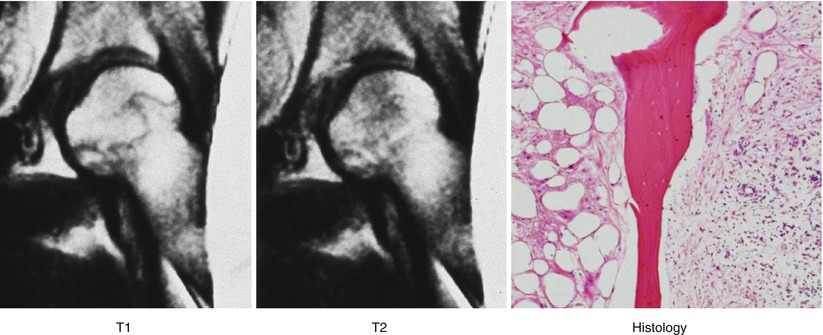
Fig. 19.1
Zone formation in ON. A wedge-shaped necrotic area is seen in a subchondral area, which is surrounded by the reparative tissue. This reparative tissue continues to the normal viable bone and bone marrow tissue. In the early phase of ON, the reparative tissue generally consists of infiltration macrophage, granulation tissue, and fibrous tissue, which can only be recognized on MRI. Thereafter, bony repair such as an appositional bone formation or creeping substitution occurs, when radiograph can detect these bony changes as a sclerotic change
In the early phase of ON, the reparative tissue generally consists of infiltration macrophage, granulation tissue, and fibrous tissue (cellular repair tissue), which can only be recognized on MRI. Thereafter, bony repair such as an appositional bone formation or creeping substitution occurs, when radiograph can detect these bony changes as a sclerotic change (Fig. 19.1). MRI is thus useful for the detection of ON in the early phase. In another word, MRI is useful for the detection of early reparative tissue formed around ON [7].
19.3 Pathology of Osteonecrosis
Macroscopically, the articular surface generally undergoes flattening (Fig. 19.2). On the cut section, opaque yellow, wedge-shaped osteonecrosis is observed in a subchondral region, which is bordered by an irregular reparative zone, comprising granulation and fibrous tissue as well as the sclerotic cancellous bone (Fig. 19.3). In general, a fracture (crescent sign) is present at the subchondral region [8].
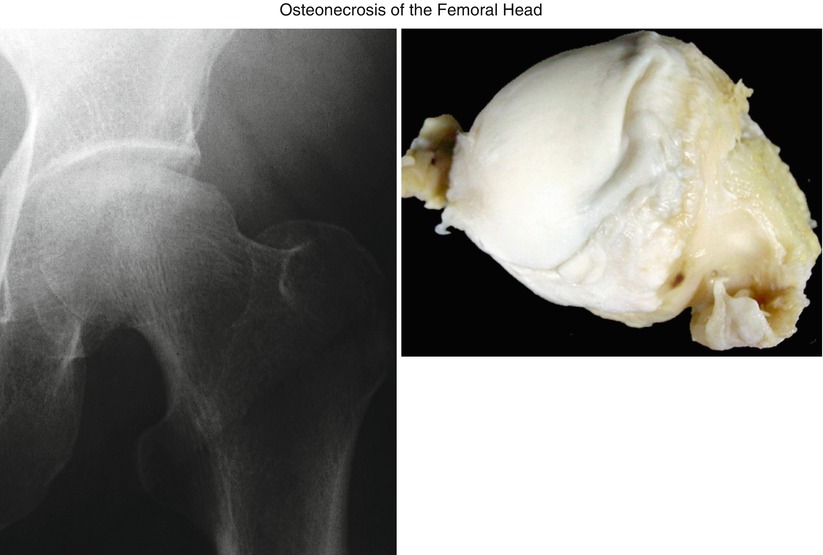
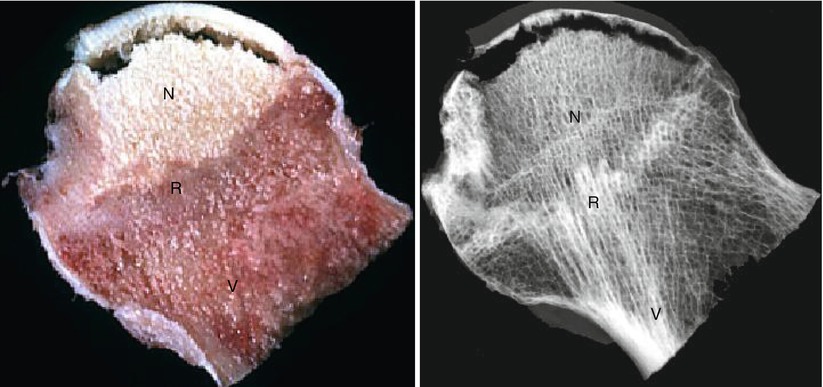
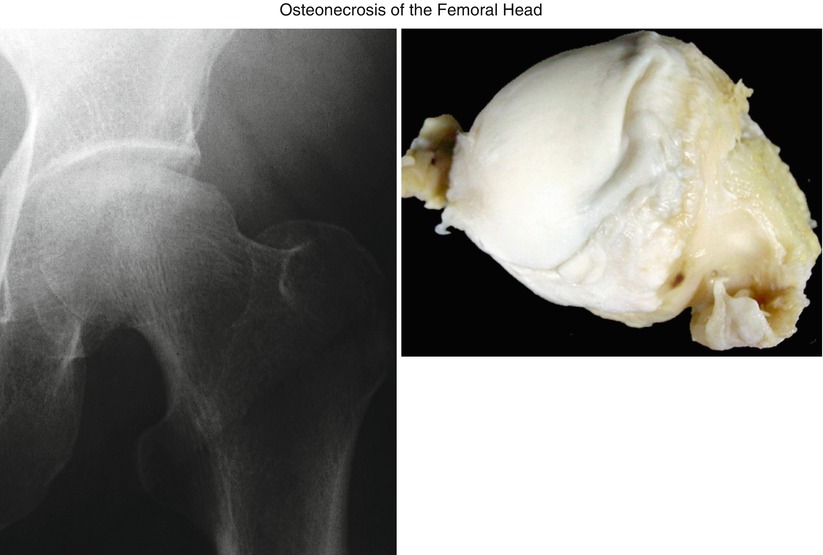
Fig. 19.2
ON often undergoes subchondral collapse, and the resected femoral head also shows the collapsed lesion at the lateral portion of the femoral head
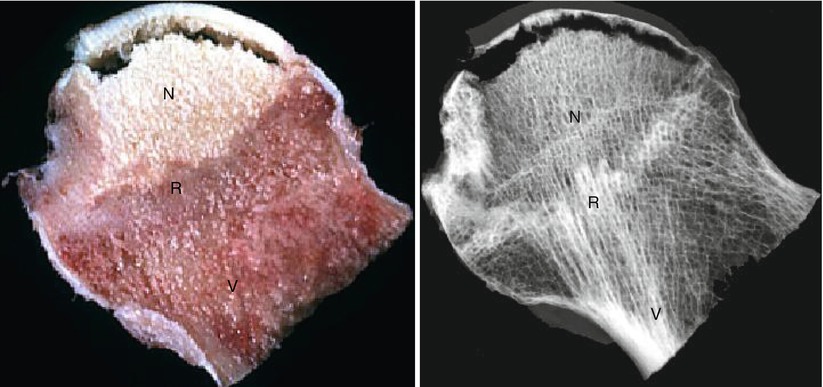
Fig. 19.3
The cut section shows wedge-shaped yellowish necrotic area (N), which is surrounded by the somewhat whitish reparative tissue (R). The reparative tissue continues to the viable normal area (V). The specimen radiograph also demonstrates the zone formation, comprising necrotic (N), reparative (R), and viable area (V)
Microscopically, typical necrotic area shows an accumulation of bone marrow cell debris and bone trabeculae demonstrating empty lacunae occasionally containing some pycnotic nuclei of osteocytes (Fig. 19.4). At the periphery of this necrotic lesion, repair process such as vascular-rich granulation tissue and appositional bone formation is observed. This appositional bone formation caused the thickening of the bone trabeculae in the reparative area (Fig. 19.5) [5, 6].

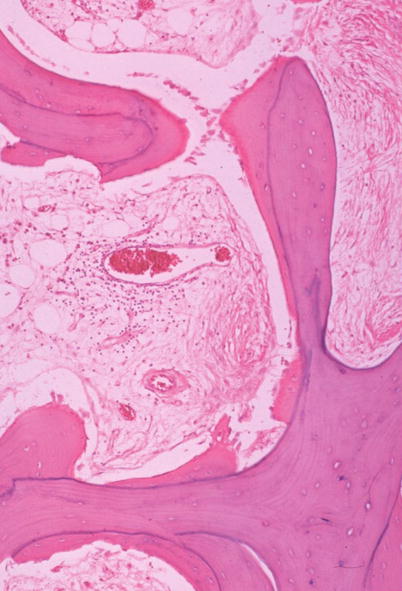

Fig. 19.4
Histology of the necrotic area. Necrotic area shows an accumulation of bone marrow cell debris and bone trabeculae demonstrating empty lacunae occasionally containing some pycnotic nuclei of osteocytes (HE ×100)
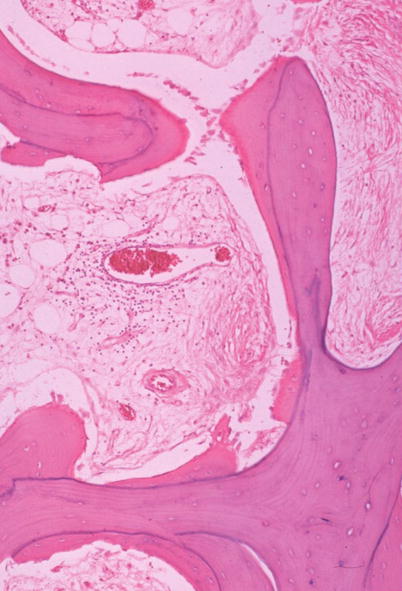
Fig. 19.5
Histology of the reparative zone. In the repair zone, appositional bone formation is seen along the necrotic bone trabeculae, and vascular-rich granulation tissue is seen in the marrow space (HE ×200)
19.4 Crescent Sign
In ON, a subchondral fracture is often observed, which is generally called as a “collapse” or “crescent sign” [8]. This sign pathologically corresponds to a space formed between the fractured lesion (Fig. 19.6). Histologically, the fractures generally occur at the junction between the thickened trabecula associated with appositional bone formation and the necrotic bone trabecula [9].
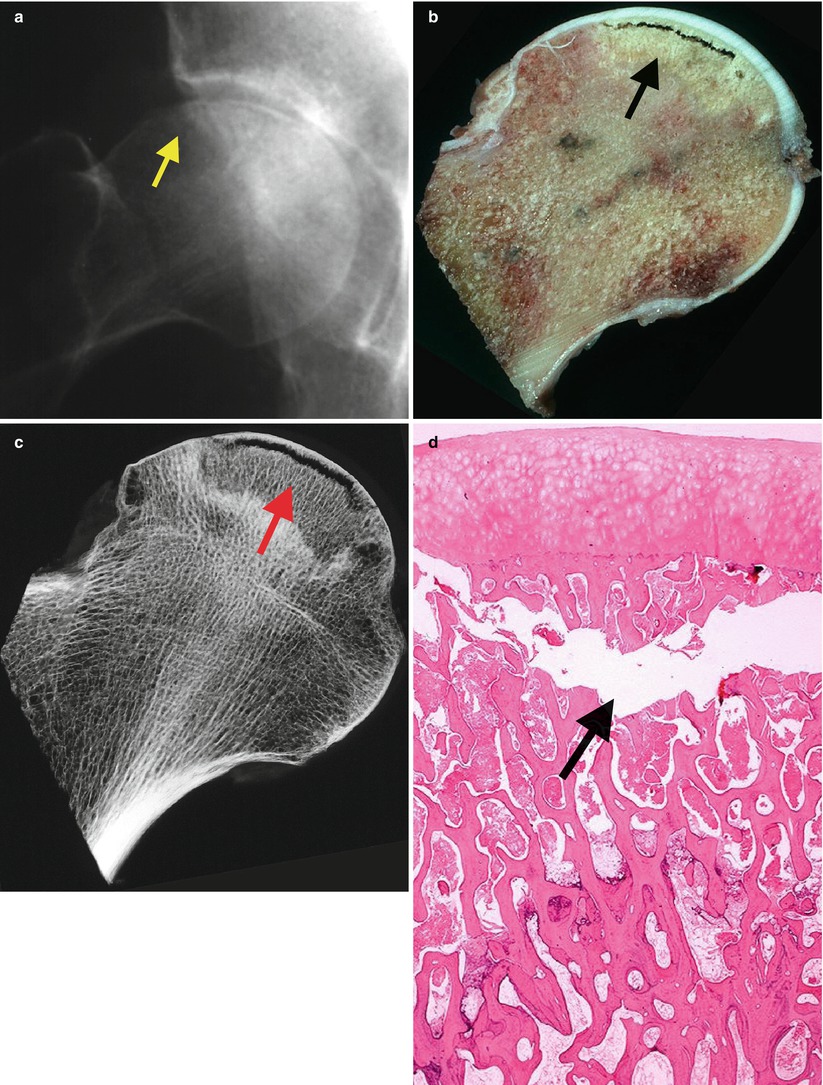
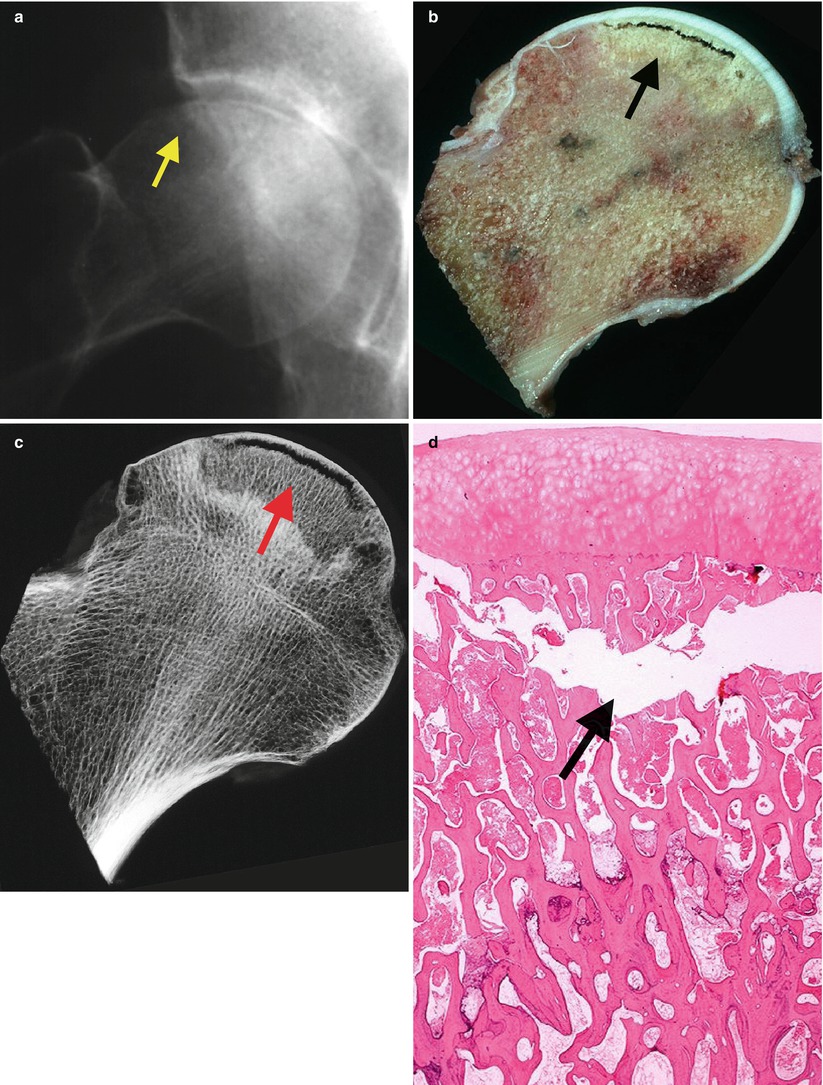
Fig. 19.6
(a) Radiographic appearance of subchondral collapse or so-called crescent sign (arrow). (b, c) On the cut section, subchondral collapse is seen just beneath the articular cartilage (black arrow), and on the specimen radiograph a subchondral fracture is clearly seen in the corresponding area (red arrow). (d) This area pathologically corresponds to a space formed between the fractured lesion
As to the mechanisms of a collapse, the following three causes are proposed: (1) the cumulative effect of microfractures induced by fatigue within the necrotic zone, (2) weakness of trabeculae in the reparative front due to osteoclastic activity, or (3) focal concentration of stress at the junctions between the thickened sclerotic trabecula of the reparative zone and the necrotic trabecula [5].
19.5 Initial Sign of ON
There has been a confusion regarding the initial sign of ON on MRI. Some reports describe that bone marrow edema pattern is the early finding of ON [10, 11]; however, it should be noted that an initial MR finding of ON is a low-intensity band on the T1-weighted images (Fig. 19.7) [7]. In the early phase of ON, the repair tissue formed around the necrotic area consists of accumulation of serofibrinous exudate and cellular-rich granulation tissue, which can be recognized as a band-like lesion surrounding the necrotic area [6, 7].