Fig. 24.1
A hybrid algorithm in the approach to CTO PCI
Setting Up for Success
Review of the Diagnostic Angiogram
A very careful review of the diagnostic angiogram is important, and it is not unusual to spend up to 30 min scrutinizing every aspect of the available information, especially when first attempting retrograde procedures. Focus initially on antegrade and retrograde ostial diameters and orientations for selecting the proper guiding catheters. The length of the CTO is often overestimated based upon single catheter injection, but one should attempt to get a sense of length to formulate a strategy ahead of time. Collateral sources both epicardial and septal should be carefully assessed as potential retrograde conduits, paying particular attention to tortuosity, location, entrance, and exit angles as discussed later in this chapter. Both collateral size and distal vessel filling will often be more prominent with injections through large-caliber guiding catheters, so be aware that all usable options may not be fully delineated until one performs dual-injection guiding catheter angiography.
Vascular Access
All procedures start with proper vascular access, and while considered a footnote in many texts on CTO PCI, we should emphasize the importance of starting with the right access for the right job. In fact, a theme of our approach is to bring every advantage to bear at each step along the way, both in terms of enhancing procedural efficiency and success. The first choice is radial versus femoral, and while CTO PCI has traditionally been performed via the femoral route, reasonable technical success with perhaps lower access site complications has been described with radial access [10, 11]. The principal limitation of radial access for retrograde PCI is not only the operators comfort with radial procedures in general but also the requirement for double-guide access with a lot of support, especially for the retrograde catheter as we will describe. It is for this reason that we will focus our discussion on the femoral approach. For those wishing to pursue the radial approach, it is highly recommended that the operator currently perform greater than 90 % of the procedures radially and understand the limitations of smaller guiding catheters.
Seven or ideally eight French sheaths should be placed in each femoral based on the choice of guiding catheter size as described below. We advocate long, reinforced sheaths to improve passive support to the guiding catheters as well as torque ability in patients with peripheral vascular disease. The use of long sheaths increases passive support and comes with minimal consequences.
Guiding Catheter Selection and Setup
Support-type guides including the “extra backup” for the left coronary and Amplatz shape for the right coronary are useful, but guide selection should not be dogmatic, and careful scrutiny of the diagnostic angiogram is important in this respect. For example, Judkins right guides may be more appropriate for a very proximal RCA occlusion in which a more aggressive guide has a higher risk of proximal dissection. We recommend at least seven and if allowable by ostial size 8 French guiding catheters both for support considerations and equipment delivery. While 6 French catheters can certainly be used successfully for CTO PCI, one is somewhat more limited in the ability to use trapping techniques, multiple over-the-wire (OTW) devices, and with respect to overall guide support especially for the retrograde guide [12]. If review of the diagnostic angiogram suggests a small ostium, the use of side holes should be considered for the antegrade guide. There are two reasons for considering an antegrade side-hole guide: First, although damping during the procedure is not likely to be clinically relevant because the vessel is chronically occluded, hydraulic coronary dissection from injections can occur with a “damped” guide. This becomes increasingly more likely once an antegrade subintimal dissection has been created when performing reverse CART, which will be discussed later in this chapter. The use of side holes may not be justified with the retrograde guide. Any damping should be recognized promptly as donor vessel ischemia puts a large territory of myocardium at risk (including the collateralized territory), and hemodynamic compromise may ensue. The need for active retrograde guide management during delivery of devices, as well as the tendency for it to deep seat during removal of equipment, makes quick recognition of donor vessel ischemia important. If bilateral guides are engaged into the two native coronary ostia, it is advisable to place the left coronary guide first and then the right to avoid displacing the RCA catheter. “Access/guide consistency,” such as always putting the antegrade guide in the right femoral and retrograde guide in the left femoral, can help to avoid accidentally injecting via the antegrade guide at the wrong time, e.g., after antegrade subintimal ballooning but prior to distal recanalization, and creating a hydraulic dissection. Acquiring short guides or the ability to shorten a guide is important for retrograde procedures especially when planning to externalize a guidewire (see section “Retrograde Operators Toolbox” below).
Although many cardiac catheterization laboratories use the Tuohy-Borst hemostatic valve, retrograde procedures in particular use devices such as the Corsair Catheter and Tornus, which require rotational motions for advancement. This can lead to significant blood loss because of the need for an open valve for free rotation of the devices. Therefore, we recommend the COPILOT (Abbott) or Guardian II (Vascular Solutions) valves, both of which allow free rotation of OTW devices while maintaining hemostasis. Power injectors, though useful for improving efficiency and possibly contrast utilization, can be potentially dangerous when injecting into the antegrade guide at high pressure and can result in hydraulic dissections. Therefore, we feel a manifold, at least for the antegrade guide, should be considered when performing CTO procedures.
Procedural Anticoagulation
Patients should be preloaded with aspirin and clopidogrel in advance of the procedure. Most CTO operators advocate unfractionated heparin (UFH) as the sole anticoagulation strategy and avoidance of GP IIB/IIIA inhibitors or bivalirudin because of the intrinsically higher risk of perforation compared to traditional PCI and the ability to rapidly reverse UFH with protamine if needed. The retrograde or antegrade guide may be dormant for prolonged periods of time depending on the stage of the procedure. This increases the risk of thrombus formation in the guide, and for this reason, we recommend keeping the activated clotting time (ACT) above 350 s, and the staff systematically alert the operator every 30 min to obtain another sample. Donor vessel thromboembolism from the retrograde guide can be particularly disastrous as a large area of myocardium is at risk (both donor and recipient territories). Additionally, when drawing an ACT, it is advisable to do so from the most recently dormant guiding catheter as that will provide an opportunity to flush that guide and thus decrease the risk of thrombus formation within the guide catheter (Table 24.1).
Table 24.1
Vascular access and guiding catheter quick tips
7 or 8 French access depending on guide catheter size |
Consider 8 French guiding catheters based on ostial coronary diameter |
Side holes are useful for the antegrade guide, avoid for retrograde |
Practice “Access/Guide Consistency” – antegrade right, retrograde left |
Use a plunger-type hemostatic valve to decrease blood loss |
Avoid power injectors |
Use heparin alone for procedural anticoagulation – ACT >300 |
Collateral Angiography
A careful evaluation of collaterals is critical to the planning and success of the retrograde approach. Ideally, good collateral angiography should be performed at the time of diagnostic angiography in all patients with a CTO. This will allow the operator the time to carefully review candidate collaterals offline. Collaterals can be classified according to the Rentrop classification: grade 0 = no visible filling of any collateral channel, grade 1 = filling of the side branch of the occluded artery, grade 2 = partial filling of the occluded vessel, or grade 3 = complete collateral filling of the occluded vessel up to its occlusion [13].
Werner et al. have also described a collateral connection (CC) classification: CC0 = collateral with no visible connection to the recipient artery, CC1 = tiny or faint CC connections, and CC2 = small vessel-like connections (Fig. 24.2) [14]. Whether dedicated collateral angiography is performed during the diagnostic or at the time of intervention, some basic guidelines apply. Cineangiograms should be acquired in angulations intended to maximize the exposure of the collateral origin from the donor vessel and associated side branches, course of the collateral, and distal anastomosis with the CTO vessel (Table 24.2) (Fig. 24.3). During acquisition, low magnification and the avoidance of panning improve the resolution of very faint collaterals.
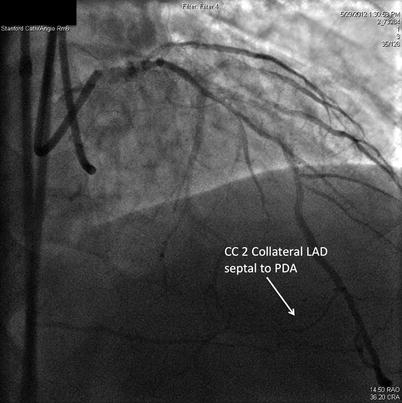
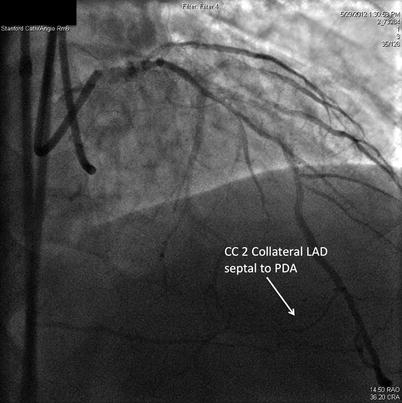
Fig. 24.2
An example of a CC2 or “side branch-like” collateral. In this case, a distal LAD septal which provided excellent access to the PDA for retrograde CTO PCi
Table 24.2
Collateral angiography
Artery | Artery | Collateral | Primary angulation | Secondary angulation |
|---|---|---|---|---|
LAD | PDA | Septal-septal | RAO cranial | RAO caudal |
LAD | PDA | Apical epicardial | LAO caudal | LAO/AP cranial |
CTX | RCA | AV groove epicardial | LAO cranial | RAO caudal |
OM | Diagonal | Epicardial | RAO caudal | LAO cranial |
Fig. 24.3
Guide shortening. In order to shorten an 8 Fr guide, we start with trimming and cutting the appropriate length, usually at least 10 cm from the guiding catheter near the proximal hub. Then, cut out a 2–3 CM section from a 7 Fr sheath. An 8 Fr dilator is used to flare out the 7 Fr sheath on both ends in order to accept the 8 Fr guiding catheter. Finally, the 7 Fr sheath joint is pushed over both ends of the cut guiding catheter to make the shortened guide
Retrograde Operators Toolbox
While we could generate an extensive list of equipment used by experts in retrograde CTO, our goal is to focus on a tenable amount of options for one lab to stock and retrograde-specific needs. Short retrograde guides are a necessity for these procedures, as standard length guides will often not allow the Corsair or other support catheters to reach the antegrade guide via collaterals. Full reach of the support catheter from retrograde guide to antegrade guide is required if one wishes to externalize the guidewire to facilitate recanalization. 90 cm guides are available for most curves, or alternatively a standard guide can be shortened (Fig. 24.4). With respect to guidewires, we advocate simplifying the inventory to five classes of wires as these will provide you with all the tools needed to successfully navigate a CTO, will improve your familiarity with a limited amount of equipment, and are more feasible from an inventory and purchasing perspective. The five classes of wires required include a soft-tipped tapered polymer-jacketed wire (i.e., Fielder XT), a soft-tipped non-tapered polymer-jacketed wire (i.e., Fielder FC), a stiff tipped non-tapered polymer-jacketed wire (i.e., Pilot 200), a stiff-tipped tapered unjacketed wire (i.e., Confianza Pro 12), and an externalization wire (RG 3 or ViperWire Advance). The Fielder XT can be used to probe for microchannels within the CTO, or it can be used as a “knuckle” wire to facilitate subintimal tracking. Wires specific to retrograde collateral crossing are non-tapered polymer-jacketed wires such as the Fielder FC, Whisper, or Pilot 50 and occasionally a tapered polymer-jacketed wire such as the Fielder XT. Recently, a new dedicated collateral wire has been developed, Sion and Sion Blue; these wires have a unique double-core, core-to-tip design with exposed wire coils that may improve access through epicardial collaterals. The Pilot 200 is useful for crossing the CTO and if it enters the subintimal space can also be knuckled to allow for subintimal tracking. The Confianza Pro 12 should be used for directed puncture when anatomic ambiguity is minimal or during a wire-based reentry technique. For wire externalization techniques, the RG3 is a dedicated 330 cm 0.010″ wire developed for this purpose but may not be available globally. Other choices include a long stiff wire such as the ViperWire Advance (335 cm). The rota-floppy wire (325 cm) is long enough and can be used for this purpose but is more prone to kinking and therefore should only be used if another more suitable wire is not available. In addition to an externalization wire, a snare may be needed to grab the retrograde wire tip from the aortic root or retrograde guide to help externalize a guidewire.
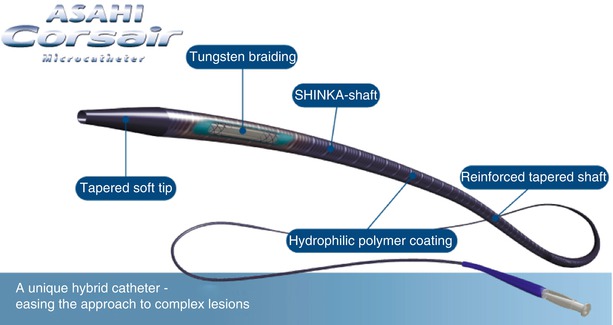
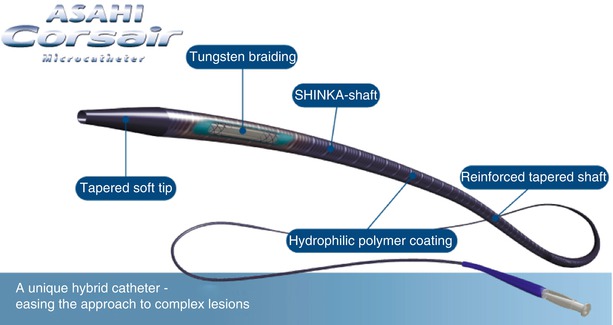
Fig. 24.4
Corsair microcatheter. The Corsair is a tungsten braided lubricious over-the-wire microcatheter that greatly facilitates retrograde collateral crossing (Courtesy of ASAHI INTECC USA, INc., Santa Ana, CA, USA)
In order to assist with collateral wire manipulation and allow for subsequent wire exchange, an OTW support catheter should be used. Many advocate a dedicated exchange catheter such as the Terumo FineCross or a 1.25 mm/1.5 mm OTW balloon catheter. Standard microcatheters have largely been supplanted by the Corsair catheter, which is an OTW hybrid support catheter and channel dilator specifically designed for retrograde PCI. It consists of an array of eight thin wires wound together with two larger wires in a spiral structure allowing torque to be transmitted from shaft to tip, and advancement is facilitated by rotation similar to the Tornus catheter. It has a hydrophilic polymer coating on the distal 60 cm to facilitate channel crossing. In a recent study, procedural retrograde CTO PCI success in cases in which the retrograde channel was successfully crossed with a guidewire was 99 % with the Corsair versus 92.5 % with standard techniques (p = 0.030). There was also a strong trend toward lower fluoroscopy and procedural time [15




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree