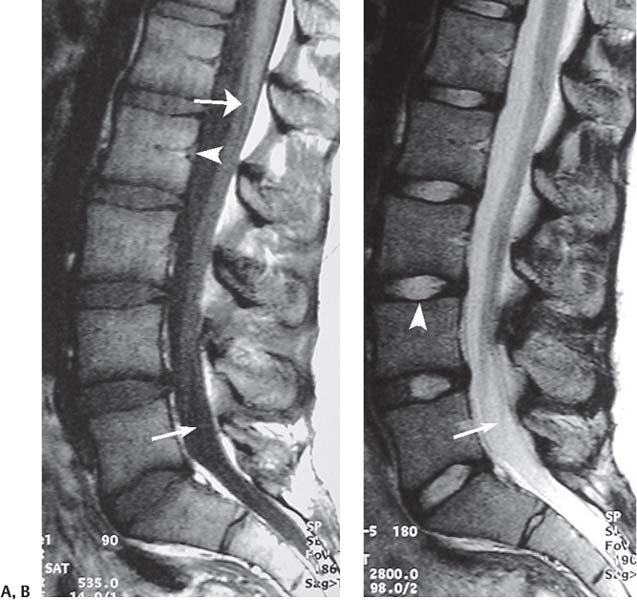
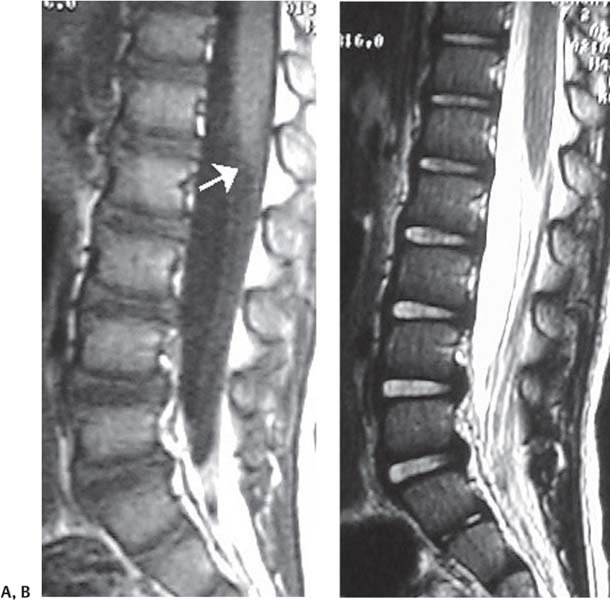
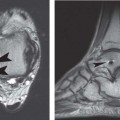
13 The Pediatric Spine Standard pulse sequences for spinal imaging include SE T1-weighted and FSE T2-weighted images. The FSE technique allows for the acquisition of T2-weighted images without prolonged imaging times. T1-weighted images allow for the evaluation of anatomic detail, including that of the osseous structures and soft tissues. T2-weighted images are primarily used to evaluate the spinal cord and enhance lesion conspicuity. Because CSF is bright on T2-weighted images and the spinal cord retains its intermediate signal, the T2-weighted images maximize the CSF to neural tissue contrast and therefore allow optimal delineation of the spinal cord and nerve roots. T2-weighted images are very sensitive to pathologic changes in tissue, including any processes in which cells and the extracellular matrix have increased water content. This pathologic change is usually shown as an increase in signal intensity on T2-weighted images, which increases the conspicuity of most pathologic processes affecting the spine. Open MRI systems are becoming more frequently used, especially for pediatric imaging. Although these systems often have significantly lower field strengths than closed magnets and thus usually produce studies of inferior overall quality, the open environment provides young patients with access to their parents and makes the experience less intimidating for patients with claustrophobia. Open systems are also helpful for procedures that might benefit from MRI guidance. When possible, however, the authors recommend that MR imaging be performed using closed 1.5-T or 3-T MRI systems. Formal sedation is often required for the successful MRI evaluation of the pediatric patient, and multiple studies and reviews have evaluated and recommended specific sedation protocols.1,2 The American Academy of Pediatrics has published guidelines for the elective sedation of pediatric patients,3,4 but compliance with these guidelines is not mandatory. The American Academy of Pediatrics has stated that careful medical screening and patient selection by knowledgeable medical personnel are needed to exclude patients at high risk for life-threatening hypoxia.4 Also, monitoring using their guidelines is necessary for the early detection and management of life-threatening hypoxia.3 The American Academy of Pediatrics recommends that, before examination in which sedation is to be used, children up to 3 years old should ingest nothing by mouth for 4 hours, and children 3 to 6 years old should ingest nothing by mouth for 6 hours.4 Although multiple protocols exist for the specific administration of various mediations for pediatric sedation and practices vary among institutions, a few agents are essential for most sedation protocols. Oral chloral hydrate is recommended for children less than 18 months old. However, the use of oral chloral hydrate is controversial because of its variable absorption, paradoxical effects, and nonstandardized dosing regimen. Older or larger children usually receive intravenous pentobarbital with or without fentanyl. Although several studies have reported the successful administration of sedation by trained nurses,1,2 patients who may benefit from the expertise of an anesthesiologist include those with substantial comorbidities, such as the following: • Cardiopulmonary disease • Skeletal dysplasias • Neuromuscular disease • Abnormal airway anatomy An important consideration after sedation for pediatric MRI is the need for strict adherence to established discharge criteria, including the following5: • Return to baseline vital signs • Level of consciousness close to baseline • Ability to maintain a patent airway Because of the potential risks associated with anesthesia and sedation in the young patient, there is a trend toward referring pediatric patients who require sedation to hospitals with pediatric anesthesiologists. Alternate techniques include sleep deprivation and rapid, segmental scanning; the latter permits the acquisition of high-quality images without the use of sedation. The surgeon referring pediatric patients for MR images of the spine should be familiar with the sedation protocols and level of expertise at the selected facilities. It is important to note that sedation protocols vary greatly from institution to institution and that no protocol is 100% safe, which emphasizes the need for monitoring, careful patient selection, and evaluation. The authors advise consultation with the pediatric anesthesiologists at the referring physician’s institution when sedating patients for MRI studies. To better understand and predict the MRI appearance of pathologic processes involving the spine, one should have a basic understanding of the normal MRI anatomy.6 Because most orthopaedic surgeons are more familiar with the normal anatomy of the adolescent (Fig. 13.1) and adult spines than with that of the pediatric spine, the salient points of the former two are presented first as a framework for understanding and differentiating the pediatric spine (for a full discussion of adult spine anatomy, see Chapter 2). The lumbar spine is the most frequently imaged region in both children and adults. The lumbar spinal canal transitions from a round appearance in its proximal portion to a more triangular one distally. The lumbar facet joints are covered with 2 to 4 mm of hyaline cartilage. This cartilage can be nicely visualized on FSE pulse sequences and with gradient-echo pulse sequences. The epidural space and ligaments should also be carefully evaluated. The epidural fat is seen as high signal intensity on T1-weighted images; the ligamentum flavum shows minimally higher T1-weighted signal than do the other ligaments. The conus medullaris, usually located at the L1-L2 level, is best seen as a regional enlargement of the spinal cord on the sagittal images. The filum terminale extends from the conus medullaris to the distal thecal sac. The traversing nerve roots pass distally from the conus medullaris and extend anteriorly and laterally. These nerve roots exit laterally underneath the pedicle and into the neural foramen. The intervertebral disc, consisting of the cartilaginous end plates, annulus fibrosus, and the nucleus pulposus, normally shows increased T2 signal in its central portion. It is important to note that CSF pulsations often create artifacts that degrade the image of the lumbar spine; those artifacts must not be mistaken for a pathologic process. Evaluation of the cervical spine begins with the vertebral bodies. A mild lordosis is noted on sagittal images. On axial images, the spinal canal is triangular, with the base located anteriorly. It is important to note the normal variant dark band at the base of the dens that represents a remnant of the subdental synchondrosis; it should not be mistaken for a fracture. In adults, the facet joints are small and triangular, whereas in children they are relatively larger and flat. The spinal cord is elliptical in cross-section in the cervical spine. It is important to recognize that there is a difference in signal between the normal gray and white matter of the spinal cord. This signal heterogeneity should not be mistaken for intramedullary pathology. The intervertebral discs are similar in appearance to, but smaller than, those seen at the thoracic and lumbar levels. An important anatomic feature of the cervical spine is the prominent epidural venous plexus, which is not present in the thoracic or lumbar spine. Fig. 13.1 Normal lumbar spine in a 16-year-old girl. (A) A sagittal T1-weighted image shows dark CSF (arrow with small head), the conus medullaris terminating at the L1-L2 level (arrow with large head), and the basivertebral channel (arrowhead). Note the normal rectangular appearance of the vertebral bodies and the lumbar lordosis. (B) A sagittal T2-weighted image shows bright CSF (arrow) and a bright nucleus pulposus (arrowhead). Understanding the normal adult and adolescent spine leads to appreciation of the dynamic development of the pediatric spine. The MRI appearance of the growing spine is quite complex. Multiple substantial changes occur in the vertebral ossification center and the intervertebral discs that markedly alter the overall appearance of the spine, especially between infancy and 2 years of age.7 In general, the vertebral ossification centers are incompletely ossified early in childhood, and the discs are thicker and have a higher water content than those in the adult. The spinal canal and neural foramina are larger, and there is less curvature. In addition, the overall signal intensity of the vertebral bodies is lower than that of the adult spine on T1-weighted images because of the abundance of red (hematopoietic) marrow relative to yellow (fat) marrow in the pediatric, adolescent, and young adult spine. By understanding the MRI appearance of this development process, the clinician is better equipped to differentiate normal from pathologic states. Sze et al.7 have characterized the MRI evolution of the pediatric spine between infancy and 2 years of age, and Goske et al.6 have described this dynamic process through the age of 10 years (see details later). In the newborn, the overall size of the vertebral body is small relative to the spinal canal, and the spinal cord ends at approximately the L2 level. The lumbar spine does not show the usual lordosis and is straight. The vertebral bodies show markedly low signal intensity on T1-weighted images, with a thin central hyperintense band that likely represents the basivertebral plexus. The spongy bone of the ossification center is ellipsoidal rather than rectangular and is often mistaken for a disc. The intervertebral disc is relatively narrow and often contains a thin, bright central band on T2-weighted images that represents the notochordal remnants. At 3 months, the osseous component of the vertebral body has increased and the amount of hyaline cartilage has decreased, with a resultant rectangular appearance to the vertebral bodies. The ossification centers begin to increase in signal intensity, starting at the end plates and progressing centrally. The neural foramina have not substantially changed at this age, remaining relatively large and ovoid in shape. At 2 years, the spine has begun to show its normal curvature, most likely because of the effects of weight bearing (Fig. 13.2). The ossified portion of the vertebral body increases substantially in size and begins to assume its adult appearance, with near-complete ossification of the pedicles and the articular processes. The disc space and nucleus pulposus become longer and thinner. The cartilaginous end plate has decreased in size and is often difficult to identify. The neural foramen also begins to take its adult appearance as its inferior portion narrows. At 10 years, the spinal curvature resembles that of an adult (Fig. 13.3). The ossification of the vertebral bodies and posterior elements is nearly complete, with a resultant decrease in the spinal canal diameter. The vertebral bodies also develop concave superior and inferior contours. The nucleus pulposus becomes smaller at this age and spans approximately half of the disc space in the sagittal plane. The neural foramina continue to narrow inferiorly. The spinal cord extends to the inferior aspect of the osseous spinal column in early fetal life.6 Because of the more rapid longitudinal growth of the vertebral bodies relative to the spinal cord, the conus medullaris is repositioned in the upper lumbar spine by birth. It is important to note the location of the conus medullaris on every pediatric spine MRI study (Figs. 13.1 and 13.2). A conus level below the L2-L3 interspace in children more than 5 years old is abnormal and indicates possible tethering.8,9 Saifuddin et al.10 reviewed the MRI findings of 504 normal adult spines and found that the average conus position was the lower third of L1 (range, middle third of T12 to upper third of L3). Fig. 13.2 Normal lumbar spine in a 2-year-old boy. (A) A sagittal T1-weighted image shows rectangular vertebral bodies and a wide, thin intervertebral disc. Note that the conus medullaris terminates at the L1-L2 level (arrow). (B) A T2-weighted image shows increased disc signal.
 Specialized Pulse Sequences and Imaging Protocols
Specialized Pulse Sequences and Imaging Protocols
 Pediatric Sedation Protocols
Pediatric Sedation Protocols
 Normal Pediatric MRI Anatomy
Normal Pediatric MRI Anatomy
Adolescents and Adults
Children
Differences Between the Pediatric and Adult Spine
Full-Term Infant
Age: 3 Months
Age: 2 Years
Age: 10 Years
Conus Medullaris
 Pathologic Processes Involving the Pediatric Spine
Pathologic Processes Involving the Pediatric Spine
Infection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree