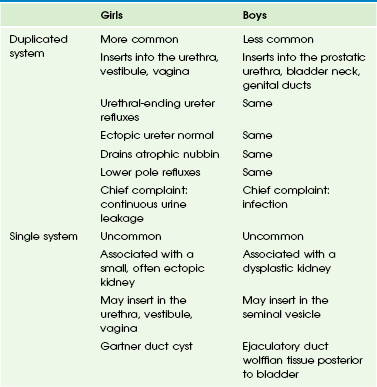
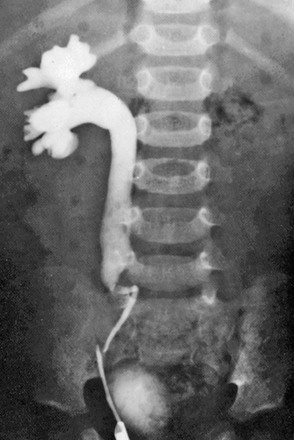
Chapter 119 The ureter develops from a branch of the mesonephric duct called the ureteric bud. It arises during the fourth to fifth week of pregnancy and grows dorsally and upward until it contacts the nephrogenic cord. This contact of the ureteric bud with the metanephric blastema induces normal kidney development. The ureterovesical junction (UVJ) develops as the distal parts of the mesonephric duct are incorporated into the enlarging bladder originating from the urogenital sinus. As the mesonephric ducts are absorbed, the ureters come to open separately into the urinary bladder, with the orifice moving superolaterally and the distal ureteral segments entering obliquely through the base of the bladder. During this complex course of development, numerous variations concerning the position of the kidney, the course of the ureter, and the anatomy of the UVJ, as well as the ureteropelvic junction (UPJ), may arise.1–11 Imaging: On ultrasonography, the ureter can only be visualized when it is sufficiently filled with urine. The UPJ usually can be sonographically visualized in well-hydrated patients with a tapering of the pelvis toward the proximal ureter, using the kidney as an acoustic window from a dorsal or lateral approach. For visualizing the distal ureter, a sufficiently distended urinary bladder is mandatory, because it serves as a window to the retrovesical space. With sufficient bladder filling, the normal ureter can be detected and followed superiorly for several centimeters. Further visualization up to the iliac vessels or higher is only possible in cases with a significantly dilated ureter and sufficient sonographic access.1 The patency of the ureteral orifice can be sonographically assessed by observing the urine inflow jet into the urinary bladder. This ureteral jet sometimes can be seen on gray scale as a rush of pseudoechoes from the ureteral ostium into the bladder lumen, but it is more easily seen with color Doppler ultrasonography. Color Doppler imaging allows not only visualization of ureteral patency and osteal position but also evaluation of the frequency of the inflow jet, indicating ureteric peristaltic activity. Thus asymmetric jets, atypical direction of the ureteral jet, lateralized orifice position, and unusual ostial shape and impaired ureteral peristalsis may be used as indirect signs for ureteral pathology or dysfunction such as obstruction or vesicoureteral reflux (VUR).1,12–14 Modern multislice computed tomography (CT) is a powerful imaging tool that provides high spatial and anatomic resolution, but it may impose a significant radiation burden even using low-dose pediatric protocols. Thus in pediatric uroradiology, CT should be restricted to uncommon and complicated cases. Contrast-enhanced CT allows for excellent delineation of the entire ureter. By using three-dimensional reformatting and viewing techniques, an intravenous urography–like comprehensive overview over the entire ureter can be achieved. This technique usually is applied in rare or difficult cases, such as for assessment of a retrocaval ureter, ureteral tumors, and paraureteral pathology compressing or displacing the ureter.1,15–17 Magnetic resonance urography (MRU) is a powerful new tool for imaging the ureter and urinary tract. By applying heavily T2-weighted sequences, a sufficiently distended or dilated ureter can be visualized in its entire course without administration of a contrast agent. However, diuretic stimulation before the investigation is helpful and even mandatory in many cases. Diuretic contrast-enhanced MRU additionally allows for functional assessment by using fast T1-weighted sequences (usually three-dimensional gradient-echo or turbo-flash). The spatial resolution of MRU is less than on CT, and thus small folds or tiny stones can be overlooked or only inferred from indirect signs. In the lower parts of the ureter, where motion from breathing is less likely, high-resolution magnetic resonance (MR) sequences can improve spatial resolution for depiction of small structures, such as an unusual course or insertion site of an ectopic ureter.1,18–22 The current best method for assessment of ureteral function and drainage is dynamic nuclear scintigraphy. Serial image acquisitions are obtained after intravenous injection of technetium-99m–labeled mercaptoacetyltriglycine and diuretic stimulation. Ureteral drainage can be visualized and quantified in a standardized fashion. However, the normal ureter usually is difficult to assess by this method and, despite its excellent functional information, anatomic resolution is poor.1,23–25 Overview: Obstruction may be severe, threatening renal function and urine drainage, or it may be partial and minor without any clinical consequence. Most ureteral obstructions occur at the UPJ or UVJ. Obstructive lesions between these two points are uncommon and include retrocaval ureter, retroiliac ureter, ureteral obstruction caused by other vessels, ureteral valves, acquired ureteral strictures, ureteral urolithiasis, ureteral neoplasms, and extrinsic lesions affecting the ureter.1 Overview: Ureteral valves are said to consist of a cusplike fold or an iris diaphragm composed of ureteral mucosa and smooth muscle fibers (Fig. 119-1). They are more commonly found in the lower third of the ureter. In neonates and infants, ureteral valves may be difficult to differentiate from physiologic ureteral folds, which are immature remnants that disappear during the first years of life. Ureteral striations are longitudinal mucosal folds that may be seen in normal ureters but often are a sign of inflammatory disease, VUR, or previous obstruction. They must be distinguished from submucosal hemorrhage and collateral circulation resulting from renal vein or inferior vena cava thrombosis.1,26–32 Overview: A retrocaval or circumcaval ureter (Fig. 119-2) is an uncommon anomaly in which the right ureter passes behind the inferior vena cava, emerges between the cava and the aorta, and then curves around and in front of the cava to return to its normal position in the pelvis. This anomaly results from abnormal persistence of the subcardinal vein in the definitive inferior vena cava. The ureter descends from the renal pelvis and crosses behind the inferior vena cava near its bifurcation. It then curves medially and upward, forming a reversed-J appearance (Fig. 119-3). Ureteral obstruction at this level is common. The retrocaval ureter is more common in males than in females and usually manifests in adult life, perhaps because the hydronephrosis is slow to develop. The anomaly may be demonstrated with contrast-enhanced multidetector CT, but MRU (with or without contrast) provides a less invasive and nonionizing imaging option.1,33–35 Ureteral obstructions caused by accessory renal arteries, iliac vessels, ovarian arteries, and hypogastric arteries (e-Fig. 119-4) are rare. Normal vascular impressions occasionally are seen on imaging (e-Fig. 119-5).36–37 Figure 119-2 Abnormal ureteral course. Figure 119-3 Retrocaval ureter. e-Figure 119-4 Ureteral obstruction from a crossing vessel. Overview: An ectopic ureter is one that drains in an abnormal location (outside the posterolateral angle of the trigone) either within the bladder or extravesically. Extravesical ureteral ectopia is more common and clinically more important than the intravesical type. It also is more common in girls than in boys, with some anatomic and functional differences between the two sexes (Table 119-1). It is more common in ureteral duplication anomalies (up to 80%).1,11,38–41 Intravesical Ureteral Ectopia: Two types of intravesical ureteral ectopia are recognized: lateral and caudal. In lateral ectopia, the more common of the two, one or both ureters (the lower pole ureter in a duplicated system) drain into the bladder more superior and laterally than normal. The intramural submucosal tunnel of the affected ureter tends to be short or otherwise defective, leading to VUR in many cases. In the second type, one or both ureters (the upper pole ureter in a duplicated system) drain inferior and medial to the usual site along a line extending from the normal lateral corner of the trigone to the bladder neck. These ureters are less prone to VUR than the lateral type.1,38,41 Extravesical Ureteral Ectopia: Extravesical ureteral ectopia in girls (Fig. 119-6) is associated with a duplicated system in at least 85% of cases and affects the upper pole ureter in practically all cases. The ectopic ureter may end in the urethra or in the vestibule or, less commonly, in the vagina (Fig. 119-7). A common presenting complaint is continuous leakage of urine in the context of an otherwise normal voiding pattern. Leakage of urine is observed even if the anomalous ureter ends in the proximal urethra, as a result of the relative weakness of the external urethral sphincter in girls. The renal parenchyma drained by the ectopic ureter often is dysplastic with decreased or absent function. The ipsilateral lower pole ureter may be normal or dilated and frequently is the site of reflux.1,42–46 Figure 119-6 Types of ureteral ectopia in females. Figure 119-7 Ureteral ectopia. Single (unduplicated) ureteral ectopia in girls is uncommon and usually unilateral. The corresponding kidney frequently is small and dysplastic and may be ectopic. Sometimes the ectopic ureter is connected with a multicystic dysplastic kidney or ends blindly superiorly without renal tissue (renal agenesis). The anomalous ureter may terminate in the urethra, vestibule, or vagina. Occasionally, a single ectopic ureter ends in a blind cystic structure in the lateral wall of the vagina (a Gartner duct cyst) (Fig. 119-8). Developmental anomalies of the vagina, uterus, and ipsilateral ovary may be encountered.1,42–46 Figure 119-8 Ureteral ectopia into Gartner duct cyst. Extravesical ureteral ectopia in boys occurs much less commonly than in girls. The anomaly commonly involves the upper pole ureter in a duplex system but also may occur in a single, unduplicated ureter. The anomalous ureter may insert in the prostatic urethra, sometimes near the bladder neck, and much less often in the genital ducts (seminal vesicle, vas deferens, or ejaculatory duct) (Fig. 119-9). Ureteral ectopia to the posterior urethra usually ends slightly above or at the level of the verumontanum (Fig. 119-10). Ureteral ectopia to the genital ducts ends in a markedly dilated, cystic mass behind the trigone of the bladder. The renal parenchyma drained by the ectopic ureter is commonly small and dysplastic and often nonfunctioning. Urinary incontinence rarely is a problem in boys because the ectopic ureter drains above the strongly developed external urethral sphincter. Cryptorchidism or testicular hypoplasia on the side of the lesion is common.1,11,38,47–49 Figure 119-9 Types of ureteral ectopia in males. Figure 119-10 Ureteral ectopia into the urethra. Imaging: Ultrasound is the initial imaging method of choice and often is diagnostic, particularly when the anomalous ureter is dilated and sufficient renal parenchyma or even cysts of the corresponding renal moiety are present. The course of this ureter often may be followed down to and beyond the bladder. A vaginal ectopic ureter may be shown by ultrasound to be connected with a urine-filled vagina (e-Fig. 119-11). A nonfunctioning system is best visualized by MRU (Fig. 119-12). When the aberrant ureter empties in the urethra, VUR into the ectopic ureter occasionally is demonstrated by voiding cystourethrogram (VCUG) (Fig. 119-13 and e-Fig. 119-14). A vaginogram or genitogram may show reflux in the affected ureter if it terminates in the vagina (see Fig. 119-7). Note that many of these anomalies are accompanied by ipsilateral malformations of the genitalia. A thorough investigation of the vagina, the uterus, and the ovaries by ultrasound or magnetic resonance imaging (MRI) is recommended.1,11,18,20–22,38,39,50–52 Figure 119-12 Ectopic ureteral insertion. Figure 119-13 A voiding cystourethrogram image series in a girl with a refluxing ectopic ureterocele inserting into the urethra and filling of a diverticula-shaped ureterocele connected to the posterior urethra during voiding (see e-Fig. 119-14). e-Figure 119-11 Ectopic ureteral insertion. e-Figure 119-14 Ultrasound and voiding cystourethrogram (VCUG) in two patients with an ectopic ureter inserting into the urethra.
The Ureter
Embryology
Obstruction of the Ureter
Ureteral Valves and Striations
Vascular Obstruction
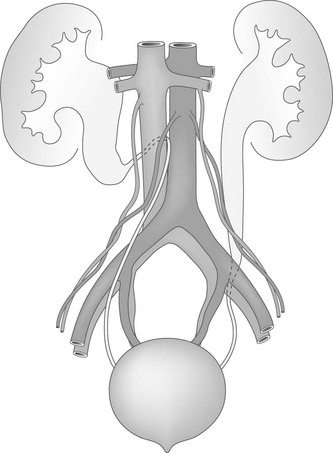
An anatomic diagram shows a right retrocaval ureter and a left retroiliac ureter.

Intravenous urography image shows right hydronephrosis. The dilated right ureter passes behind the inferior vena cava in front of the L3 pedicle.
A retrograde study in a child with partial ureteral obstruction as a result of an overlying hypogastric artery.
Ureteral Ectopia: Intravesical Versus Extravesical
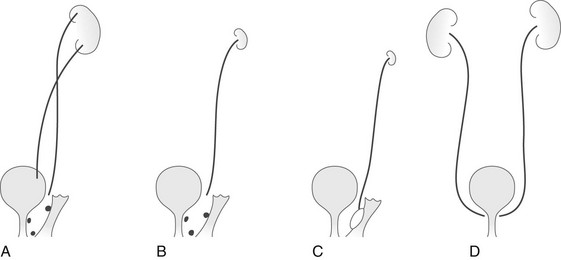
A, In the most common variant, ureteral duplication is present, with the upper pole ureter draining into the urethra, into the perineum near the urethral meatus, or into the vagina. B, Ectopic ureteral drainage as in A, but from a single collecting system. The kidney may be small and dysplastic. C, Ectopic drainage from a single system into a Gartner duct cyst in the wall of the vagina. The ipsilateral kidney may not be identifiable. D, Bilateral single-system ectopic drainage into the bladder neck or proximal urethra. This uncommon form is found almost exclusively in females and usually is associated with a wide bladder neck, a defective internal sphincter, sometimes a malformed urethra, and urinary incontinence.
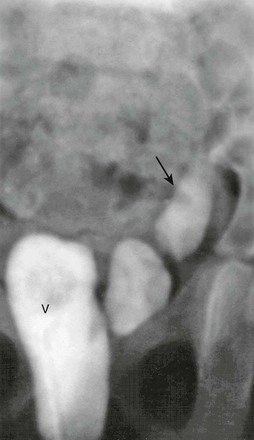
Contrast medium injected into the vagina (V) is seen filling the distal left ureter (arrow).
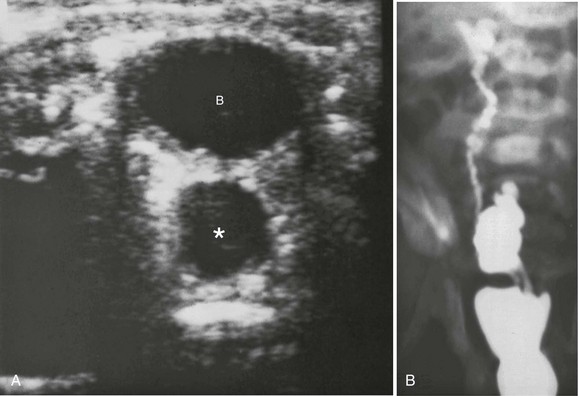
A, A transverse sonogram shows a cystic structure (asterisk) posterior to the bladder (B). B, A voiding cystourethrogram image shows filling of the bladder, through the Gartner duct cyst, and through the ureter to the upper pole.
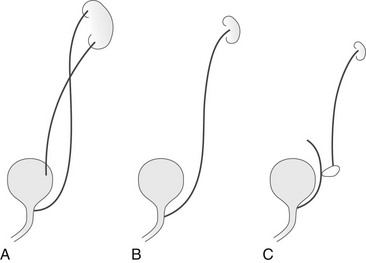
A, In the most common variant, ureteral duplication is present with the upper pole ureter draining into the posterior urethra. B, Ectopic ureteral drainage as in A but from a single collecting system. The kidney may be small and dysplastic. C, Ectopic drainage from a single system into a seminal vesicle, vas deferens, or ejaculatory duct. The ipsilateral kidney may not be identifiable.
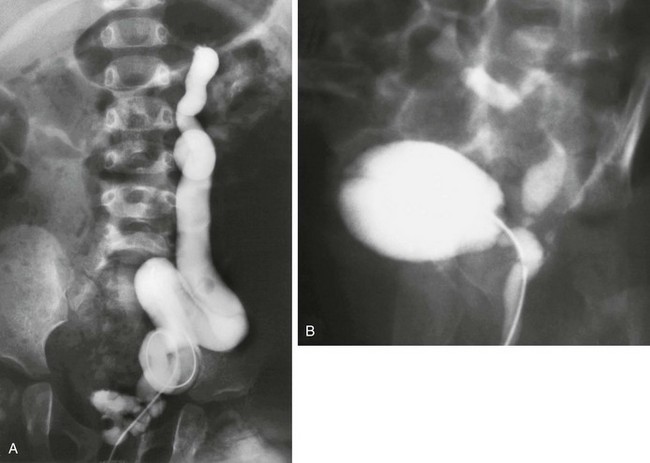
A, A voiding cystourethrogram image shows that the catheter has passed from the urethra directly into the ureter, which drains an atrophic upper pole. B, A voiding cystourethrogram image during voiding shows vesicoureteral reflux into the ureter, which drains into the posterior urethra.
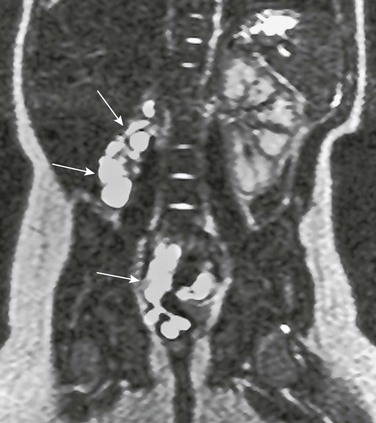
Magnetic resonance urography demonstrating a cystic remnant of an ectopic renal bud (top arrows) with only minimal residual function and a dilated and tortuous dysplastic ureter (bottom arrow) ectopically inserting into the vagina.

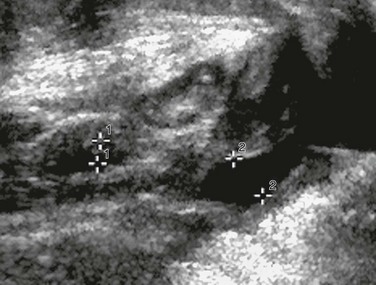
A longitudinal sonogram demonstrates a urine-filled vagina (cursors labeled “2”) with a nearly empty bladder (cursors labeled “1”) in a girl with ectopic vaginal ureteral insertion.
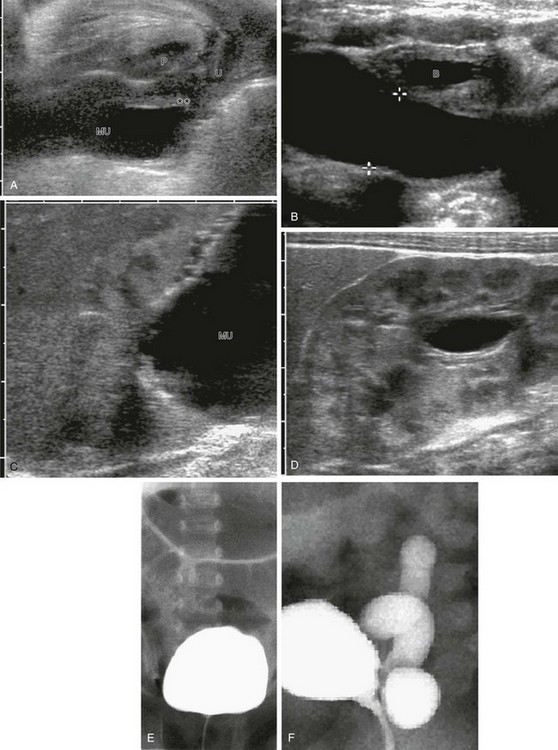
A, Perineal ultrasound of the urethra and the distal megaureter (MU) inserting ectopically (asterisks). U, Urethra; P, pubis. B, Megaureter (cursors) behind the urinary bladder (B). C, A longitudinal sonogram shows the upper dysplastic moiety of the kidney draining into the megaureter (MU). D, A longitudinal sonogram shows some dilatation of the lower moiety of the duplex kidney as a result of compression of the ureteropelvic junction by the upper pole megaureter. E and F, A VCUG image series in a girl with a refluxing ectopic ureterocele inserting into the urethra: no vesicoureteral reflux during filling (E) and with consecutive slow vesicoureteral reflux into the fluid-filled corresponding megaureter (F).
Get Clinical Tree app for offline access