The Pancreas
Kellie A. Schmidt
|
OBJECTIVES
Describe pancreatic surface anatomy, vascular supply, and the common relational landmarks.
Discuss the most common pancreatic congenital anomalies to include pancreas divisum, annular pancreas, and ectopic pancreas.
Identify the endocrine and exocrine functions of the pancreas.
Correlate laboratory values and clinical indications associated with pancreatic abnormalities, disease, and pathology.
Explain the sonographic evaluation of the pancreas to include patient preparation and protocol and demonstrate completing the examination procedure.
Differentiate normal from the varying sonographic appearances associated with pancreatic disease or pathology.
Describe the pathology, etiology, clinical signs and symptoms, and sonographic appearance for congenital diseases, inflammatory diseases, neoplastic diseases, and nonneoplastic cystic lesions.
KEY TERMS
acute pancreatitis
chronic pancreatitis
pancreatic carcinoma
phlegmon
pseudocyst
GLOSSARY
acini cells cells that perform exocrine functions secreting digestive enzymes
alpha cells cells that perform endocrine functions secreting glucagon
amylase enzyme that digests carbohydrates
beta cells cells that perform endocrine functions secreting insulin
delta cells cells that perform endocrine function secreting somatostatin
endocrine secreting into blood or tissue
exocrine secreting into a duct
glucagon hormone secreted by the alpha cells that functions to increase activity of phosphorylase
insulin hormone secreted by beta cells that functions to increase the uptake of glucose and amino acids by most body cells
islets of Langerhans endocrine portion of the pancreas made up of alpha cells and beta cells, which is the source of insulin and glucagon; also called pancreatic islet
lipase fat-digesting enzyme
phlegmon diffuse inflammatory reaction to infection spreading along fascial pathways, producing edema and swelling
pseudocyst an abnormal or dilated cavity resembling a true cyst but not lined with epithelium
somatostatin hormone secreted by delta cells that functions to regulate insulin and glucagon production
Sonographic imaging of the pancreas is often fraught with technical limitations, specifically overlying bowel gas. Although sonography may identify some pancreatic lesions, its primary use is often to identify abnormalities of other organs associated with pancreatic disease.
ANATOMY
The pancreas is a nonencapsulated structure that lies obliquely in the anterior portion of the retroperitoneum. It consists of three main portions: the head, body, and tail. The head is located to the right and inferior to the body and tail. It has the largest anteroposterior (AP) dimension of the gland and is bordered by the C-loop of the duodenum1 (Fig. 9-1).
Extending posterior and medial from the head is a curved projection of pancreatic tissue, the uncinate process. The uncinate process lies anterior to the inferior vena cava and posterior to the superior mesenteric vein (SMV). The body and tail of the pancreas are bounded anteriorly and superiorly by portions of the stomach, duodenum, and left lobe of the liver.
The body of the pancreas lies anterior to the aorta, superior mesenteric artery (SMA), and left renal vein. Between these vessels and the body of the pancreas, the splenic vein may be identified as it courses from the spleen, toward its confluence with the SMV.
The neck of the pancreas lies just anterior to this confluence, where the SMV and splenic vein merge to form the portal vein. In many patients, the left lobe of the liver lies between the body and the anterior abdominal wall. Branches of the celiac axis—namely the hepatic, left gastric, and splenic arteries—course along the superior border of the body.
The tail of the pancreas extends from the body into the left anterior pararenal space. Bordered posteriorly by the splenic vein, it frequently extends to the splenic hilum. The tail is bordered anteriorly by the stomach and laterally by the left kidney. Because of its proximity to the stomach, the pancreatic tail is often obscured by gas on sonography.
The parenchyma of the pancreas consists of small groups of acini, which secrete digestive enzymes, clustered in multiple lobules, each surrounding a tributary duct. The smaller ducts merge into increasingly larger ducts, subsequently emptying into the main pancreatic duct, the duct of Wirsung. Enzymes secreted by the pancreas are carried by the main pancreatic duct into the alimentary tract via the ampulla of Vater. Near the ampulla, the main pancreatic duct merges with the distal common bile duct to form a single perforating channel into the duodenum (Fig. 9-2). A smaller accessory duct, the duct of Santorini, branches from the main pancreatic duct and perforates into the duodenum separately from the ampulla.2
Wedged within the acinar lobules are groups of endocrine cells known as the islets of Langerhans. These clusters contain various types of cells that release hormones directly into the bloodstream and lymph system. This allows them to be distributed throughout the body, where they stimulate other organs or functional tissues.
Blood supply to the pancreas is provided by branches of the splenic artery and the pancreaticoduodenal arteries. The superior pancreaticoduodenal artery arises from the gastroduodenal artery and perfuses the head of the pancreas. The gastroduodenal artery arises from the common hepatic artery and perforates the pancreatic parenchyma along the superior aspect of the head.3 The body and tail sections of the pancreas are perfused by the inferior pancreaticoduodenal artery, which arises from the SMA. Branches of this and the splenic artery enter the pancreas at numerous points along the body and tail.4
Congenital Anomalies
Congenital anomalies of the pancreas are rare, but do exist. Pancreas divisum is the most common congenital anomaly, occurring in approximately 4% to 14% of the population.5 It results from a failure of fusion of the dorsal and ventral pancreatic buds during embryologic development (Fig. 9-3). This variant results in anomalous drainage of the pancreatic ducts, but it is usually not associated with any significant sequelae.5
An annular pancreas is another congenital anomaly in which the head of the pancreas surrounds the second portion of the duodenum (Fig. 9-4). It occurs more frequently in males and has been associated with complete or partial atresia of the duodenum. Annular pancreas is associated with other congenital abnormalities in up to 70% of affected infants.6 This includes duodenal stenosis or atresia, Down syndrome, tracheoesophageal fistula, gastrointestinal anomalies, and congenital heart disease.6,7
Ectopic pancreatic tissue may also occur. The reported incidence ranges from 0.5% to 13.7%.8 In this setting, pancreatic tissue grows in other organs. This usually occurs in the walls of the stomach, duodenum, large or small intestine and rarely in the gallbladder, spleen, or liver. Ectopic pancreatic structures may be comprised of acinar and ductal elements. Because they are functional deposits of pancreatic tissue, they are susceptible to developing acute pancreatitis or tumor.
 FIGURE 9-2 Diagram showing the relationship of the common bile duct and main pancreatic duct as they merge and enter the ampulla of Vater. (Asset provided by Anatomical Chart Co.) |
PHYSIOLOGY
The pancreas is responsible for both endocrine and exocrine functions.
Endocrine Function
The endocrine function of the pancreas consists of hormone production, which occurs in the islets of Langerhans. Specialized cells, referred to as alpha, beta, and delta cells, are contained within the islets of Langerhans. Each is responsible for the production of specific hormones. The majority of these cells are beta cells, which produce insulin. Insulin aids in the metabolism of carbohydrates. By facilitating the transport of glucose across cell membranes, insulin increases the energy available for normal physiologic functions. It also influences the metabolism of proteins and fats. Insulin is released by the pancreas via a negative feedback mechanism. When the blood glucose level rises above a certain level, believed to be 100 mg/dL, the beta cells immediately secrete insulin.9 When the blood
glucose level falls, insulin secretion decreases. Other factors influencing insulin secretion include autonomic nervous system responses, the release of other endocrine hormones, and certain drugs.10 Abnormalities of insulin secretion result in impairment of metabolic functions throughout the body. Diabetes results from an imbalance between insulin secretion and the metabolic needs of the body.
glucose level falls, insulin secretion decreases. Other factors influencing insulin secretion include autonomic nervous system responses, the release of other endocrine hormones, and certain drugs.10 Abnormalities of insulin secretion result in impairment of metabolic functions throughout the body. Diabetes results from an imbalance between insulin secretion and the metabolic needs of the body.
Glucagon, secreted by alpha cells within the islets of Langerhans, is another important hormone. It functions primarily in the liver and aids in conversion of glycogen into glucose, or usable energy. As with insulin, blood glucose levels initiate the release of glucagon.
Delta cells comprise the smallest component and are responsible for producing somatostatin, a hormone involved with regulating the production of insulin and glucagons.
Exocrine Function
The exocrine function of the pancreas is to secrete enzymes, commonly referred to as pancreatic juice, that aid in food breakdown and digestion. These secretions accumulate in small intercellular spaces and the acini cells and are eventually transported to the duodenum via the excretory ducts. Chemical analysis of pancreatic juice shows that in addition to digestive enzymes, it consists of water and inorganic salts such as potassium, sodium, and calcium.
The enzymes secreted by the pancreas are amylase, lipase, trypsinogen, and chymotrypsinogen—all of which are essential to the digestion and absorption of essential nutrients. Amylase breaks down complex carbohydrates into usable sugars; lipase is an enzyme that breaks down fats; and trypsinogen and chymotrypsinogen are preproteolytic enzymes that reduce proteins to their component amino acids. Additionally, some of these substances play an important role in the pathogenesis of pancreatic disease, especially in pancreatitis. The preproteolytic enzymes in the normal pancreas are inert. It is postulated that an inhibiting factor is secreted by the same cells that secrete exocrine enzymes. This inhibiting factor prevents trypsinogen and chymotrypsin from autodigesting the protein in the cell walls of the pancreas. With injury or disease, the inhibiting factor is unable to prevent the activation of proteolytic enzymes, which spill out into the surrounding parenchyma. Once the process begins, it can advance rapidly, each bursting cell releasing yet more digestive juice, reducing normal tissue to amorphous fluid.11 Another component of pancreatic juice is the alkaline substance bicarbonate, which neutralizes the acidic gastric enzymes and triggers the action of the otherwise inert pancreatic enzymes in the duodenum. The pancreas is capable of secreting about 1,500 mL of pancreatic fluid per day.12
LABORATORY VALUES
Amylase
Amylase is an enzyme essential in the digestion of carbohydrates. The level of amylase within the blood is a useful laboratory test when diagnosing pancreatic disease. In a diseased pancreas, disintegrating acinar cells release their digestive enzymes into the organ’s parenchyma, and ultimately into the capillaries that supply the diseased area. Amylase levels can be accessed with either serum or urine analysis. Normal values vary from laboratory to laboratory.
Serum amylase is considered elevated when the value is three or more times the normal reference range.13 Levels usually begin to increase within 5 to 8 hours following the first onset of clinical symptoms.14 They usually reach a maximum level within the first 1 to 2 days of disease onset, and often persist until the underlying cause is treated.15 Amylase elevation is also associated with pancreatic duct obstruction, pancreatic malignancy, and biliary disease. Other non-pancreas related processes may also cause an increased amylase level, such as perforated ulcers, bowel obstruction, and some cancers, but it is not commonly used to monitor these entities. With chronic pancreatitis, it is not uncommon for amylase levels to be normal or only slightly elevated.
An increased amylase level in the urine may lag behind the onset of an increased serum amylase. Additionally, in the setting of pancreatitis, urine amylase may remain elevated for up to 7 days after serum values have returned to normal. Elevation of the serum amylase without concurrent elevation of the urinary amylase value may represent a pathologic process not related to pancreatic disease such as decreased renal function.16 Drugs such as aspirin, diuretics, alcohol, and oral contraceptives may also cause an increased amylase level.
Lipase
Lipase is a fat-splitting enzyme excreted by the pancreas. It is released into the bloodstream in increased quantities in the setting of inflammatory, and occasionally neoplastic, pancreatic disease. With acute pancreatitis, lipase levels may be 5 to 10 times the normal reference range. Lipase levels increase rapidly within 3 to 6 hours of onset, peak at 24 hours, and remain elevated for 1 to 2 weeks.19 Lipase elevation also occurs in patients with obstruction of the pancreatic duct, pancreatic carcinoma, acute cholecystitis, cirrhosis, and severe renal disease.20 Drugs associated with an increased lipase value include codeine, indomethacin, and morphine.
Fat Excretion
Fecal fat excretion values reflect the amount of undigested fat molecules passing through the alimentary tract. Increased fecal fat (steatorrhea) is symptomatic of pancreatitis. Other abnormalities may also result in an increased discharge of fat into fecal matter, including celiac disease, inflammatory bowel disease, or short bowel syndrome. However, fat excretion is increased significantly in pancreatic disease.21 Weight loss and oily stool are often associated with pancreatic steatorrhea.
Bilirubin and Liver Function Tests
An elevation of bilirubin and other liver function values may also occur with pancreatic disease.22 This is due to
the close anatomic relationships between the liver and biliary system with the pancreas. Pathologic processes in one structure may cause disease in the other. Neoplasia or inflammatory enlargement of the head of the pancreas frequently causes stenosis or complete obstruction of the distal common bile duct. In such cases, total serum bilirubin values are increased. Conversely, biliary duct disease, such as calculi and subsequent inflammation, may spread to the pancreas. Altered biliary and hepatic function values may suggest an underlying pancreatic process.
the close anatomic relationships between the liver and biliary system with the pancreas. Pathologic processes in one structure may cause disease in the other. Neoplasia or inflammatory enlargement of the head of the pancreas frequently causes stenosis or complete obstruction of the distal common bile duct. In such cases, total serum bilirubin values are increased. Conversely, biliary duct disease, such as calculi and subsequent inflammation, may spread to the pancreas. Altered biliary and hepatic function values may suggest an underlying pancreatic process.
SONOGRAPHIC EVALUATION
Indications
The pancreas is usually sonographically evaluated as part of a complete abdominal sonography examination. Common indications include epigastric pain, abdominal pain, abdominal distension, or jaundice. Patients with abnormal laboratory values or a prior history of acute or chronic pancreatitis may also be referred for sonography. Sonography is not considered the best imaging test to evaluate for pancreatic disease or neoplasm, but it may be very useful in identifying secondary signs of a pancreatic process such as dilated biliary ducts, fluid collections, and gallstones.
Preparation
Preparation for pancreatic sonography attempts to minimize the amount of gas in the stomach and duodenum by having the patient refrain from eating or drinking anything for 8 to 12 hours prior to the examination. Pancreatic sonography is contraindicated for patients who have undergone gastroscopic examination within 6 hours because large amounts of air are introduced into the stomach during this procedure. The head of the pancreas is intimately related to the duodenum. Gas present here as well as the overlying transverse colon may easily obscure visualization.
It is also recommended that the pancreas be the first organ evaluated when performing a complete sonographic evaluation of the abdomen. This is because patients are often asked to perform deep inspiration during the course of the examination. This often improves visualization of abdominal organs by displacing them caudally. However, it also increases the amount of air within the bowel, which in turn obscures visualization of the pancreas.
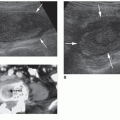
Transverse Imaging
In the transverse plane, the pancreas is identified as a crescent-shaped structure draping over the prevertebral vessels (Figs. 9-5 and 9-6). It has been described variously as horseshoe-, dumbbell-, or comma-shaped.23 Normally, its echogenicity is equal to or greater than that of the liver, depending on the patient’s age and body habitus.24 Fat deposition in the interlobular areas accounts for the varying degrees of echogenicity and in some settings may cause contour alterations.25 Children normally have less pancreatic fat than adults, so a hypoechoic pancreas in a pediatric patient is a normal finding.26 In the adult population, a hypoechoic pancreas represents an abnormal finding.1
The main pancreatic duct, the duct of Wirsung, is frequently visualized sonographically in normal patients.27,28 It appears as an echogenic lucency bordered by two parallel linear echoes traversing the body of the pancreas29 (Fig. 9-7). In the normal population, the pancreatic duct diameter is usually 3 mm or less.4 The normal pancreatic duct mean diameter has been found to measure 3 mm in the head, 2.1 mm in the body, and 1.6 mm in the tail.4 The contour of the duct walls should be smooth without any areas of focal dilatation.30 Color Doppler is useful in distinguishing the pancreatic duct from surrounding vascular structures.
The accessory pancreatic duct, the duct of Santorini, is not commonly seen. The duct of Santorini drains the head of the pancreas.
The dimensions of the pancreas are best assessed using a true transverse plane of section. It is important to align the transducer so that the incident beam intersects the pancreas perpendicular to its transverse axis. This is usually a slight obliquity, with the head of the pancreas slightly lower than the tail.
 FIGURE 9-7 Transverse image of the pancreas showing a normal main pancreatic duct (arrowhead). The duct of Wirsung. |
Pancreatic size can vary considerably from individual to individual.4 The head of the pancreas is the widest portion of the gland, with the normal AP dimension measuring between 2 and 3.5 cm3 (Fig. 9-8). The body of the pancreas is narrower and normally measures between 2 and 3 cm23 (Fig. 9-9). The tail may be difficult to image from a projection that provides a true AP measurement; but in the normal gland, it measures 1 to 2 cm31 (Fig. 9-10). A child’s pancreas is smaller than an adult’s, but relative to other upper abdominal organs such as the liver and kidneys, it may appear larger. Size, texture, and contour are all important considerations in identifying pancreatic disease.
 FIGURE 9-8 Transverse image of the pancreas showing normal caliper placement for measuring the head of the pancreas. |
 FIGURE 9-9 Transverse image of the pancreas showing normal caliper placement for measuring the body of the pancreas. |
In the transverse plane, the common bile duct should be seen in cross section entering the head of the pancreas.
Longitudinal Imaging
On a longitudinal section, the pancreas is identified as an ovoid or circular structure lying anterior to the prevertebral vessels (Fig. 9-11). From a slightly oblique longitudinal section, the common bile duct may be seen entering the pancreatic head (Fig. 9-12). Anterior to the bile duct, the gastroduodenal artery is visualized. The neck of the pancreas appears as a narrow structure just anterior to the confluence of the
SMV and the splenic vein. The body can be seen anterior to the SMA and posterior to the left lobe of the liver. In a true longitudinal section through the left anterior pararenal space, the tail appears thicker than the other portions because it is being transected as it dips posteriorly.
SMV and the splenic vein. The body can be seen anterior to the SMA and posterior to the left lobe of the liver. In a true longitudinal section through the left anterior pararenal space, the tail appears thicker than the other portions because it is being transected as it dips posteriorly.
 FIGURE 9-10 Transverse image of the pancreas showing normal caliper placement for measuring the tail of the pancreas. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree