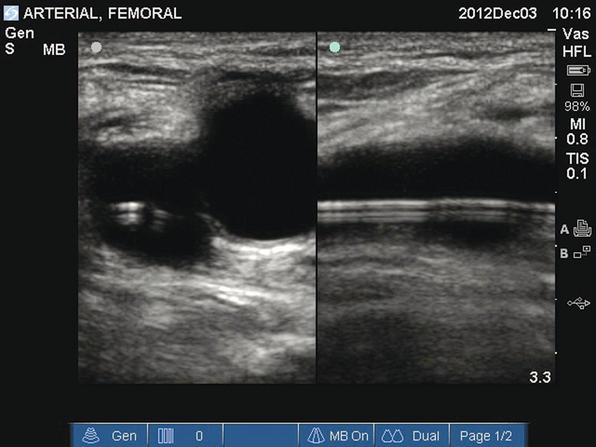
16 Arterial catheterization is a frequent and essential procedure that is used in the intensive care unit (ICU) for accurate hemodynamic monitoring and repeated sampling of blood for analysis.1 Blind or palpated catheter insertion can be difficult because pulsations and landmarks are often obscured by edema, obesity, hypotension, hypovolemia, and small-caliber vasculature. Repeated attempts at catheterization are often less successful because of arterial spasm. In addition, the external landmarks used for catheter placement are not necessarily predictive of the underlying anatomy. This is especially true of the femoral vasculature, for which it has been reported that a portion of the common femoral artery overlaps the common femoral vein up to 65% of the time.2–5 Recent studies and meta-analyses have shown the utility of ultrasound for guiding arterial catheterization, with increased success and decreased complication rates similar to those found with the use of ultrasound for central venous catheter placement.6–10 A meta-analysis by Shiloh et al demonstrated a 71% improvement in first-attempt success and a number needed to treat of six when using ultrasound guidance for radial artery catheterization.9 Ultrasound-guided arterial catheterization has been shown to be beneficial in pediatric and adult populations in the ICU, surgical, and interventional settings. B-mode (two-dimensional) ultrasound is most often used for arterial catheterization and has been shown to be superior to Doppler ultrasound techniques. Real-time visual guidance is superior to marking a spot with ultrasound and then trying to locate a vessel without guidance.11–15 B-mode (two-dimensional) ultrasound is used for arterial catheterization. Arteries appear hypoechoic on B-mode in contrast to the adjacent soft tissue (isoechoic). A key step in ultrasound-guided arterial catheterization is identification of the target artery and the adjacent vein. Pulsatility distinguishes arteries from veins. Partial arterial compression will accentuate pulsations that may be difficult to visualize in smaller-caliber vessels or hypotensive patients.16 As opposed to veins, arteries should not be fully compressible with mild pressure from the transducer. As a rule, the artery should begin to indent when the vein is completely collapsed by pressure from the transducer. In addition, color power Doppler and pulsed wave Doppler can be used to distinguish arterial and venous pulsation. Color Doppler can be used to distinguish the flow of blood in relation to the transducer. Blood cells moving toward the transducer produce a positive Doppler shift, and by convention the latter is represented as red color flow on color mode. A negative Doppler shift, produced by blood cells moving away from the probe, is represented by blue color flow accordingly. As blood velocity increases, so does the Doppler frequency. Lighter shades of red or blue indicate higher velocity, whereas deeper shades indicate lower velocity. Absent flow or low-flow states fail to produce a Doppler shift and are represented as black. For color flow to be present there must be flow in the direction of the ultrasound beam. The angle of insonation (the angle between the direction of flow and the ultrasound beam) is the key factor when using color Doppler (see Chapters 1 and 8). Doppler frequency increases as the ultrasound beam becomes more aligned with the direction of flow (parallel to the vessel). If the flow is perpendicular to the beam, no relative motion will be detected. It is dependent on the operator to appropriately angle the transducer in a fashion that will create flow toward the transducer as arterial or red-shifted. In addition to being red-shifted, arterial flow will be visualized as pulsatile and of higher velocity than venous flow. Venous flow will be blue-shifted and demonstrate continuous flow when compared with arterial flow. Similarly, pulsed wave Doppler can be used to measure changing blood velocity at a single point. A flow waveform of frequency shift (velocity) over time is created. Arterial flow demonstrates pulsatility, representative of the cardiac cycle, with a systolic peak and diastolic nadir. Venous flow is represented by continuous, low-velocity flow. It is important to not rely on Doppler techniques alone, because pulsatile venous Doppler flow can be demonstrated in patients with elevated right atrial and central venous pressure.17,18 Before the procedure a preliminary scan of prospective sites should be performed to identify the most appropriate vessel for catheterization. Frequently, there is asymmetry in the size of the arteries between the two sides of the body. Common locations for arterial catheterization include the radial, femoral (Figure 16-1), brachial, axillary, and dorsalis pedis arteries. After determining the target artery, the site is prepared in sterile fashion with full barrier precautions. An assistant applies sterile conducting gel to the uncovered probe and holds it vertically. The sterile operator inserts a hand into the sheath, holds the probe, and inverts the sheath over the probe and cable. Additional sterile ultrasound gel is then applied to the sterile probe. Figure 16-1 Transverse and longitudinal views of the femoral artery. A femoral arterial catheter can be visualized within the lumen of the vessel. If using a one-person technique, the operator controls the needle with the dominant hand and the transducer with the nondominant hand. When using a two-person technique, an assistant in full sterile barrier precautions controls the transducer. When compared with the two-person technique, the one-person technique has been reported to be learned easily and has improved first-pass and overall success for central venous catheterization.11,15
Ultrasound-guided arterial catheterization
Overview
Procedure and instrumentation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine