Chapter 25 Tumours of the thorax
Lung cancer
Diagnosis
Patients presenting with the above symptoms require a chest x-ray. A lateral view may be helpful. A computed tomography (CT) scan of the chest and upper abdomen is recommended before bronchoscopy as peripheral tumours will not be reached by bronchoscopy and, in these cases, a CT-guided biopsy is required for histological diagnosis. Magnetic resonance imaging (MRI) can be used to determine if there are direct invasion structures contraindicating surgery but is not superior to CT in the detection of mediastinal disease (Table 25.1).
Table 25.1 Assessment of patients with lung cancer
History and examination including performance status and weight loss Additional staging if considering surgery: |
Non-small cell lung cancer (NSCLC)
Staging
The NSCLC Staging system (Table 25.2) is based on the TNM (tumour, node, metastases) method of staging and divides patients into prognostic groups for treatment.
Table 25.2 The staging system of NSCLC
| T stage | Disease extent |
|---|---|
| T0 | No evidence of tumour |
| Tis | Carcinoma in situ |
| Tx | Tumour cells obtained from sputum, no site of primary found on bronchoscopy |
| T1 | Tumour <3 cm surrounded by visceral pleura or lung tissue |
| T2 | Tumour larger than 3 cm but more than 2 cm from the carina. Involves the visceral pleura or causes atelectasis or obstructive pneumonitis of less than one lung |
| T3 | Tumour less than 2 cm from the carina but not involving it. Tumour invades chest wall; diaphragm; mediastinal pleura; parietal pericardium or causes atelectasis or obstructive pneumonitis of the whole lung |
| T4 | Tumour invades heart; great vessels; trachea; oesophagus; vertebral body; pleural effusion or satellite tumour nodules within the same lobe |
| Nx | The nodal status cannot be determined |
| N0 | No regional lymph node involvement |
| N1 | Ipsilateral peribronchial and/or hilar lymphnode involvement |
| N2 | Ipsilateral mediastinal and/or subcarinal lymphnodes |
| N3 | Contralateral mediastinal or hilar lymphnodes. Supraclavicular lymphnodes |
| Mx | Distant metastases cannot be determined |
| M0 | Distant metastases absent |
| M1 | Distant metastases present |
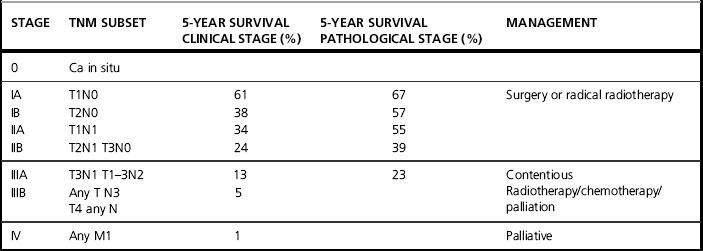
The staging and survival of NSCLC (Table 25.3) illustrates the prognostic importance of the current staging system.
The management of NSCLC
Surgery
Surgery offers the best chance of cure. Patients must be carefully selected, as incomplete excision is of no benefit. Patients must undergo extensive staging and, in practice, only those with stage I and II tumours and good cardiopulmonary function are suitable for surgery (Table 25.4).
Table 25.4 Contraindications for surgery in NSCLC
| Operable | Contraindications |
|---|---|
| FEV1 > 1.5 Stage I and II NSCLC | Poor lung function Phrenic nerve palsy (elevated diaphragm) Recurrent laryngeal nerve palsy (hoarseness) Invasion of trachea, aorta, heart, superior vena cava, oesophagus Distant metastases Metastatic SCLC Malignant pleural effusion |
Radical radiotherapy
Thoracic radiotherapy is particularly challenging as the tumour is a moving target within an area surrounded by critical and radiosensitive tissues, such as lung parenchyma and spinal cord. In addition, the characteristics of the beam are altered as the beam passes through lung tissue. Careful planning is required to take these challenges into account (Table 25.5).
Table 25.5 Indications for radical radiotherapy
| Stage 1&2 NSCLC – medically inoperable Tumour volume approximately 5 cm FEV>1; FVC>1.5 Weight loss <10% Positive margins postoperatively Heavy N2 disease postoperatively (individual patient basis) Wedge resection Stage 3 disease sufficiently downstaged to be included in a radical volume |
Technique
Patients should be CT planned, lying supine in an immobilization device. The patient is instructed to breathe normally. The normal treatment position is ‘arms up, elbows flexed’ but, for apical tumours, it may be better to have the arms down (Figure 25.1).
Target volume
The type of plan created depends on the site of the tumour, whether central or peripheral. If the patient has undergone pneumonectomy, surgical clips may define the clinical target volume. It is important to ensure that beams pass through the resected space and spare the remaining contralateral lung (Figure evolves 25.2 and 25.3 ![]() ).
).
Usually, three fields are required for optimum dose distribution but, occasionally, if there is a small peripheral tumour, wedged opposed oblique fields may be used (Figure evolve 25.4 ![]() ).
).
Depth dose tables estimating the dose at each point in tissue have been derived from experiments in solid tissue. Since air is much less dense, there is less scatter of the beam on traversing lung. As a result, the dose is 3% greater for every centimetre of lung traversed. Therefore, on calculating the dose to the tumour, the lung correction factor must be applied (Figure evolves 25.5 and 25.6 ![]() ).
).
Tolerances
The spinal cord should receive no more than 40–44 Gy depending on fraction size. Twelve centimeters of oesophagus should receive no more than 50 Gy. Heart doses at present are hard to define. They may not be reported routinely but the whole heart should receive less than 40 Gy and two thirds of it less than 55 Gy (Figure evolve 25.7 ![]() ).
).
Doses
Suggested radiation doses are given in Table 25.6.
Table 25.6 Suggested radiation doses for NSCLC
| Indication | Suggested dose regimens |
|---|---|
| Radical postoperative dose | 50 Gy 20–23 fractions given in 4–5 weeks |
| Radical radiotherapy | 55 Gy 20 fractions given in 4 weeks 60 Gy 30 fractions given in 6 weeks |