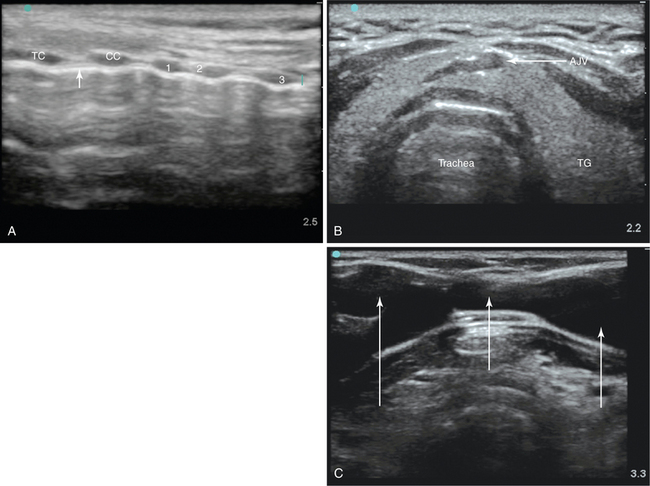
52 Kearney et al1 reported rates of perioperative morbidity of 6% and procedure-related mortality of 0.6%. Placement complications include hemorrhage, accidental extubation, pneumothorax, formation of a false passage, damage to tracheal rings, and perforation of the posterior tracheal wall. Delayed bleeding is typically seen a few days after PT and is due to either minor vessel damage or erosion into high or aberrant mediastinal vessels. The latter can be life-threatening and necessitates immediate surgical input. The most important late complications are tracheal stenosis, tracheomalacia, and vocal cord dysfunction, which could adversely affect the quality of life of ICU survivors.1,2 Point-of-care ultrasound (US) is increasingly being used for the management of critically ill patients. Despite wide application, US-guided percutaneous tracheostomy (USGPT) is not yet routine practice in many centers. Preprocedural, real-time US can reduce some of the complications just mentioned, morbidity, and possibly the occasional mortality associated with PT.3–8 This chapter focuses on the role of US for PT, the sonographic anatomy of the anterior neck region, and the evidence available for USGPT. Typically, a high-frequency (5- to 10-MHz), high-resolution, small-footprint, vascular-type linear probe is used for US scanning of the trachea and paratracheal area. Because air within the larynx and trachea has very high acoustic impedance, which results in high reflectance of the sound waves, US has limited ability to depict the inside of the air-filled airways and generates a characteristic acoustic shadow. Despite this shortfall, the superficial location of the larynx and trachea allows delineation and visualization of the anterior and lateral walls. Both the thyroid and cricoid cartilage are clearly visible as midline echogenic structures separated by the echolucent cricothyroid membrane with characteristic acoustic shadow underneath.4,5 Below, the cartilaginous tracheal rings, which are characterized by a thin acoustic shadow, are easily visible along with pretracheal tissue and vessels. In the longitudinal view, the thyroid, cricoid cartilage, and individual tracheal rings can be seen anterior to the hyperechogenic line formed by the air-tissue interface at the anterior tracheal wall. The longitudinal view allows identification of the intercartilaginous spaces and selection of the most appropriate needle puncture site, which can be performed in real time with a sterile probe cover. However, the need for a probe with a small physical footprint and the inability to visualize the posterior wall of the trachea and paratracheal structures may limit the usefulness of this approach (Figure 52-1A).4,5
Ultrasound-guided percutaneous tracheostomy
Overview
Sonographic anatomy of the anterior neck region
Ultrasound-guided percutaneous tracheostomy