20 Thermal Ablation of Renal Lesion
Wael E.A. Saad and Daniel B. Brown
This book deals with ultrasound-guided procedures. The majority of institutions/operators utilize computed tomography (CT-) guidance, not ultrasound guidance, for renal ablation. This is for several reasons.
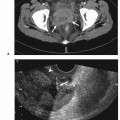
- Although ultrasound guidance provides real-time imaging and can be helpful during needle placement, its advantage is lost once radiofrequency ablation (RFA)/cryoablation begins due to the increased echogenicity/visualization of the lead edge of the ice-ball during cryoablation.
- Not all lesions can be visualized easily with ultrasound to the extent that an operator may not be comfortable that he or she is in a good position for a complete ablation. This is particularly true in patients with large body habitus. Almost all masses can be seen, assessed, and treated with CT guidance. For the sake of streamlining the process and not tailoring guidance requirements to each lesion/patient, many institutions adopt “get-them-all” guidance.
- CT provides a global image of the surrounding structures (“a lay of the land”) and accurately assesses distances between the probe and adjacent structures, particularly the colon. It is easier to assess colon distance (with reproducibility) by CT particularly for lesions that are at a higher risk for being closer to the colon – lower pole and posterior lesions.
- For the reason noted above, CT rather than with ultrasound is more accurate (with reproducibility) in assessing bowel displacement techniques because it helps the operator to maintain a safe distance between bowel and the ablative probe before and after displacement.
The increasing use of cross-sectional imaging over the past two decades has led to the discovery of more incidental early-stage renal tumors. In addition, the trend for managing early stage – less than 3-to 4-cm diameter – renal masses has been away from nephrectomy and toward nephron-sparing surgeries. Percutaneous thermal ablation of renal tumors with its reduced morbidity is a further step in the progression of this trend.
The rising “incidence,” or rather, discovery of renal masses and the minimally invasive treatment trend drive percutaneous ablation of renal tumors. However, the lack of randomized control trials and/or long-term follow-up data (especially when we are dealing with renal cell carcinoma [RCC] with tumor size <3–4 cm, which usually has a long-term survival rate without patient treatment) make it difficult to clearly define indications for image-guided renal mass ablation. Therefore, this chapter will discuss patient candidates/lesion selection rather than indications. Patient selection should be multidisciplinary.
- Small (<3–4 cm) solid renal cell mass confined to the kidney
- Renal arteriovenous malformation (AVM) with gross hematuria that is inaccessible by endoluminal means
A lot of device selection is going to come down to operator preference.
- Radiofrequency ablation
- Small solid lesions
- Exophytic lesions
- Cryoablation (heat-sump problems for RFA)
- Central lesions closer to collecting system (pelvicalyceal system)
- Cystic lesions
- Solid lesions adjacent to cysts
- Cryoablation is less painful and may be more appropriate for patients undergoing ablation under sedation only (no general anesthesia).
- Patients with high medical comorbidities (nonsurgical candidates)
- Very elderly patients with small (<3 cm) RCC (life expectancy)
- Patients who refuse surgery
- Patients requiring the highest nephron-sparing procedure available
- Multifocal RCC whether
- RCC in solitary native kidneys
- RCC in transplanted kidney
- Borderline poor renal function (on the brink of dialysis)
- See the introduction to this chapter
- Lesions seen by ultrasound – especially lesions that are intraparenchymal and are appreciated by ultrasound (differentiated from surrounding normal parenchyma) and not by unenhanced CT
- Lesions found by preprocedural cross-sectional imaging that are clearly at a distance (>2 cm) from the colon
- Uncorrected coagulopathy
- Suggested coagulation parameters
- International normalized ratio (INR): ≤1.4
- Platelets (PLT): ≥50,000
- Activated partial thromboplastin time (aPTT): ≤65 seconds
- Renal ablation should be performed electively unless hematuria is the cause of instability or is adding to the instability, which is not common).
- Sepsis (can be treated first, unless you are dealing with gross hematuria requiring a blood transfusion)
- Patient instability (can stabilize first, unless you are dealing with gross hematuria requiring a blood transfusion)
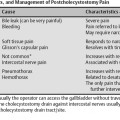
- Lesions that are anterior on the kidney that require access percutaneously via normal kidney (transrenal approach) are probably better candidates for laparoscopic ablation and not image-guided percutaneous ablation.
- Lesions that are anteromedial and adjacent to the uretero-pelvic junction (UPJ) or proximal ureter (particularly in the lower pole) have a higher risk of causing UPJ/ureteric injury such as
- Ureteric obstruction/stenosis
- Urine leaks
- Disease not confined to kidney (extrarenal dissemination)
- Distant metastasis (unless you are treating hematuria)
- Large lesion extending to surrounding structures outside Gerota’s fascia
- Vascular invasion (renal venous tumor thrombus)
- Location related: Lesions that are close to adjacent structures especially bowel in cases where bowel displacement techniques have failed
- Characterize the lesion
- Make sure that this is a legitimate lesion. Fat inside the lesion may indicate that it is an angiomyolipoma and not a malignant lesion that needs to be ablated.
- Cystic lesions may rupture, and thus change shape, characteristics, and size on deploying the ablative probe. Be prepared for that; think of using cryotherapy.
- Some institutions/operators tailor the ablative modality depending on lesion characteristics (alternate cryoablation and radiofrequency).
- Cystic and/or central lesions get cryoablation.
- Exophytic and/or solid lesions get cryoablation.
- Lesion size: Ideal lesion size is <3 cm. The smaller the better, if you can see it.
- Lesions that are anterior on the kidney that require access percutaneously via normal kidney (transrenal approach) are probably better candidates for laparoscopic cryotherapy and not image-guided percutaneous ablation.
- Small central and intraparenchymal lesions may not be appreciated by noncontrast CT.
- See if you can identify and access the lesion by ultrasound
- Carefully examine intrarenal landmarks that do not rely on intravenous (IV) contrast to attempt to identify its location to ablate the region of the lesion (“vicinity ablation”)
- Look for adjacent organs that can be inadvertently traversed or are close enough that they can be thermally injured
- Size and identify the shape of the lesion for probe sizing
- Ablation should involve the lesion in its entirety with a 5- to 10-mm normal parenchymal margin.
- Longitudinal/egg-shaped lesions should be treated with the intent of ablating at multiple overlapping stations with a probe access along the longitudinal axis of the lesion.
- Laboratory value evaluation to rule out coagulopathy. Suggested coagulopathy thresholds are
- INR: <1.4
- PLT: ≥70,000
- aPTT: ≤65 seconds
- Obtain a baseline serum creatinine value especially in nephron-sparing situations
- Indications
- Local control of malignant renal disease
- Local control of malignant liver disease can be with the intention of
- Cure
- Temporizing and local control
- Palliation (hematuria)
- Result summary for percutaneous thermal ablation of RCC
- Local tumor control (technical success): 80–100% (usually >90%)
- Technical success/local control depend on tumor location/morphology: Lesions that are more amenable to ablation are those that are exophytic – even if they are large (up to 5 cm), they can be treated successfully.
- Technical success/local control also depend on tumor size.
- <3 cm tumor: 100% success rate
- 3–5 cm tumor: 92% success rate
- <4 cm tumor
- 92% first session
- 100% by the second session
- >5 cm tumor: 25%
- Recurrence rate for RFA is 1.3–5.3% (up to 3% in partial nephrectomy).
- Recurrence rate for cryotherapy is not as clear and is probably the same. A quoted recurrence rate is 3.6%.
- Alternatives
- There is no firm evidence to establish the optimal first-line treatment of early-stage RCC because of the lack of randomized controlled trials.
- The lack of randomized control trials and/or longterm follow-up data (especially because we are dealing with RCC with a tumor size of <3–4 cm, which has a long-term survival rate without treatment) make it difficult to clearly define indications for image-guided renal mass ablation.
- To refuse the percutaneous ablation or any other therapy
- Surgery nephrectomy, partial nephrectomy
- Traditional treatment of choice
- Laparoscopic-guided thermal ablation
- Applicable to anterior lesions that can be identified and are accessible laparoscopically
- Ability to displace/remove bowel away from the target lesion
- Advantages of percutaneous thermal ablation
- Can be performed on nonsurgical candidates
- Can be performed on postoperative patients
- Is nephron-sparing
- Repeatability of treatment if initial treatments are incomplete
- Can be used with regional and systemic chemotherapy
- Minimally invasive
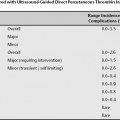
- Procedural risks
- Mortality is rare.
- Major complications occur in 0–8.3% of cases and include
- Bleeding
- Most common complication
- More common with central lesion
- Can present with
- Renal capsular hematomas
- Minor ones can be seen in up to 43% of cases.
- Larger ones can be seen in 1.9–12.5% of cases.
- Subcapsular hematomas and/or extrarenal retroperitoneal hematomas (bellow) requiring blood transfusion occur in 0.8–4.2% of cases.
- Extrarenal retroperitoneal bleeding (drop in hematocrit)
- Gross hematuria
- Infection
- Wound infection (more common)
- Retroperitoneal abscess (not common)
- It is more common with cryoablation and is reported in 1.0–4.3% of cryoablation cases.
- Pneumothorax, hemothorax requiring chest tube
- Not common
- More common with upper pole lesion
- More common with intercostal approach
- Grounding pad burns (second- or third-degree burns)
- Pelvicalyceal/ureteric injury
- Leaks
- Strictures
- Obstruction
- Early: Clotted gross hematuria (1.9%)
- Late: Ureteric stricture (0.0–8.3%)
- Focal hydrocalyx (0.0–2.5%)
- Minor complications
- Occur in 2.5–12.5% of cases
- Usually include
- Postablative syndrome (fever) seen in up to 70% of patients
- Flank pain seen in up to 10% of patients 24 hours from the procedure
- Transient hematuria not requiring a blood transfusion
- Incidental perirenal hematuria
- Paresthesia (transient)
- Minor wound infection
- Tumor seeding
- Can occur in up to 1.7–2.6% of cases
- Ultrasound machine with Doppler capability
- Multiarray 4–5 MHz ultrasound transducer
- Transducer guide bracket
- Sterile transducer cover
- Chlorhexidine skin preparation/cleansing fluid
- Fenestrated drape
- 21-gauge infiltration needle
- 10–20 mL 1% lidocaine syringe
- 11-blade incision scalpel
- Coaxial access needle
- Some thermal probes are introduced through coaxial needles.
- Coaxial needles allow coaxial biopsy needle placement followed by ablative probe placement without losing access.
- A coaxial needle may reduce the risk of tract seeding (anecdotal).
- Thermal ablative probes
The probes currently in use are summarized below.
- RFA systems
- The radiofrequency generator and the patient are the main components of an electric circuit.
- The generator is the source of the alternating current and the patient’s body is the resistor.
- The resistance in the tissue (impedance