the use of a surface coil with cartilage-sensitive, intermediate TE, FSE pulse sequences in the coronal, sagittal, and axial planes, with high in-plane and segment resolution. The authors’ institution also prefers to use an intermediate TE sequence rather than T1-weighted and T2-weighted images for several reasons. First, T1 is not good for evaluating cartilage because there is no contrast between fluid and cartilage. Second, it is also not good for evaluating subtle muscle abnormalities, so another sequence in each plane would be required for a thorough evaluation, and yet a third for cartilage. The intermediate TE sequence eliminates that redundancy by allowing enough signal for excellent resolution and enough contrast to evaluate all the structures (bone, ligament, tendon, muscle, and articular cartilage) and the quality of synovitis, if present. One can obtain this sequence in each plane and then add one fat-suppressed sequence to evaluate for subtle findings and assess acuity. Many authors advocate using MR arthrography of the hip for the evaluation of labral pathology and articular cartilage (see Chapter 14),1–3 but this modality increases the cost and imaging time, and makes MRI an invasive procedure.4 Mintz et al.5 evaluated 92 patients before hip arthroscopy via an optimized protocol similar to that outlined above and concluded that noncontrast imaging can identify labral and chondral pathology. However, many institutions in the United States and abroad continue to use MR arthrography to improve the visualization of intraarticular hip pathology, especially labral pathology.6 The fibrocartilaginous labrum (type I collagen) appears as a triangular, low signal intensity structure attached to the rim of the acetabulum7 (Fig. 7.1). Labral pathology can be a cause of substantial hip pain (Table 7.1) and is associated with the development of osteoarthritis.8 The labrum surrounds the rim of the acetabulum nearly circumferentially and is contiguous with the transverse acetabular ligament across the acetabular notch. The labrum is thickest superiorly and posteriorly and widest anteriorly and superiorly. The joint capsule attaches to the acetabular rim adjacent to the labrum; however, at the superior aspect of the joint, the capsule inserts a few millimeters above the labrum, which creates a sublabral recess or sulcus.9 Neuroreceptors that provide proprioception have been identified, and there is a limited blood supply to the periphery of the labrum.10,11 Fig. 7.1 A sagittal FSE image of the hip showing a normal anterior labrum (left arrow) as a triangular focus of low signal and normal articular cartilage of the acetabulum (top arrow). (© 2009 Hospital for Special Surgery, New York, NY.)
 Specialized Pulse Sequences and Imaging Protocols
Specialized Pulse Sequences and Imaging Protocols
 Traumatic Conditions and the Athletic Hip
Traumatic Conditions and the Athletic Hip
Acetabular Labral Tears
Primary labral pathology | Nonmusculoskeletal causes |
Femoroacetabular impingement | Genitourinary |
Laxity | Spine |
Trauma | Psoas muscle abscess |
Dysplasia | Hernia |
Degenerative | Endometriosis |
Ovarian cyst | |
Peripheral vascular disease | |
Primary chondral | Unknown etiology |
Lateral impact | Transient osteoporosis of the hip |
Subluxation/dislocation | Bone marrow edema syndrome |
Osteonecrosis | |
Loose bodies | |
Degeneration | |
Primary capsule | Synovial proliferative disorders |
Laxity | PVNS |
Adhesive capsulitis | Synovial chondromatosis |
Synovitis/inflammation | Chondrocalcinosis |
Extraarticular | Infectious/tumor/metabolic |
Snapping hip (internal/external) | Septic arthritis |
Trochanteric bursitis | Osteomyelitis |
Ischial bursitis | |
Psoas bursitis | Neoplasms |
Osteitis pubis | Benign bone and soft tissue |
Sports hernia | Malignant bone and soft tissue |
Piriformis syndrome | Paget disease |
Sacroiliac joint | Primary hyperparathyroidism |
Tendinitis | Metastatic bone disease |
Hip flexor | |
Adductor | |
Abductor | |
Gluteus medius tear | |
Inflammatory | Systemic |
RA | Polyarticular |
Reiter syndrome | Reflex sympathetic dystrophy |
Psoriatic arthritis | Complex regional pain syndrome |
Bursitis | Hormonal |
Source: From Shindle MK, Ranawat AS, Kelly BT. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med 2006;25:309–326. Reprinted by permission.
Labral tears are diagnosed by the presence of increased signal intensity (often equivalent to that of synovial fluid) on fat-suppressed images through the substance of the labrum, with or without displacement (Fig. 7.2). Partial or complete detachment is characterized by fluid-matching signal undermining the attachment between the labrum and acetabulum. The presence of paralabral cysts should prompt careful inspection of the labrum to discern the often subtle splits that serve as the origin for these cysts (Fig. 7.3). Lecouvet et al.12 performed MRI of the hip in 200 asymptomatic individuals and showed that intralabral areas of high signal intensity communicating with the free surface increased with age.
To optimize outcomes, the underlying etiology of the injury must be identified. In addition to degenerative labral tears associated with arthritis, there are at least five causes of labral tears13:
• Femoroacetabular impingement
• Traumatic labral injury (dislocation/subluxation)
• Atraumatic capsular laxity (hypermobility)
Fig. 7.2 A sagittal FSE image of the hip showing a nondisplaced anterior labral tear (arrow). (© 2009 Hospital for Special Surgery, New York, NY.)
Fig. 7.3 A sagittal FSE image of the hip showing paralabral cysts associated with an anterior labral tear (arrow) and full-thickness cartilage loss of the anterior acetabulum. (© 2009 Hospital for Special Surgery, New York, NY)
• Psoas impingement
• Dysplastic labral tears
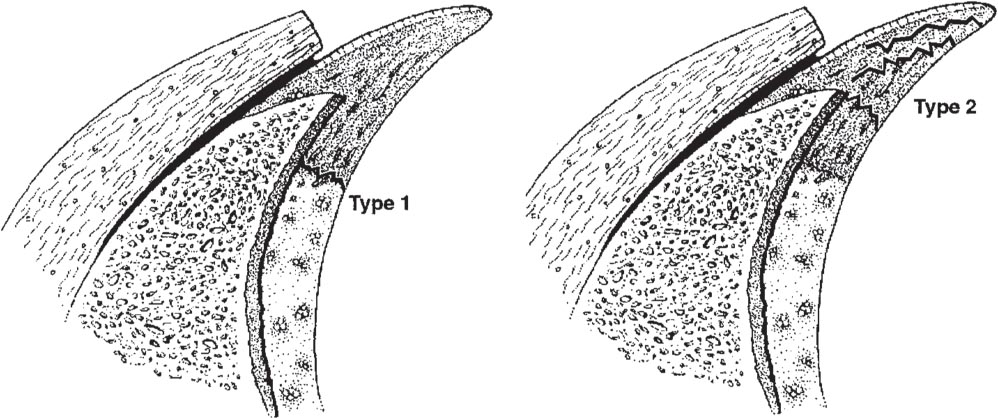
Several classification systems have been used for labral tears, two of which are described here. In a cadaveric study, Seldes et al.14 determined histologically that there were two distinct types of tears (Fig. 7.4):
• Detachment of the labrum from the hyaline cartilage at the transitional zone (type 1)
• Cleavage of variable depth within the substance of the labrum (type 2)
In another study, Lage et al.15 developed an arthroscopic classification based on morphology:
• Radial flap tear
• Radial fibrillated tear
• Longitudinal peripheral tear
• Unstable tear
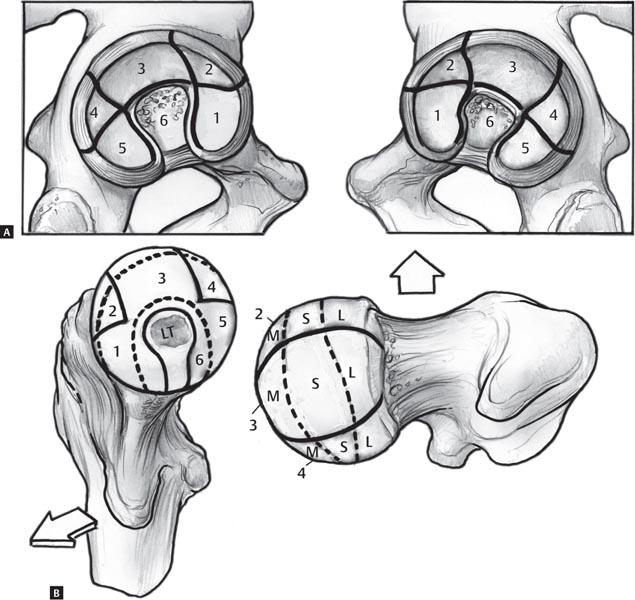
A recent article by Ilizaliturri et al.16 described a zone method with which to classify intraarticular pathology at hip arthroscopy (Fig. 7.5). Among a group of expert hip arthroscopists, the zone method was found to be more reproducible than the clock-face method.16
Two potential pitfalls may occur when interpreting non-contrast MRI and MR arthrography studies, potentially leading to an inaccurate diagnosis of a labral tear. First, there is a normal variant of the posteroinferior sublabral groove, which is a relatively common occurrence and typically seen on axial images.9 The clinician should recognize that this location is distinct from that of most labral tears. The second variant is a superior sublabral recess at the anterosuperior margin of the acetabulum, which has been described in the presence of mild acetabular dysplasia.17
The prevalence of labral tears in the anterosuperior labrum reportedly is high, and several authors have speculated that this tear may be secondary to decreased vascularity in this zone.13,14 In an evaluation of 12 hips from six cadavers, Kelly et al.13 used a modified Spalteholz technique to map the anatomic zones of labral vascularity. They reported that cadaveric specimens have relatively avascular hip labra, with no statistically significant (p >.05) differences among the anterior, superior, posterior, or inferior labral lesions, or in torn versus intact specimens. However, slightly increased vascularity was seen on the capsular compared with the articular side, suggesting that the vascularity usually is supplied by the capsule. Those authors also noted that all labral tears were associated with increased microvascularity at the labral base, adjacent to the attachment of bone. Such studies have important future implications for labral surgery in terms of determining the type and location of tears that would be amenable to successful repair, as opposed to arthroscopic debridement.
Fig. 7.4 Seldes type 1 and type 2 labral tears: detachment of the labrum from the hyaline cartilage at the transitional zone and cleavage of variable depth within the substance of the labrum, respectively. (From Seldes RM, Tan V, Hunt J, Katz M, Winiarsky R, Fitzgerald RH Jr. Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res 2001;382:232–240. Reprinted by permission.)
Fig. 7.5 Zone classification. (A) An artist’s depiction of the left and right hemipelves. The acetabulum has been subdivided into six zones: 1, anterior-inferior; 2, anterior-superior; 3, central superior; 4, posterior-superior; 5, posterior-inferior; and 6, acetabular notch. (B) An artist’s depiction of the left and right proximal femurs. (Left) The frontal view of the femoral head is divided into six zones around the acetabular fossa (there is a dotted line around the ligamentum teres [LT]): 1, anterior-inferior; 2, anterior-superior; 3, central superior; 4, posterior-superior; 5, posterior-inferior; and 6, area around the ligamentum teres. (Right) The superior view shows the three subdivisions of zones 2, 3, and 4: medial (M), superior (S), and lateral (L). (From Ilizaliturri VM Jr, Byrd JWT, Sampson TG, et al. A geographic zone method to describe intra-articular pathology in hip arthroscopy: cadaveric study and preliminary report. Arthroscopy 2008;24:534–539. Reprinted by permission.)
Stress Fractures
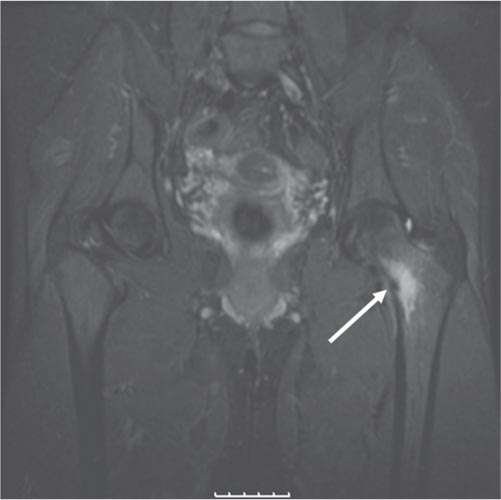
Stress fractures, which result from cyclic mechanical stress, can be subdivided into one of two groups: fatigue or insufficiency. Military recruits and athletes are more susceptible than the general population to fatigue fractures, given that they occur in normal bone that is exposed to a repetitive mechanical overload that overwhelms the normal remodeling process.18 Insufficiency fractures occur more commonly in the elderly secondary to osteoporosis, osteomalacia, or other processes that weaken the bone, permitting osseous failure to occur after fewer loading cycles than in normal bone. Insufficiency fractures in the athletic population have also been described in female athletes, in association with the female athletic triad.19 Stress fractures can occur on the compression or the tension side of the femoral neck.20 Compression stress fractures are more common and begin at the inferior cortex of the femoral neck. Tension stress fractures begin in the superior cortex, have a greater propensity to displace, and thus require more aggressive treatment. A fracture line with a benign periosteal reaction may be visualized on conventional radiography or CT, and bone scintigraphy may be sensitive but not specific for the diagnosis of femoral neck stress fracture. However, MRI is sensitive and specific to the presence of underlying bone marrow lesions, and a linear fracture line associated with the preservation of fatty marrow should be sought to confirm the diagnosis of a stress fracture.20,21 Fat-suppressed or STIR coronal images show a linear pattern of increased signal intensity, which is compatible with an acute or subacute fracture (Fig. 7.6). MRI is also useful for excluding underlying lesions, such as a tumor, or marrow disorders that may be the cause of a pathologic stress fracture.
Traumatic Posterior Subluxation/Dislocation/Lateral Impaction
A traumatic posterior hip dislocation most commonly occurs as a result of a motor vehicle accident when the hip and knee are flexed and the knee impacts on the dashboard, producing a posteriorly directed force on the hip. In the acute setting, MRI may aid in the diagnosis of the following22,23:
Fig. 7.6 A coronal fat-suppressed image obtained with a body coil technique, showing increased signal intensity (arrow) surrounding a stress fracture at the medial aspect of the left femoral neck. (© 2009 Hospital for Special Surgery, New York, NY.)
• Femoral head contusions
• Labral disruptions
• Sciatic nerve injury
• Intraarticular fragments
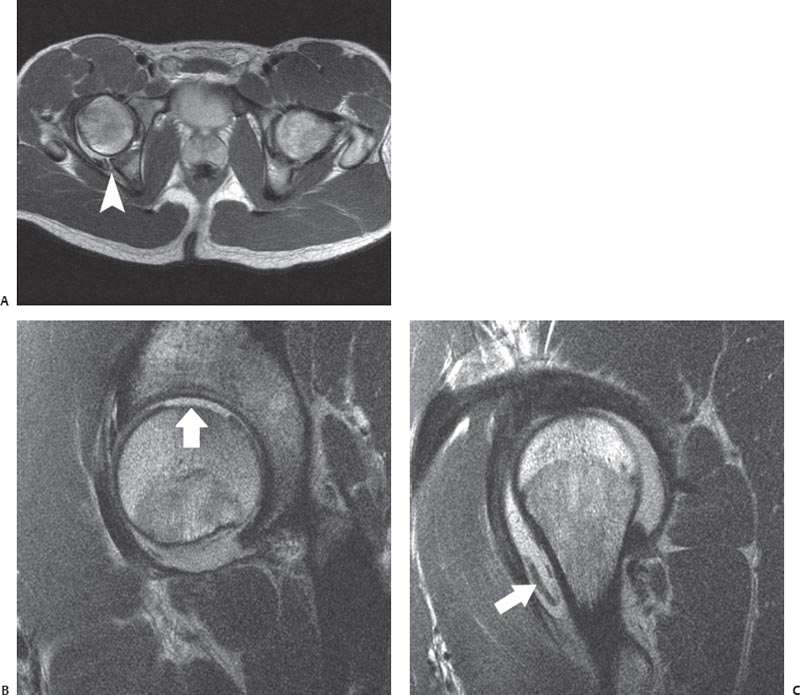
Hip subluxation usually has a more subtle presentation than does hip dislocation because of its lower energy mechanism of injury, such as a fall on a flexed hip and knee; however, subluxation is a potentially devastating injury that may be misdiagnosed as a simple hip strain or sprain. Traumatic posterior subluxation events in football or other high-level athletic activities may cause symptomatic cartilage-shearing injuries and labral tears, but they are not associated with radiographic documentation of a dislocation.24 Depending on the degree of force applied to the hip at the time of translation, the posterior labrum or wall may be displaced and/or combined with anterior labral tears, disruption of the iliofemoral ligament, and parafoveal cartilage shearing injuries; the latter two typically are sustained at the time of reduction (Fig. 7.7). MRI is also a useful tool for detecting the complication of osteonecrosis and for assisting in the determination of when athletes may return safely to sports activity24,25 (see Osteonecrosis, below). Byrd26 described a lateral impaction injury as a direct blow to the greater trochanter, resulting in isolated traumatic chondral injuries in young, physically fit individuals as a consequence of sports or activity. MRI is useful in this scenario for determining the extent of chondral damage and for evaluating the presence of osteochondral loose bodies.
Fig. 7.7 Posterior hip subluxation. Axial body coil (A) and sagittal surface coil (B,C)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree