Fig. 3.1
Right (a) and left (b) uterine blood flow measured by 2D Doppler ultrasound
Flow velocity waveforms are obtained from the ascending main branch of the uterine artery on the right and left side of the cervix in a longitudinal plane before it enters the uterus. The ‘gate’ of the Doppler is positioned when the vessel with good colour signals is identified on the screen. The PI and RI of the uterine arteries were calculated electronically when three similar, consecutive waveforms of good quality were obtained.
Good uterine blood flow as shown by low PI or RI is correlated with successful IVF outcomes [12, 13]. Steer et al. [12] classified PI measured on the day of ET as low, medium and high in the ranges of 0–1.99, 2.00–2.99 and ≥3.00, respectively, and reported a 35 % implantation failure when PI was >3.0. Using a PI upper limit of 3.0 [12] or 3.3 [13], the uterine Doppler flow indices have a high negative predictive value and sensitivity (in the ranges of 88–100 % and 96–100 %, respectively) and a relatively higher range of positive predictive value and specificity (44–56 % and 13–35 %, respectively) when compared with endometrial thickness and pattern [5].
Uterine artery Doppler study may not reflect the actual blood flow to the endometrium as the major compartment of the uterus is the myometrium and there is collateral circulation between uterine and ovarian vessels. I have shown 2D Doppler study of uterine vessels is a poor reflection of subendometrial blood flow by 3D power Doppler in both stimulated and natural cycles as endometrial and subendometrial 3D Doppler flow indices were similar among patients with averaged uterine PI <2.0, 2.0–2.99 and ≥3.0. [14].
Endometrial and Subendometrial Blood Flow by 2D Doppler
Endometrial and subendometrial blood flow examined by colour (Table 3.1) and power Doppler (Table 3.2) was correlated with implantation or pregnancy rates during IVF treatment. 2D Doppler flow indices of spiral arteries such as PI and PSV are not predictive of pregnancy [8, 19, 22], although Battaglia et al. [16] and Kupesic et al. [23] found significantly lower spiral artery PI in pregnant cycles than nonpregnant cycles.
Table 3.1
Summary of studies of endometrial blood flow by 2D colour Doppler
Study | IVF cycles | USS parameters | USS day | Results |
|---|---|---|---|---|
Popovic-Todorovic et al. [15] | 96 cycles using a long protocol | Spiral PI and PSV | hCG | No difference in subendometrial PI and PSV between pregnant and nonpregnant cycles |
Presence of endometrial and subendometrial flow | Absent subendometrial flow associated with no pregnancy | |||
Battaglia et al. [16] | 60 cycles | Uterine and spiral PI | OR | Uterine and spiral PI lower in pregnant than nonpregnant cycles |
Presence of endometrial blood flow | Absent subendometrial flow associated with no pregnancy | |||
Chien et al. [17] | 623 cycles using ultrashort and ultralong protocols | Uterine and spiral PI and RI | ET | Significantly lower implantation and pregnancy rates in patients without endometrial/subendometrial flow |
Presence of endometrial and subendometrial (<10 mm) blood flow | Presence of subendometrial flow 5.9 times to become pregnant than those with absent flow |
Table 3.2
Summary of studies of endometrial blood flow by 2D power Doppler
Study | IVF cycles | USS parameter | USS day | Results |
|---|---|---|---|---|
Yang et al. [18] | 95 cycles using long and short protocols | Intraendometrial power Doppler area (EDPA) <5 mm2; ≥5 mm2 | OR | Higher EDPA in pregnant cycles |
Endometrium ≥10 mm | Lower implantation and pregnancy rates when EDPA <5 mm2 | |||
Yuval et al. [19] | 156 cycles using a long protocol | PI and RI | OR and ET | No difference in any USS parameters between pregnant and nonpregnant cycles |
Contart et al. [20] | 185 cycles using a long protocol | Fundal region along transverse plan; grades I, II, III and IV according to visualisation of power Doppler in the quadrants | hCG | Implantation and pregnancy rates similar in all grades of endometrial vascularity |
Schild et al. [8] | 135 cycles using a long protocol; first cycle only | PI and PSV of vessels in endometrium and subendometrial area (<5 mm) | OR | No difference in spiral artery PI and PSV between pregnant and nonpregnant cycles |
Non-detectable spiral blood flow was not associated with a lower implantation rate | ||||
Maugey-Laulon et al. [21] | 144 cycles using a long protocol | Presence of endometrial and subendometrial blood flow | ET | Absent endometrial and subendometrial flow associated with a lower pregnancy rate |
Yang et al. [18] used a computer software to measure the area and intensity of colour signals present in the endometrium in a longitudinal axis, i.e. intraendometrial power Doppler area (EDPA). Significantly higher EDPA was found in pregnant cycles than nonpregnant cycles (8.8 mm2 vs. 5.8 mm2 respectively). Patients with EDPA <5 mm2 had significantly lower pregnancy rate (23.5 % vs. 47.5 %; P = 0.021) and implantation rate (8.1 % vs. 20.2 %; P = 0.003) than those with ≥5 mm2. Contart et al. [20] graded endometrial blood flow by the visualisation of power Doppler in the quadrants in the fundal region of the transverse plane but could not demonstrate any predictive value of such grading system.
Endometrial and Subendometrial Blood Flow by 3D Doppler
3D power Doppler ultrasound with the aid of the VOCAL® (Virtual Organ Computer-Aided Analysis) imaging program for the 3D power Doppler histogram can be used to measure the endometrial volume and indices of blood flow within the endometrium (Fig. 3.2). Vascularisation index (VI), which measures the ratio of the number of colour voxels to the number of all the voxels, is thought to represent the presence of blood vessels (vascularity) in the endometrium, and this was expressed as a percentage (%) of the endometrial volume. Flow index (FI), the mean power Doppler signal intensity inside the endometrium, is thought to express the average intensity of flow. Vascularisation flow index (VFI) is a combination of vascularity and flow intensity [24].
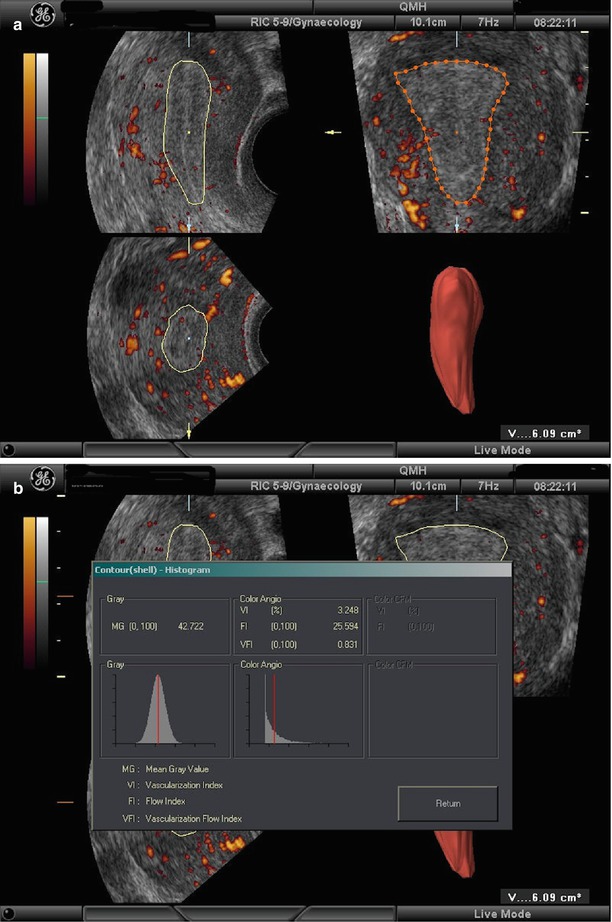
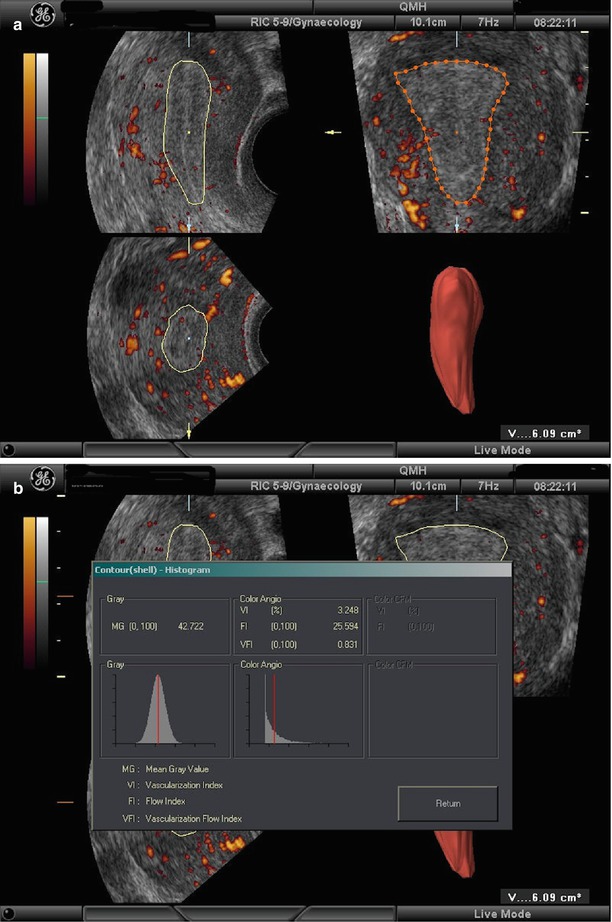
Fig. 3.2
Endometrial volume (a) and blood flow (b) measured by 3D Doppler ultrasound
The subendometrium can be examined through the application of ‘shell imaging’ which allows the user to generate a variable contour that parallels the originally defined surface contour. The VI, FI and VFI of the subendometrial region are obtained accordingly (Fig. 3.3). The intra-observer reliability and interobserver reliability of endometrial and subendometrial blood flow by 3D power Doppler have been confirmed to be high with all measurements obtaining an intra-class correlation of above 0.9 [25, 26].
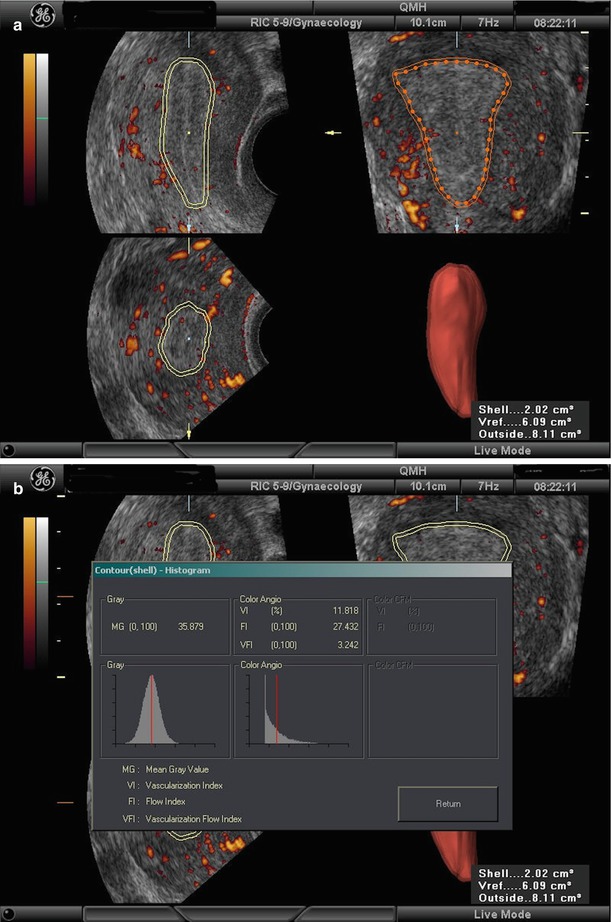
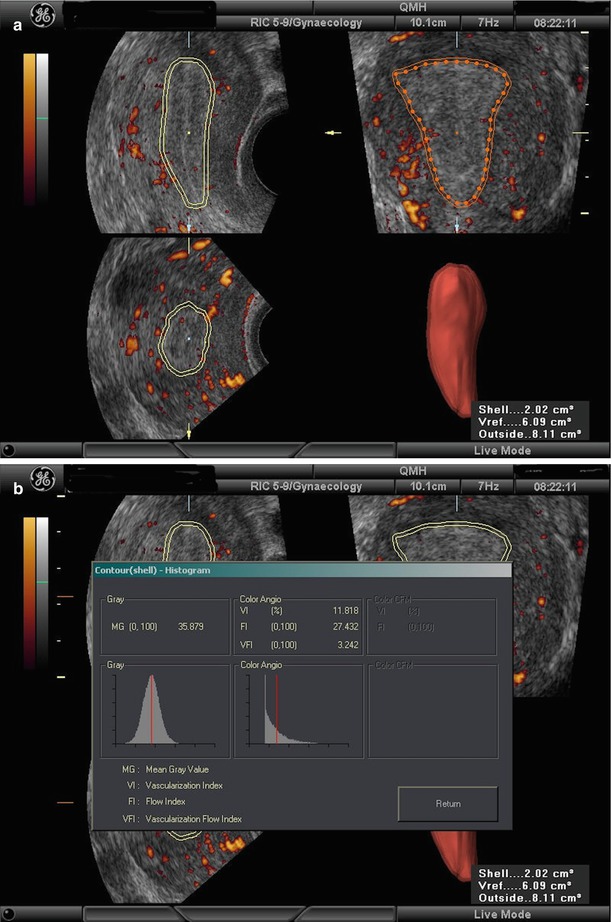
Fig. 3.3
Subendometrial volume (a) and blood flow (b) measured by 3D Doppler ultrasound
Studies addressing the role of endometrial and subendometrial blood flow measured by 3D Doppler in IVF treatment are summarised in Table 3.3. Schild et al. [27] measured the subendometrial blood flow after pituitary downregulation but prior to ovarian stimulation and showed that subendometrial VI, FI and VFI were significantly lower in pregnant cycles than nonpregnant ones. Logistic regression analysis found that the subendometrial FI was the strongest predictive factor for the pregnancy outcome among other 3D Doppler flow indices.
Table 3.3
Summary of studies of endometrial and subendometrial blood flow by 3D power Doppler ultrasound
Study | IVF cycles | Inclusion/exclusion criteria | USS day | Results |
|---|---|---|---|---|
Schild et al. [27] | 75 cycles using a long protocol | Inclusion criteria | Before stimulation | Subendometrial VI, FI and VFI lower in pregnant than nonpregnant cycles |
ET 2 days after TUGOR | Downregulation confirmed (endometrium <5 mm, no ovarian cyst of >2.5 cm, serum oestradiol <60 pg/mL) | Subendometrial FI is the strongest predictive factor for IVF in logistic regression analysis | ||
Kupesic et al. [23] | 89 cycles using a long protocol | Inclusion criteria | ET (hCG +7) | Higher subendometrial FI in pregnant cycles |
Blastocyst transfer 5 days after TUGOR | Serum FSH < 10 IU/L | |||
No fibroid, ovarian cysts and ovarian endometriosis | ||||
Wu et al. [28] | 54 cycles; first cycle only (details of ovarian stimulation and ET not given) | Inclusion criteria | hCG | Subendometrial VFI higher in pregnant cycles |
Age <38 years | ||||
Normal uterine cavity | ||||
Serum FSH <15 IU/L | ||||
≥2 good quality embryos | ||||
Dorn et al. [29] | 42 cycles using a long protocol | Exclusion criteria | OR | No difference in subendometrial VI, FI and VFI between pregnant and nonpregnant cycles |
Polycystic ovary syndrome | ||||
Endometrium <6 mm | ||||
Gynaecological surgery | ||||
Järvelä et al. [30] | 35 cycles using a long protocol | Exclusion criteria | After stimulation and OR | No difference in endometrial and subendometrial VI between pregnant and nonpregnant cycles on both days |
ET 2 days after TUGOR | Uterine fibroids | |||
Endometriosis | ||||
Single ovary | ||||
Previous operation on uterus or salpingectomy | ||||
Ng et al. [31] | 451 cycles using a long protocol; first cycle only | Inclusion criteria | OR | Endometrial VI and VFI lower in pregnant cycles |
ET 2 days after TUGOR | Normal uterine cavity on scanning | |||
Ng et al. [32] | 193 cycles | Inclusion criteria | LH + 1 | No difference in endometrial and subendometrial 3D Doppler flow indices between pregnant and nonpregnant cycles |
Frozen-thawed embryo transfer cycles | Normal uterine cavity | |||
Mercè et al. [33] | 80 cycles using a long protocol | Inclusion criteria | hCG | Higher endometrial VI, FI and VFI in pregnant cycles |
First cycle | ||||
Normal uterine cavity | ||||
Serum FSH <10 IU/L | ||||
Regular cycles | ||||
Non-smokers | ||||
Ng et al. [34] | 293 cycles using a long protocol | Inclusion criteria | OR and ET | No difference in endometrial and subendometrial 3D Doppler flow indices on the 2 days and changes in these indices between pregnant and nonpregnant cycles |
ET 2 days after OR | First cycle | |||
Normal uterine cavity |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree