7 | The Role of Doppler Ultrasound in the Diagnosis of Ectopic Pregnancy |
In the prospective, risk-oriented care of early pregnancy it is axiomatic to think of an ectopic implantation (think ectopic) until an intact intrauterine gestation has been demonstrated. Hence exclusion of an abnormal early gestation becomes the essential diagnostic goal of the first 10 weeks of pregnancy, i. e., before 3-point screenings can be instituted.
The early detection of an ectopic pregnancy has been advanced by three basic recent developments:
1. The development of highly sensitive rapid determinations of human chorionic gonadotropin (β-hCG),
2. Improved resolution by transvaginal sonography,
3. The capability of using transvaginal color Doppler sonography to examine extrauterine structures suspected of containing chorionic material.
The Significance of Transvaginal Sonography and Serum hCG
A number of studies agree that an ectopic pregnancy can be detected by transvaginal sonography in 80–95% of cases. In these cases β-hCG levels were 6500 mIU/mL or above. These findings lead to the conclusion that in asymptomatic patients, when the serum β-hCG level exceeds 6500 mIU/mL with no evidence of intrauterine gestational material an ectopic pregnancy must be suspected. Further diagnostic studies must be performed to confirm or exclude the diagnosis.
All patients should have transvaginal ultrasonography performed routinely in early pregnancy. Early diagnosis clearly reduces maternal risk by diagnosing ectopic pregnancy early and provides a better chance to use laparoscopic intervention and avoid organ damage. Such a precaution is particularly mandatory in patients with a diagnosis of sterility or chronic relapsing inflammation, patients fitted with intraunterine devices (IUDs), and of course women with a prior ectopic pregnancy.
Characteristic Sonographic Findings in Ectopic Pregnancy
Currently, in the presence of a positive pregnancy test, the following transvaginal sonographic findings are considered to be diagnostic or at least strongly suspicious of an early ectopic pregnancy:
1. Exclusion of an intrauterine gestational structure,
2. An extrauterine structure suggesting a gestational sac,
3. The sac shows signs of cardiac activity and movement (frequency <5%),
4. The uterus is enlarged and the endometrium is thickened and hyperechoic,
5. There is free fluid with clotting and fibrin strands in the space of Douglas and in the pericolic recesses (hemoperitoneum).
As the number of these coincidental or associated factors increases, it becomes more likely that the suspected diagnosis is correct.
Differential Diagnosis
Differentiating an ectopic pregnancy that is not intact from an adnexal tumor is difficult, since the amniotic cavity cannot always be clearly delineated from a partly cystic, partly solid tumor. In such cases diagnosis must be based on clinical symptoms and serial β-hCG readings.
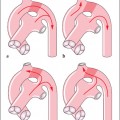
A pseudogestational sac seen on abdominal sonography, hence previously considered characteristic of ectopic pregnancy, may no longer appear on vaginal sonography because of its improved resolution. If a ring structure is seen in the uterine cavity by the vaginal route, the differential diagnosis rests between a threatened and an incomplete abortion, especially if accompanied by bleeding.
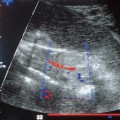
Without doubt the use of improved ultrasound methods increases the success of preoperative diagnosis. The most recent advance is the use of color Doppler ultrasound, in an attempt to attain better differentiation of possible extrauterine gestational structures by their increased vascularization and their characteristic peritrophoblastic blood flow patterns.
Nevertheless, in clinical settings ectopic pregnancy continues to pose daily diagnostic and therapeutic challenges, both in asymptomatic and symptomatic cases.
Transvaginal Color Doppler Ultrasound
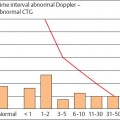
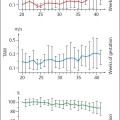
As transvaginal color Doppler sonography spread, publications began to appear in 1990 defining the characteristics of blood circulation during early placentation. The typical Doppler signal from the peritrophoblastic region is characterized by a high systolic flow velocity and low impedance, i. e., a high diastolic flow velocity. This leads to the conclusion that there is a high pressure gradient between the maternal arteries and a perfusion space with low pressure, the intervillous space. Physiologically, the histomorphological correlate to this physiological event can be found in the maternal vessels at the site of placental implantation.
In ectopic implantation corresponding phenomena of early placentation can be demonstrated until they are outweighed by the limitations posed by the abnormal nidation site. These induce regressive changes that terminate the perfusion, unless an acute event such as abdominal pain caused by the rupture of the fallopian tube emerges first.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree