Thoracic Aorta and Arteries of the Trunk
The thoracic aorta is conventionally divided into three segments: the ascending aorta, the aortic arch, and the descending aorta, which is subsequently divided into thoracic and abdominal segments (Fig. 7.1).
The ascending aorta arises from the left ventricle of the heart, where the aortic valve closes it. It is about 5 cm in length (Fig. 7.2). The aorta courses an anterior ascending tract to the right side of the chest, curving backward and crossing the mediastinum in the segment called the aortic arch, to the posterior mediastinum and to the left of the vertebral column (Fig. 7.3). The descending aorta approaches the median plane and terminates in front of the column, where it crosses the diaphragm at the aortic hiatus, where begins the abdominal aorta (Fig. 7.4).
Due to the need for reporting the outcomes of the modern endovascular procedures performed in the thoracic aorta—the ascending aorta, aortic arch and descending thoracic aorta were further divided into zones (Fig. 7.5). Zone 0 extends from the aortic valve to the level of the brachiocephalic trunk (including). Zone 1 extends from the edge of the brachiocephalic trunk to the left carotid artery (including). Zone 2 extends from the edge of the left carotid artery to the left subclavian artery (including). Zone 3 is the curve segment from the edge of the left subclavian artery to the beginning of the vertical descending thoracic aorta. Zone 4 includes the whole descending thoracic aorta and the segments are named T4 through T12 according to the level of the intercostal arteries. The abdominal aorta segments are named after the lumbar artery levels, from L1 to L5.
Thoracic Aorta
Aortic Vasa Vasorum
The walls of the thoracic and abdominal aorta are supplied by the vasa vasorum. The vasa vasorum system is formed by small nutrient vessels to the walls of other larger vessels. These are the vessel’s vessels, which deliver blood to a capillary network within the large arterial wall. However, only part of the vessel wall is supplied by the vasa vasorum. The part of the wall that is fed by the filtration of nutrients through the vascular endothelium is called the physiologic intima. There is a “critical deepness” of vascularization, which varies according to the different arteries and species. At the thoracic aorta, the avascular zone is of about 500 μm in thickness, whereas the avascular zone of the abdominal aorta is of about 700 μm. The tunica intima and the internal third of the tunica media receive nutrients directly from the blood within the lumen of the main artery by diffusion, whereas the external two thirds of the tunica media and the tunica adventitia are fed by arterial blood from the vasa vasorum (Figs. 7.6, 7.7).
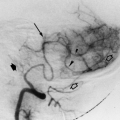
The vasa vasorum arises from the intercostal arteries at the thoracic aorta and from the lumbar arteries at the abdominal aorta. The vasa vasorum originates at the level of the tunica adventitia with a diameter of about 350 μm. The initial trunk has a ventral direction with a length of about 4 mm. Still at the tunica adventitia, the vasa vasorum trunk with a diameter of about 150 μm divides into two secondary branches of equal diameter. These branches run parallel to the main axis of the aorta in an opposite cranial and caudal direction. From these branches, a network of smaller branches is found with a lateral and ventral distribution, and with several contralateral anastomoses, forming vascular arcades on the aortic wall. The vascular disposition of the vasa vasorum follows a reticular distribution with a polygonal appearance. From the reticular vasa vasorum network originates a rich anastomotic plexus with arterioles of 1st order with a diameter of 200 μm to 100 μm. The microcirculation of the vasa vasorum is formed by the vessels less than 200 μm in diameter (Fig. 7.6).
Microcirculation of the Aorta
Arterioles of first order—between 200 μm and 100 μm
Arterioles of second order—between 100 μm and 30 μm
Precapillaries or terminal—between 30 μm and 10 μm
Capillaries—between 3 μm and 10 μm
Postcapillaries venules—between 10 μm and 30 μm
Venules of second order—between 30 μm and 100 μm
Venules of first order—between 100 μm and 200 μm
The arterioles of second order with a diameter of 100 μm and 30 μm are also called arcuate arterioles. These vessels extend for sectors of the aortic circle varying from 90° to 220°, but with an average of 120°. The precapillaries or terminal arterioles originate from the arcuate arterioles and distribute to the junction of the medium and external third of the tunica media. The distal portion of the terminal branches does not reach the internal third of the tunica media and spreads as a tree with a flat top (Figs. 7.6, 7.7).
The arterial vasa vasorum is followed by the venous vasa vasorum with inverted direction of flow. Morphologically, two venous structures correspond to the arterial structure, at the precapillaries and arcuate arterioles.
Segments of the Thoracic Aorta
An important requirement for successful endografting is to select a sufficiently long segment of healthy aorta for the landing site. This position differs from case to case, but it is necessary to make it clear where the landing zone is located if data reported from various institutions are to be accurately evaluated. Balm et al. proposed distinguishing the location of an endograft deployed in the aortic arch based on lines drawn distally to each arterial branch from the arch. Although this classification tells us which branch artery is occluded by the endograft, it does not help identify the extent of the area covered by the endograft. To arrive at a more clinically useful system an anatomic endograft landing zone map was advocated at the First International Summit on Thoracic Aortic Endografting held in Tokyo in 2001. Use of this landing-zone map to classify the proximal deployment site of an endograft would make it possible for investigators at different institutions to evaluate indications for treatment and analyze follow-up results. In 2002, this landing-zone map was expanded to include the position of the distal end of the endograft. Since then, the map (Fig. 7.5) has achieved consensus as the standardized anatomic definition to evaluate outcomes.
Ascending Aorta
At the origin of the ascending aorta, just after the cusps of the aortic valve, there are three dilations called aortic sinuses. The coronary arteries orifices are located high up in the aortic sinuses or even above them (Figs. 7.2, 7.8, 7.9, 7.10, 7.11).
Branches
Coronary arteries are described in Chapter 13.
Aortic Arch (Fig. 7.12)
There are three main branches at the aortic arch.
Branches
Brachiocephalic trunk (innominate artery) and right common carotid artery
Left common carotid artery
Left subclavian artery
The aortic arch, with age and the presence of longstanding arterial hypertension, tends to become elongated and tortuous, and the origin of the brachiocephalic vessels tends to move forward and the angle between the branches and the aortic arch becomes more acute, making selective catheterization much more difficult. The aortic arch is classified into three different types: type I, type II and type III, according to the angle between the branches and the aortic arch. One way to determine the arch’s type is to measure the diameter of the brachiocephalic artery and compare that measurement to the distance from the horizontal line traced tangent to the top of the aortic arch to the origin of the brachiocephalic trunk (Fig. 7.11). One width or less of the brachiocephalic artery is type I, two widths is type II, and three widths is type III.
Variations of the Aortic Arch
Right aortic arch
Double aortic arch
Cervical aortic arch
Brachiocephalic Trunk
It is the first and largest branch of the aortic arch. This trunk arises from the superior posterior aspect of the aortic arch. It ascends posterolaterally to the right. At first positioned anterior to the trachea, it gradually moves to the right. From its bifurcation originates the two terminal branches: the right subclavian and right common carotid arteries. Occasional branches are the arteria thyroidea ima, the thymic artery, and the bronchial artery. The right vertebral artery originates from the right subclavian artery.
The right subclavian artery has been described as the arterial supply of the upper limb section. The right common carotid artery is the principal terminal branch of the brachiocephalic artery.
The principal arteries of the head and neck are the common carotid arteries. These arteries ascend in the neck up to the level of the upper border of the thyroid cartilage, where they divide into two main branches, the external and internal carotid arteries. At the division of the vessel, there is a dilation known as carotid sinus. At the bifurcation, there are terminal nerve fibers, a baroreceptor, and a chemoreceptor called carotid body. The common carotid arteries differ in length and place of origin. Whereas the right carotid artery originates from the brachiocephalic trunk, the left carotid artery arises directly from the arch of the aorta.
It is the second branch of the arch of the aorta, arising immediately behind and to the left of the brachiocephalic trunk, presenting thoracic and cervical portions. The artery courses in an upward direction, originally in front of the trachea and progressively inclining to the left side.
Left Subclavian Artery (Fig. 7.15)
It is the third branch of the arch of the aorta, arising after and behind the left common carotid artery. It is described in Chapter 15. The left vertebral artery originates from the left subclavian artery.
Variations of the Branches of Aortic Arch
There are a number of variations of the origins of the aortic arch branches. The six vessels may arise separately from the aortic arch: carotids, the subclavians, and the vertebrals, or they may arise as a single trunk, or in a number of combinations (Figs. 7.17, 7.18, 7.19, 7.20, 7.21, 7.22). The most common variation is a high origin of the innominate artery (to the left of the trachea) (Fig. 7.17), a common origin of the left carotid artery with the brachiocephalic trunk (bovine arch) (Fig. 7.16, 7.17, 7.20), an anomalous origin of the right subclavian artery distal to the left subclavian artery (Fig. 7.19, 7.20), and an origin of the left vertebral artery directly from the aorta (Fig. 7.18).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree