P-32
Y-90
Re-86
Er-169
Radiation
B
B
B and G
B and G
Particle size (u)
6–20
10–20
0.1
1000–2000 nm
Penetration (mm)
3–5
4–10
1–4
0.1–0.4
Half-life (days)
14
2–4
3.8
9.4 days
Safety concerns with this method gear toward growth plate disturbance as the subjects are mostly children. Articular cartilage is highly resistant to radiation and although damage is theoretically possible, none has been reported.
The other concern is the late effects of neoplasia from the radiation. Because of the low dose penetration of P-32 bone exposure is minimal. In the follow-up of more than 5000 radiation synovectomies done for rheumatoid arthritis, none developed malignancies. (Lee 1982) Chromosomal changes have been reported in a small proportion but which disappear by the end of the first year post-procedure, besides no pre-malignant chromosomal structure has been described. (Nilsson et al. 1992).
The approved radionuclides for therapy in Europe (Clunie and Fischer 2003) are (Yttrium–90, Rhenium-186, and Erbium-169). In Canada and the US, P-32 is being used. These radionuclides are thought to be rapidly phagocytised by synoviocytes and then distributed within the surface of the synovium causing vasculitis, which occludes the microvascular supply. This, in addition to the cytotoxic effect of radiation, results in ablation of the synovium. (Rodriguez-Merchan and Wiedel 2001).
The ideal radionuclide should meet the following requirements: it should be attached to a particle that is sufficiently small to be phagocytized but not too small that it might leak from the joint before being phagocytized (2–10 um); binding between the radionuclide and particle should be stable throughout the course of RSV, which in turn is determined by the half life of the radionuclide; and radiolabeled particles should be distributed homogenously in the intraarticular space without initiating inflammatory response. (Arnold and Hilgartner 1977).
These requirements are met by Y-90 colloid, making it suitable for the knee joint, while Re-186 on the other hand, is more appropriate for medium-sized joints such as the hip, the shoulder, the elbow, the wrist, the ankle, and the subtalar. Lastly, for the smaller joints, Er-169 is used.
The activity administered and the volume is dependent on the type of joint to be injected. The recommended doses are seen in Table 2. As mentioned, Y–90 colloids are only suitable for the knee joints. The recommended dose for it would therefore be 185–222 MBq (5–6 mCi). Doses to be delivered to the synovium have been estimated from models of joints using a series of assumptions. (Johnson and Yanch 1991) Generally, doses are dependent on the radionuclide used, size of joint cavity, synovial thickness, distribution of the colloids in the joint fluid, and inflammatory activity of the joints.
Table 2
Recommended isotope, dose and volume
Joint | Adm activity Mbq (mCi) | Recommended volume |
|---|---|---|
Knees | Y-90-185-232 | 5 ml |
Hip | Re-186-74-185 (2-5) | 3 ml |
Shoulder | Re-186-74-185 (2-5) | 3 ml |
Elbow | Re-186-74-111 (2) | 1–2 ml |
Wrist | Re-186-37-74 (1-2) | 1–1.5 ml |
Ankle | Re-186-74 (2) | 1–1.5 ml |
Subtalar | Er-169-37-74 (1-2) | 1.5–2 ml |
3.2 Indications
Radiosynovectomy has common indications as rheumatoid arthritis, hemophilic arthritis, and other forms of arthritis. (Schneider et al. 2005) Absolute contraindications include pregnancy, breastfeeding, local skin infection, and ruptured popliteal cyst (knee). Relative contraindications are when the potential risks outweigh benefits, presence of inhibitor, extensive joint instability with bone destruction, and evidence of significant cartilage loss within the joint.
3.3 Side Effects
Side effects (Fettich 2005) are rare if the RSV is done properly. Side effects are dependent on the radionuclide used, activity administered, and technique of administration. Infection is rare because of the high concentration of the radioactive material in the joint killing all the bacteria. Fever, initial flare, and local pain may occur and oral analgesics may help. Necrosis from extravasation to soft tissues may also occur. Leakage of the radionuclide from the joint via the lymph node may also happen so the need for post-RSV scintigraphy. Immobilization for at least 48 h is advised to decrease chances of leakage. Late side effects have not been reported.
3.4 Procedure
There are several conditions that have to be met before RSV treatment can be carried out. First of all, the procedure must be done in an approved facility with appropriately shielded and sterile rooms that are manned by trained medical staff. The hemophilic patient must also have at least a history of three successive bleeds in the past six months. (Siegel et al. 2004).
3.4.1 Ancillary Tests Prior to RSV
Radiographs of the joints to be treated (Fig. 1) should be obtained and reviewed before the procedure. (Arnold and Hilgartner 1977) Candidates with good prognosis should be at least Stage II according to the classification of Arnold and Hilgartner. Bone scintigraphy (Fig. 2a, b, 3a, b) is ideally done as it is useful especially the blood pool or soft tissue images, not only for assessing the suitable joints, but in monitoring the severity of active bleeding or inflammation as well. It could also aid the clinician in noting any improvements during follow-ups post-RSV. Ultrasound may evaluate joint space, synovial structure and thickness, extent of effusion, and exclude Baker’s cyst. Magnetic resonance imaging of the affected joint may help but is not necessary.
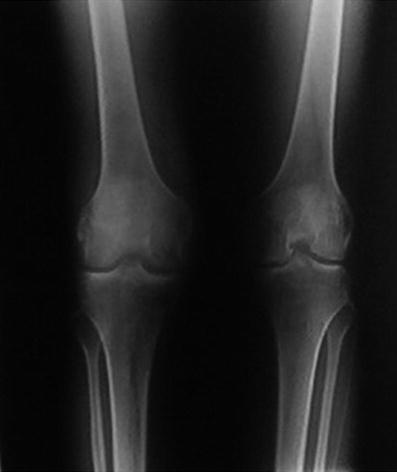
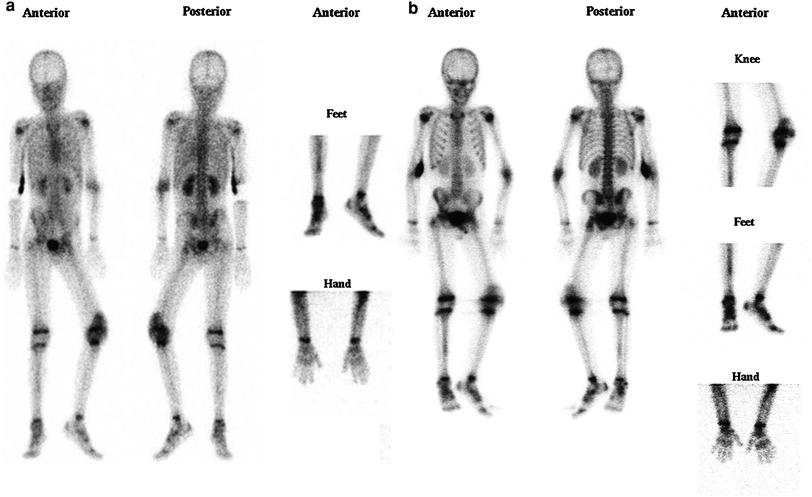
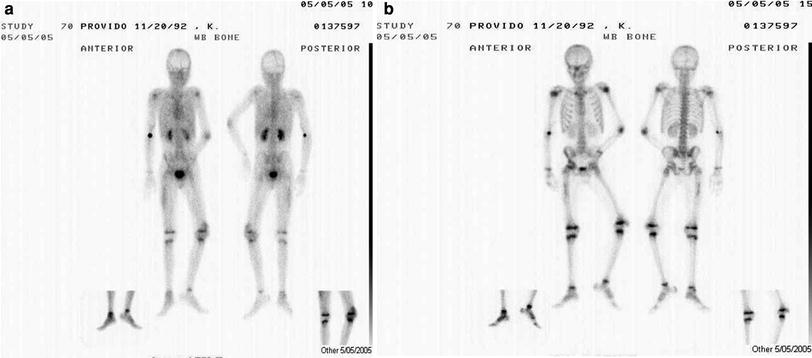
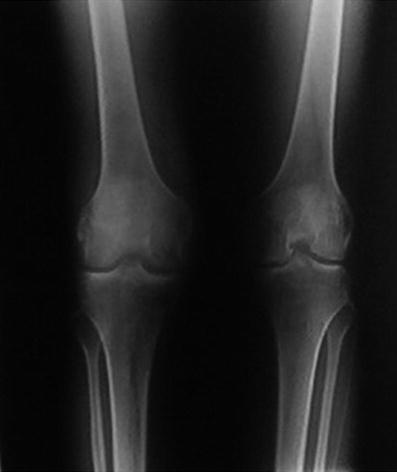
Fig. 1
Baseline radiographs of the knees
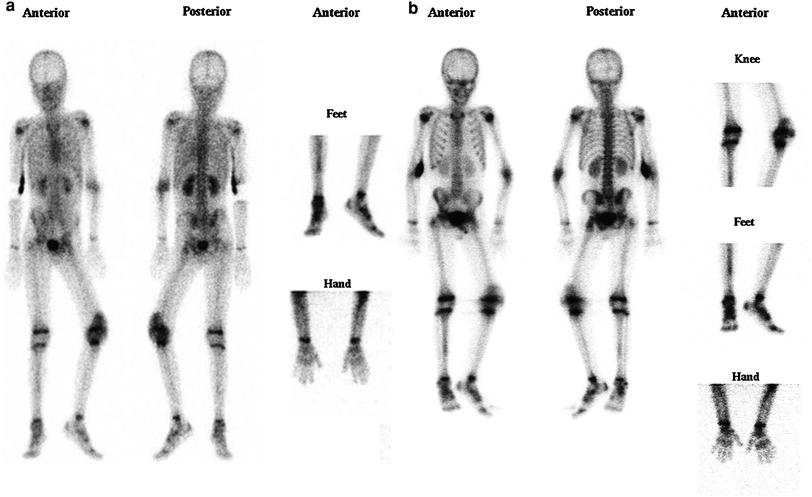
Fig. 2
a Pre-therapy scans of a hemophilic patient in the tissue phase b Pre-therapy scans of a hemophilic patient in the skeletal phase
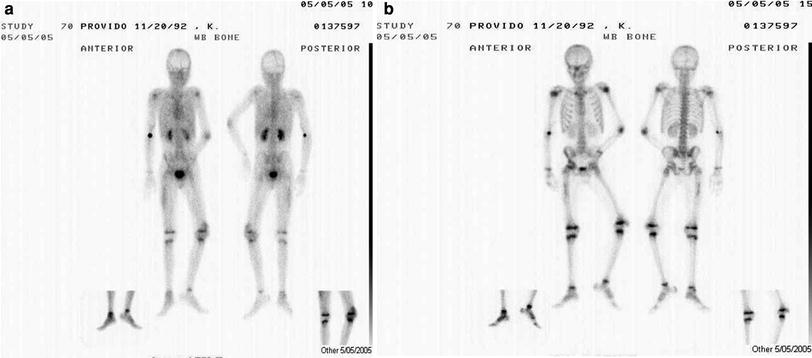
Fig. 3
a Post-therapy of same hemophilic boy one year after (tissue phase) showing tremendous improvement of the left knee, which was subjected to radiosynovectomy b Post-therapy of same hemophilic boy one year after (skeletal phase) showing tremendous improvement of the left knee which was subjected to radiosynovectomy
The time interval between arthroscopy and joint surgery should be 2–6 weeks and there should be a minimum interval of 6 months between repeated treatments in the same joint.
Patients should have both written and verbal instructions. It is important to tell them that they need to immobilize the affected joint for 48–72 h post-injection. They should know that there may be an initial flare/synovitis and that the success rate is 60–90 %. They should also be told that response is around 14 days and that the benefit is limited to the injected joint. They should know the potential risks that go with the joint puncture, such as hemorrhage, infection, discoloration, and extravasations as well as theoretical risks for radiation necrosis (rare) and future malignancy.
3.4.2 Administration
The hemophilic patient must be given Factor VIII or IX before the procedure and must have at least 30 % coagulopathy before the procedure.
After positioning the patient, the area around the joint to be treated should be cleansed adequately. After strict asepsis, local skin anesthesia (Xylocaine) is advised. Correct deposition to the joint is essential and may be done by fluoroscopy, or ultrasound guided, or when one is able to aspirate synovial fluid and blood from the affected joint.
The needle through which the radiopharmaceutical has been injected should be flushed with NSS before withdrawal to avoid tissue extravasations. Absolute immobilization of the treated joint for 48–72 h using splints or bed rest reduces leakage of particles to the regional lymph nodes. Ice packs may help immediately after the procedure for clotting. Bremsstrahlung imaging of the injected joint (Fig. 4) to determine if there is homogeneous deposition of the radionuclide as well as for leakage.
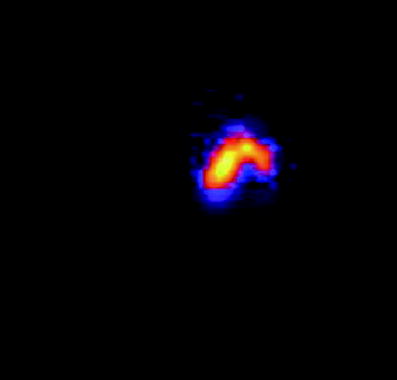
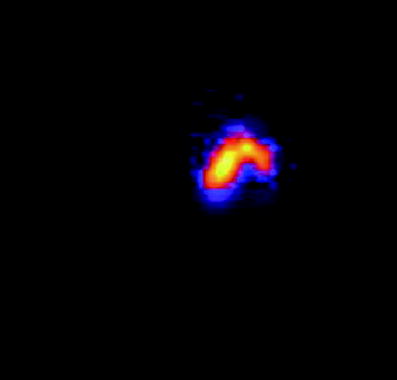
Fig. 4
Image (Brehmstrallung) to ensure Y-90 is deposited to the injected knee
Other instructions include that patients should avoid pregnancy for at least 4 months, urinary excretion for the first two days should be flushed two times and that good hygiene is a must to avoid contamination.
Follow-up should be done after a month, 3–6 months or when a problem occurs. Bone scans and radiographs may be needed to assess improvement and function.
Success of treatment as accepted by the World Federation of Hemophilia (WFH) comprises of four parameters: pain, bleeding, physical examination, and radiographic examination. They developed a clinical and radiologic scale to quantify improvement considering hemarthrosis, articular pain, range of motion (ROM) in flexion, ROM in extension, muscle strength (MS) in flexion, MS in extension, the degree of synovitis detected on clinical examination, the size of the synovium as measured by means of imaging techniques (in millimeters). Most studies consider the number of episodes of hemarthrosis and the severity of pain as the variables associated with the greatest improvement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







