10 Ultrasound of the acute abdomen
Introduction
CT has become increasingly accessible in most trauma centres, and has the advantage of demonstrating structures not demonstrable on ultrasound. This means that trauma victims with multiple injuries are often best served by immediate and comprehensive CT. However, the risk to the patient from the radiation dose must be carefully balanced by the potential benefit of the diagnostic process.1 Women with probable gynaecological pain, some paediatrics and the acutely ill, unstable patients are likely to benefit from a comprehensive ultrasound examination by a trained practitioner with good-quality equipment.
The accuracy of the ultrasound scan is directly attributable to the skill and experience of the operator.2 For instance, a detailed knowledge of the anatomy, and therefore potential communications, of the peritoneal and retroperitoneal fascial spaces is essential in order to understand the significance and likely origin of an abdominal fluid collection. A left iliac fluid collection may simply be due to local causes such as a diverticular abscess, but could be the result of fluid tracking from a leaking aortic aneurysm or an acutely inflamed or ruptured pancreas.
Trauma
Blunt or penetrating trauma to the torso, frequently due to a road traffic accident (RTA) or other forms of accident or violence, is a frequent cause of referral to most emergency departments. Internal organ injury as a result of trauma is extremely difficult to assess clinically, especially as many patients are admitted unconscious or in a highly unstable condition. Such trauma patients may require emergency laparotomy and ultrasound has been shown to be an invaluable tool in the triage process.3,4 CT has the advantage of being able to recognize other injuries which may be present, such as bony, spinal or retroperitoneal trauma which may not be accessible to ultrasound investigation, and is often the first choice for imaging in multiple injury trauma patients.
FAST
FAST (focused assessment with sonography for trauma) has become widely adopted in many trauma centres. This system uses a limited scan by emergency physicians to identify the presence of free fluid on ultrasound. Results are highly dependent on proper training, and a number of standardized training and accreditation programmes have been devised, notably by the American College of Emergency Physicians.5 FAST scanning involves a minimum four-view examination, principally to detect the presence of fluid which may result from the rupture of internal organs. The four-view scan should include the right and left flanks (for hepatorenal space, perisplenic regions and spaces above and below the diaphragm), the subcostal region (to include the pericardial space) and the pelvis (retrovesical and retrouterine spaces).6
Free fluid is associated with numerous types of injury including rupture of the liver, spleen, kidney, pancreas or bowel (Fig. 10.1). Free fluid in the pelvis may be difficult to detect (due to overlying bowel and underfilled bladder) unless the patient is put into the Trendelenburg position, allowing it to collect in the pelvis under the influence of gravity. Ultrasound is more successful in detecting free fluid than in detecting organ injury directly.7,8 One study reported a 98% sensitivity for detection of fluid, but only 41% of organ injuries could be demonstrated.9 FAST has so far failed to demonstrate any population benefit10 and its use is difficult to support on evidence-based grounds. However, there may be evidence for a reduction in the interval between admission and surgery for some patients, with potential resource benefits.11
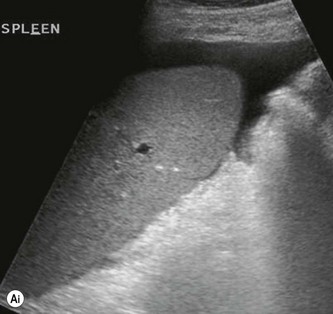
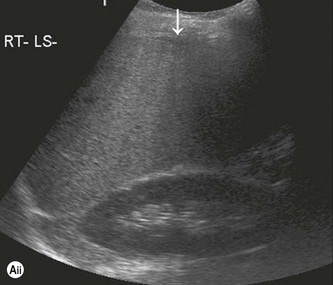



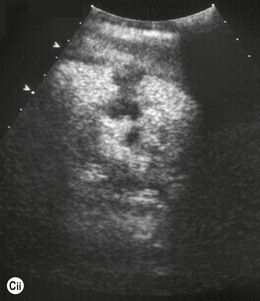
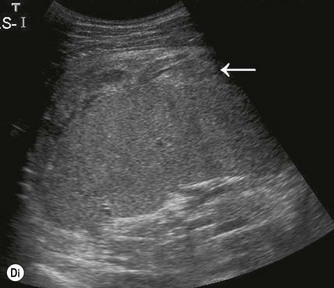
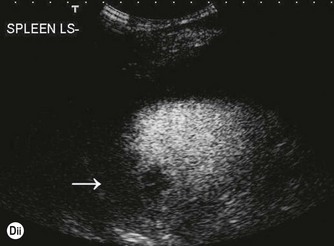
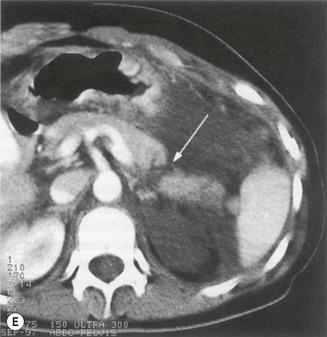
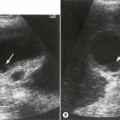
Fig. 10.1 • (Ai) The presence of free fluid in a trauma patient infers organ injury.
(Aiii) When the focal zone is placed in the near field.
(Cii) CEUS confirms a splenic laceration which was managed conservatively.
(Dii) CEUS demonstrates the injury at the dome of the spleen (arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree