Fig. 2.1
Diagnostic US saline enema. (a) Tube inserted, colon filled and distended with saline. (b) Increasing filling of more proximal bowel loops after advancing tube under constant saline irrigation. (c) The soft feeding tube advanced further – no distension can be achieved, no saline passes to more oral loops, no meconium plugs seen at that level – indicative for atresia
Tube removed after sufficient filling and distention of entire colon, assess in longitudinal + axial sections.
Perineal US can be applied to observe defecation, particularly observe shape of rectum and transition zone to anal canal as well as respective angulations secondary to pelvic floor activity after withdrawing the catheter (Fig. 2.2).
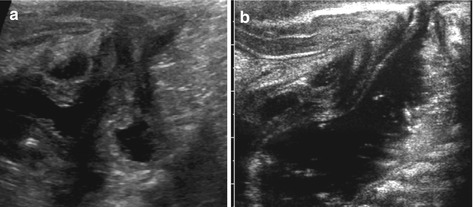
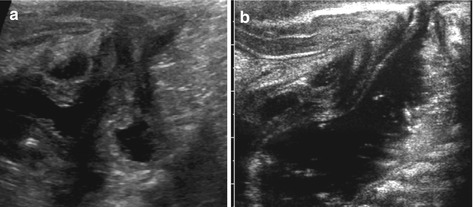
Fig. 2.2
Perineal US for defecation. (a) Perineal US demonstrates bladder, urethra, narrow and atypical anal canal and fluid-filled rectal pouch. Note no distal opening of the anus and no proper anal canal in a neonate with anal atresia. (b) Still image from a video clip during defecation after saline enema, perineal sagittal view (neonate): open short rectal canal, atypical shape of recto-pubic angle
2.2.3 Therapeutic Sonographic Enema
Same procedure as above can be used for reduction of intussusception or meconium plug.
How to do: Basically same technique as described above:
Dedicated precautions are recommended: analgesia/sedation, IV infusion for hydration and electrolyte balance, sometimes antibiotic prophylaxis, physiological monitoring.
For successful reduction, higher pressures have to be applied, thus larger tubes are necessary. Filling pressure = 80–100 cm H2O (less in preterms/neonates):
Success is seen if saline enters beyond point of obstruction: in intussusception unhindered reflux into ileum is mandatory; in meconium obstruction, mixing of meconium with saline and mobilisation of plugs indicates success (Fig. 2.3).
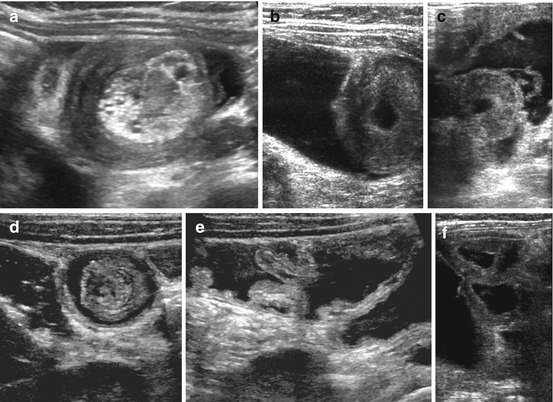
Fig. 2.3
Therapeutic saline enema: reduction of intussusception (or meconium ileus). (a) Typical US image of intussusception (with entrapped fluid). (b) Enema fluid starts to push back the intussusception, enema fluid (saline) filling of colon from saline enema (80 cm H2O water pressure). (c, d) Gradually fluid is reducing the intussusception, increasing fluid around head of invaginated bowel. (e) Intussusception successfully reduced – fluid passes through somewhat swollen ileocoecal valve. (f) Enema has reached small bowel which is filled with enema fluid from now unhindered reflux into ileum
Repeated attempts after a pause can be easily performed and increase success rate.
Mandatory to seal anal canal by taping or manual compression; use of balloon catheters not recommended due to higher risk for perforation during uncontrolled pressure increase.
Benefits: Easily repeatable, furthermore, guided by US manual/transducer massage can assist reduction in intussusception or mobilisation of meconium; procedure applicable at bedside. Some only massage the intussusceptum out of the intussusciepiens manually through the abdominal wall (using same technique as surgions would intra-operatively) without the enema procedure, with some reported success.
Restrictions: Less overview; fluid instead of air (as used for pneumatic reduction) – less elastic – higher perforation risk.
2.2.4 US Genitography
Indications: Equivocal findings on US in suspicion of genital malformations.
How to do: With full bladder (or after filling of bladder), vagina filled after gentle catheterisation. Same saline infusion technique with constant drip and pre-filled catheter as for ce-VUS (see below, Sect. 2.2.5):
Distension, size/shape of vagina clearly delineated, potential fistula visible, atretic/double vaginas, cysts, uterine cervix much better delineated; improves assessment of uterine malformations (Fig. 2.4).
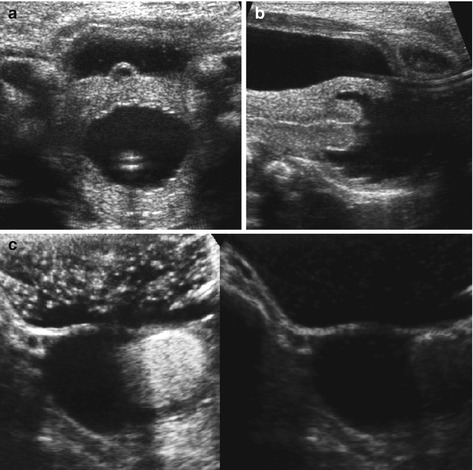
Fig. 2.4
US genitography. (a)Axial transvesical section: vagina with catheter during filling with saline infusion for US genitography. (b) Longitudinal transvesical view: nicely outlined uterine cervix after distension and filling of vagina via saline infusion. (c and d, or lower row) ce-US genitography: additionally diluted US-CM added to see if there is a connection between the two vaginas in a girl with uterus didelphis and hydrocolpos of atretic hemivagina; no contrast seen in right-sided cystic-obstructed hemivagina, normally filled and distended echoic contrast-filled main left vagina (double image technique, right side is dedicated contrast image, left side is fundamental image)
3DUS with coronal reconstructions helpful and improves classification (Fig. 1.33).
Perineal approach + complementing upper abdominal/urinary tract study added (Figs. 2.5 and 1.24).
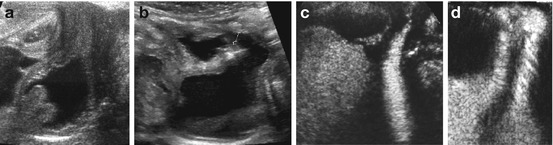
Fig. 2.5
Perineal US for vaginal pathology after filling with saline/during voiding. (a) Vagina filled with saline after catheter is withdrawn, cervix lips nicely visualised. (b) Perineal sagittal US depicts an obvious fistula (+ +) to urine-filled distended vagina. (c) Additional diluted US-CM instillation (ce-VUS + ce-US-genitography) demonstrates intact vagina and separated course of urethra (during voiding) and vagina. (d) Distal common tract of urethra and vagina (urogenital sinus tract) depicted on ce-US genitography by sagittal perineal access during voiding in a newborn girl with adrenogenital syndrome
Eventually catheters removed, vagina observed during/after voiding for urine influx into vagina.
In case of suspected fistulae – additional instillation of US-CM to enhance structures/clearly delineate connection between different cavities.
2.2.5 Contrast-Enhanced Voiding Urosonography (ce-VUS)
US method for detection of vesico-ureteric reflux (VUR).
Although US-CM presently not licensed for paediatric use, thousands of investigations have been performed – high success rate, low complication rate and reliable results well documented. (See also Fig. 1.23.)
Indications: Recommended in girls and for follow-up investigations, as well as for family screening. With increasing ability to properly assess urethra also applicable to male infants.
NOTE: Initial thorough detailed comprehensive US investigation of entire urinary tract including post-void assessment mandatory before performing ce-VUS.
How to do: After assuring sterile urine and initial US assessment performed, urethral catheter placed (or suprapubic puncture) and bladder emptied:
Then bladder gradually filled by drip infusion (infusion height <40 cm above bladder level – physiologic filling pressure):
Potential antibiotics added (or antibiotic prophylaxis).
Alternating scanning of retrovesical space + bladder as well as both kidneys during filling:
Drip infusion may be used as manometer to see moments of increased bladder pressure during filling – may indicate unstable bladder, helps to depict moments of high pressure VUR.
Fractional instillation of US-CM (at present mostly Sonovue®), concentration = 0.2–1.0 % of actual bladder filling volume (Fig. 2.6).
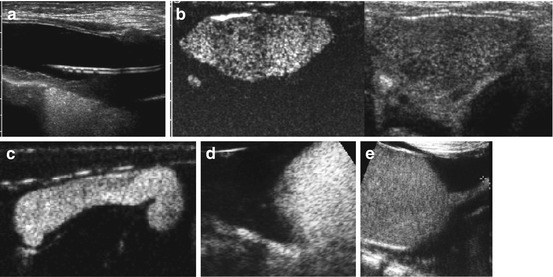
Fig. 2.6
ce-VUS: bladder and ureter. (a) Filling of the bladder with saline drip infusion (30–40 cm H20 pressure) via catheter. (b) Dual image technique (left – contrast image): US-CM instilled – bladder lumen gets distended with echogenic material. Note the echoic CM-filled distal right ureter behind the bladder, only clearly detectable by the contrast image. (c) Single contrast image: echogenic contrast in a megaureter in dilating VUR (V°). (d) Single contrast image: contrast reflux into narrow distal ureter, with gapping and pathologically shaped UVJ. (e) Voiding on ce-VUS (transvesical sagittal access in an infant): only proximal urethra (+ +) seen from abdominal sagital approach/view
Ongoing alternating assessment of bladder, retrovesical space/distal ureter and both kidneys.
NOTE: In first years of life, cyclic filling (three cycles) recommended.
Scanning continued when bladder is filled (urge or spontaneous voiding).
Potentially assess urethra by perineal US.
After voiding, check kidneys for potential refluxed US-CM within collecting system, CM drainage dynamics, and bladder for residual urine/diverticulae.
At last cycle, catheter withdrawn for proper view of unobstructed urethra on perineal US, unless same catheter used for complementing focused fluoroscopic VCUG.
Diagnosis: Any US-CM in upper urinary tract/ureters seen as echogenic bubbles – indicative of VUR (Fig. 2.7). Also try to note potential CM influx into vagina. Establish grading related to international VUR classification system (see Table 1.3).