(1)
Department of Emergency Medicine, Virginia Commonwealth University Medical Center, P.O. Box 980401, Richmond, VA 23298-0401, USA
Electronic Supplementary Material
The online version of this chapter (doi:10.1007/978-3-319-68634-9_18) contains supplementary material, which is available to authorized users.
Keywords
Peripheral intravenous accessCentral venous catheterLumbar punctureNerve blockRegional anesthesiaParacentesisUltrasound-Guided Peripheral Intravenous Access
- (a)
Procedure Indications
Difficult intravenous (IV) access:
Risk factors for difficult IV access include:
Dialysis patient
Sickle cell patient
Diabetic patient
Chemotherapy patient
Dehydration
Obesity
Edema
IV drug abuse
History of difficult access
Multiple previous attempts without successful IV placement
- (b)
Procedure Complications
Infection, phlebitis, hematoma
Extraluminal placement
Dislodgement and infiltration
- (c)
Transducer Selection
Linear array
- (d)
Equipment
IV needle with angiocatheter:
Long catheters are preferred if available.
Figure 18.1—Long and short IV catheters.
Ultrasound gel:
Sterile surgical lubricant is recommended for deep vein access or when drawing blood cultures.
Antiseptic swab:
Chlorhexidine is recommended for deep vein access.
Tourniquet
Luer lock adapter
Saline flush
Adhesive dressing
Gloves
- (e)
Patient Position and Anatomical Landmarks
The patient should be supine with their arm extended and externally rotated:
Figure 18.2—Patient position for PIV placement
Blood vessels appear anechoic:
Veins are thin walled and compressible.
Arteries have thicker walls, typically pulsate, and are not compressible.
Figure 18.3—Ultrasound of the artery and vein.
The brachial vein runs adjacent to the brachial artery and median nerve within the upper medial arm.
The basilic vein runs medial to the brachial vessels.
Figure 18.4—Brachial and basilic vein positions.
- (f)
Preparation
Universal precautions should be utilized at all times.
Apply tourniquet.
Identify the vessel with ultrasound:
Success rate increases when the vein is less than 1.5 cm from the skin surface [1].
Clean transducer with antiseptic cloth.
Hold transducer with nondominant hand and place over the vessel:
Be careful not to apply pressure with the transducer as this will displace the vessel deeper within the arm and can compress the vein.
Figure 18.5—Transducer placement.
Adjust depth so that the vessel is in the center of the screen.
Increase gain so that needle will show up bright on the screen.
Figure 18.6—Ideal image for ultrasound-guided peripheral IV placement.
- (g)
Technique
Out-of-plane:
The vein will be imaged using a transverse or cross-sectional view.
The transducer marker should point in the same direction on the patient as on the ultrasound monitor.
Identify the vein in cross section:
Make sure the vessel is compressible before attempting access.
Insert the needle just distal to the transducer and enter the skin at a 15–30° angle:
Figure 18.8—Needle position relative to transducer
Needle tip will be visualized in the subcutaneous tissue as a small bright white dot:
Figure 18.9—Needle tip
As the needle is advanced closer to the vessel, the transducer should slide with the advancement to keep the needle tip visualized at all times.
Once the needle tip enters the vessel, drop the angle of the needle, and advance at least 2 mm to ensure the needle and the catheter are within the vessel lumen:
Figure 18.10—Needle in the vessel.
Remember: catheter tip sits back slightly from needle bevel so at the initial flash, it may not be far enough into the vessel to advance the catheter.
Stabilize the needle and slowly advance the catheter until it is completely within the vessel lumen.
Video 18.1—Out-of-plane peripheral IV placement.
In-plane:
The vein will be imaged using a longitudinal view of the vessel.
Place the transducer over the vessel with the marker pointed toward the needle:
This can also be done with the marker pointed away from the needle.
In this view, the vein will appear as an anechoic tube.
Insert the needle just distal to the leading edge of the transducer and enter the skin at a 15–30° angle:
Figure 18.11—Transducer and needle placement in long axis
If the needle is directly under the transducer beam, it will reflect the entire needle, and you can visualize it along its course into the vessel:
Figure 18.12—Long axis of needle toward the vein
Once the needle tip enters the vessel, drop the angle, and advance 2 mm to ensure the needle and the catheter are within the vessel lumen:
Figure 18.13—Needle in the vessel, long axis.
Remember: catheter tip sits back slightly from needle bevel so at the initial flash, it may not be far enough into the vessel to advance the catheter.
Stabilize the needle and slowly advance the catheter until it is completely within the vessel lumen.
Video 18.2—In-plane peripheral IV placement.
Completing the procedure:
Remove the tourniquet.
Flush the luer lock and tubing with saline to remove air bubbles, attach it to the catheter, and secure it in place with adhesive dressing.
Flush the catheter once inside the vessel:
The IV should flush easily.
If there is resistance or pain with the flush, the catheter is likely outside the lumen of the vessel and needs to be removed.
- (h)

Figure 18.1
Long and short IV catheters. Peripheral IV setup with short catheters (1.6 cm) and long catheters (2.1 cm)

Figure 18.2
Patient position for PIV placement. Extend and externally rotate the patient’s arm when preparing for ultrasound-guided peripheral intravenous catheter placement

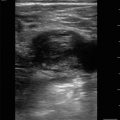
Figure 18.3
Ultrasound of the artery and vein. Arteries are circular with thick walls and pulsate when pressure is applied. Veins have thinner walls and will compress with pressure

Figure 18.4
Brachial and basilic vein positions. Approximate location of where the brachial and basilic veins lie within the arm

Figure 18.5
Transducer placement over the area of the basilic vein

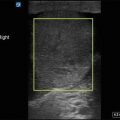
Figure 18.6
Ideal image for ultrasound-guided peripheral IV placement. Success rate increases when the target vessel is within 1–1.5 cm depth and in the center of the screen

Figure 18.7
In-plane vs. out-of-plane. (a) Is an in-plane approach and (b) is an out-of-plane approach

Figure 18.8
Transducer with needle entering into the skin. Place the transducer centrally over the vessel of choice with the nondominant hand. The dominant hand holds the needle with catheter at the center of the transducer ready to enter the skin at a 15–30° angle

Figure 18.9
Needle tip above the vessel. The needle tip is hyperechoic and seen just anterior to the vessel. Follow the needle tip through the layers of the skin and into the vein

Figure 18.10
Needle in the vessel, out-of-plane. The hyperechoic needle tip is seen within the center of the vein

Figure 18.11
Transducer and needle placement in long axis. Place the transducer centrally over the vessel of choice with the nondominant hand. The dominant hand holds the needle with catheter at the center of the transducer ready to enter the skin at a 15–30° angle

Figure 18.12
Long axis of needle toward the vein. Advance the needle toward the vessel, ensuring to visualize the entire needle and vessel the entire time

Figure 18.13
Needle in the vessel, in-plane. The in-plane approach allows for visualization of the entire needle as it enters the vein
Central Venous Catheterization
- 1.
Procedure Indications
- (a)
Inability to obtain peripheral IV access
- (b)
Emergent venous access
- (c)
Hemodynamic resuscitation
- (d)
Transvenous pacer placement
- (e)
Use of caustic or vasoactive medications
- (a)
- 2.
Procedure Contraindications
- (a)
Absolute:
Thrombus
Infection over the site of needle insertion
- (b)
Relative:
Anticoagulation.
Bleeding dyscrasia.
The patient is unable to cooperate.
- (a)
- 3.
Procedure Complications
- (a)
Arterial puncture
- (b)
Bleeding or hematoma
- (c)
Pneumothorax
- (d)
Thrombosis
- (e)
Infection
- (f)
Nerve injury
- (a)
- 4.
Transducer Selection
- (a)
Linear array
- (a)
- 5.
Equipment
- (a)
Central venous catheterization (CVC) kit
- (b)
Sterile transducer cover
- (c)
Sterile ultrasound gel
- (d)
Antiseptic swab (chlorhexidine)
- (e)
Sterile saline flush
- (f)
Sterile personal protective equipment
- (g)
Sterile adhesive dressing
- (a)
- 6.
Patient Position and Anatomical Landmarks
- (a)
Internal jugular (IJ) vein:
The patient should be supine with their head turned slightly to the opposite side of insertion site.
If the patient is hypovolemic, position the patient in Trendelenburg, or have them Valsalva to assist visualizing the IJ lumen.
Figure 18.14—Internal jugular vein.
Video 18.3—Internal jugular vein.
- (b)
Femoral vein:
Place the transducer at the inguinal ligament, and slide distally until the thin-walled vein is visualized just medial to the femoral artery:
Alternatively, feel for a femoral pulse, and place the transducer over this site to locate the femoral vein.
For patients who are hypovolemic, reverse Trendelenburg may assist to expand the vessel:
Use caution with collapsed veins as it is easier to penetrate the posterior wall.
Figure 18.15—Femoral vein.
Video 18.4—Femoral vein.
- (a)
- 7.
Get Clinical Tree app for offline access
Preparation
- (a)
Sterile personal protective equipment.
- (b)
Identify the vessel using ultrasound.
- (c)
Clean transducer with antiseptic cloth.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



- (a)