Fig. 22.1
A short, thin-lumen, T-shaped uterus. Saline 3D US may replace the radiologic hysterography in similar cases. 2D US may be difficult to measure and interpret because of thin lumen cavity

Fig. 22.2
A very anteverted 3 cm deep uterine cavity depicted on MRI. A skilled vaginal US may replace the MRI and result in a significant cost savings

Fig. 22.3
Pre-ET vaginal US measurement of cervical-fundal distance allows accurate ET catheter placement
Tactile ET Versus Ultrasound-Guided ET
The optimal area of embryo deposition in the uterine cavity is probably 1–1.5 cm from the fundus resulting in higher PR [15, 16]. Evidence-based data demonstrated that US-guided ET will result in easier ETs and significantly improve ART outcome [11–14]. These RCTs and meta-analysis compared the main outcomes of clinical touch ETs versus ultrasound-guided ETs: implantation, clinical pregnancies, and live birth rates. In addition, other parameters were investigated: miscarriage rate, multiple and ectopic pregnancies rate, difficult or failed transfers, the need for instrumental assistance during the transfer (e.g., stylette, tenaculum, dilatation), signs of cervical or endometrial trauma (e.g., presence of blood, mucus, or both), and percentage of retained embryos. While few studies have found no significance in ART outcomes, most RCTs and the meta-analysis concluded that ultrasound guidance improves the chances of clinical pregnancies and live birth compared to the clinical touch method. A recent analysis showed that blood on the catheter is associated with decreased implantation rates, clinical pregnancy rates, and live birth rates when compared to no blood, which is easier to attain when performing US-guided ET [17]. Furthermore, it increases the ease of transfer rate and significantly decreases the chance of a difficult transfer [18], the need for instrumental assistance, and the failure to transfer with the assigned catheter. The incidence of finding blood on the catheter tips after US-guided ET was significantly lower. Adding ultrasound had no significant effect on finding mucus on the catheter tips, percentage of transfer with retained embryos, and the rate of multiple pregnancies, ectopic pregnancies, and spontaneous miscarriages.
Routine US use before, during, and post-ET has largely eliminated the discordance between mock ET and live ET [19]. US guidance has reduced unrecognized events such as 180° curling of the inner catheter and cervical deposition of the embryos. US prevents inadvertent embryo injection into the fallopian tube and directly into the uterine wall.
US-guided transmyometrial ET (Fig. 22.4) can be easily performed in the rare occasion when catheter access into the uterus is impossible [20, 21]. This alternative US-guided approach eliminates an unplanned laparoscopic intratubal ET. This technique is usually performed under conscious sedation using a coaxial needle outfitted with a matching ET catheter.
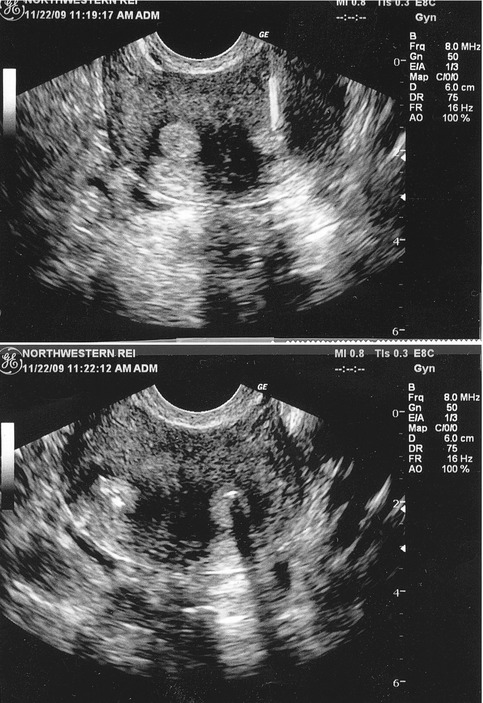
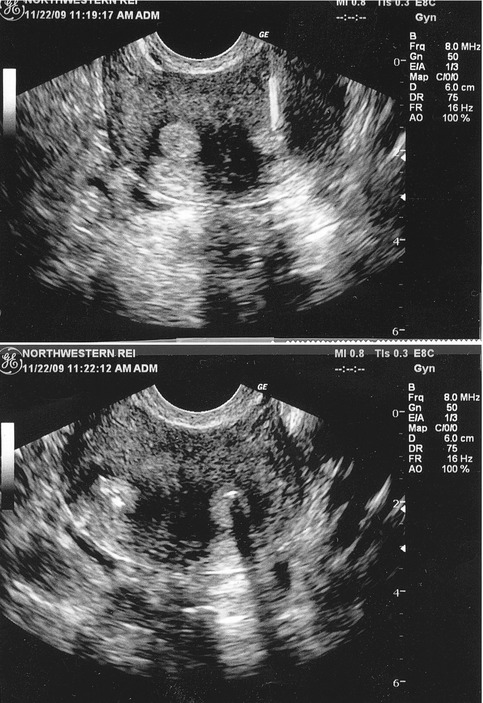
Fig. 22.4
Vaginal US-guided transmyometrial needle placement in a partially fused bicornuate uterus (upper figure right). Bubble markers are present in both right and left uterine horns depicting proper bilateral placement of one embryo in each uterine cavity (lower figure)
There are several mechanisms by which ultrasound-guided ET may improve ART outcome. The full bladder needed for transabdominal US straightens the angle between the cervix and the uterus. Avoiding endometrial indentation and uterine contractions as well as confirming the position of the tip of the catheter at the desirable site for embryo deposition seems to be the predominant mechanism by which US guidance improves ART outcomes.
Transvaginal Versus Transabdominal Ultrasound for ET
Transabdominal ultrasound in ET has been the most commonly reported form of US guidance for ET. Typically during such an US, the patient needs to have a full bladder. The full bladder is needed for the transabdominal visualization of the endometrial canal and it will also straighten the uterocervical angle, which is one of the main benefits of a full bladder. This in turn will make the transfer easier. However, this may cause additional cramping and discomfort during the ET to the patient, which may have an impact on clinical PR and increase times, as physicians may need for the bladder to fill and distend. A transvaginal US does not cause such issues, but does come with its own difficulties. Although it may give a better visualization of the uterocervical angle and clearly delineate the catheter tip, it is technically more difficult to perform. It needs to be placed in the vagina, in addition to a speculum and catheter for ET. Several RCTs demonstrated no difference in overall pregnancy, live birth, or implantation rate when comparing a transabdominal to transvaginal US [22, 23]. While the duration of the procedure is significantly longer with the TVUS, it was associated with increased patient comfort due to the absence of bladder distension [23].
Training in Embryo Transfer
Pregnancy rates have been shown to vary between different physicians performing ET, even at the same practice [24]. US-guided intrauterine inseminations (IUIs) have been used to train fellows in reproductive medicine before allowing them to perform a live ET. Live US ET guidance minimizes the potential complication of myometrial contractions. The post-ET marker bubbles visualized on US verify mid-cavity embryo placement (Fig. 22.5). The physician, the patient, and the spouse observing the marker bubbles are instantly reassured of proper embryo placement. The extent of post-ET embryo migration in the uterus is still unclear [25, 26]. Shah et al. [27] recently demonstrated that the most important factor in obtaining high ET success rates was the actual performance of live ETs rather than practicing US-guided IUIs. Thus, how training in embryo transfer should be performed remains a controversy [3].


Fig. 22.5
Abdominal US with full bladder depicts two marker bubbles visualized in mid uterine cavity and confirming a perfect placement of embryos
Coaxial catheter US-guided ET approach involves initial placement of an outer catheter in the internal uterine os (Fig. 22.6). The outer catheter protects the inner catheter from mucus exposure and eliminates the need to renegotiate a deviated or a branching cervical canal. In this instance, time is not a limiting factor because the embryos are loaded into the inner catheter while the outer catheter is already in place. US will then allow ET time to be less than 30 s (Fig. 22.7). US guidance is extremely instructive at training facilities as it can provide feedback and reassurance to physicians in training. Coaxial live US guided ET allows teaching ET without a decline in the center’s PR.
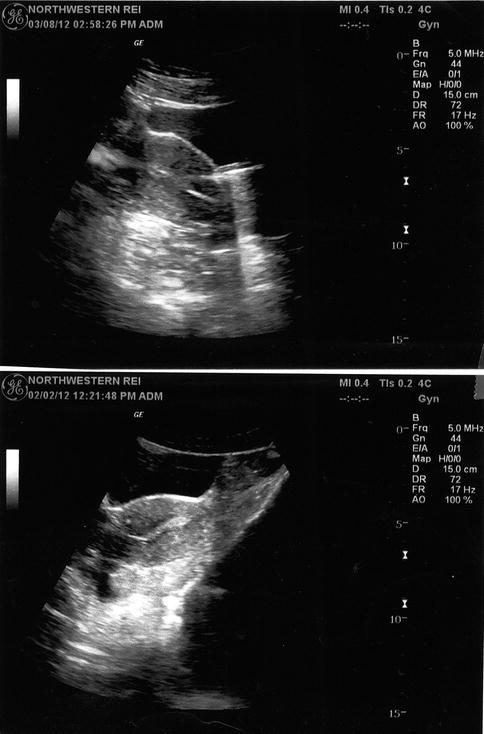
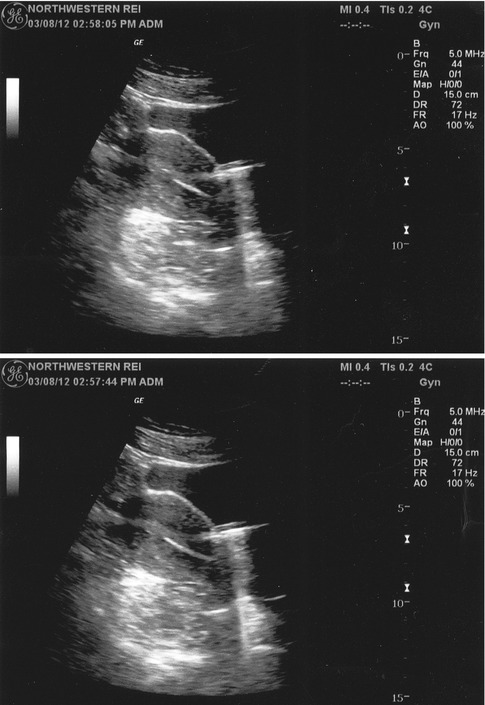
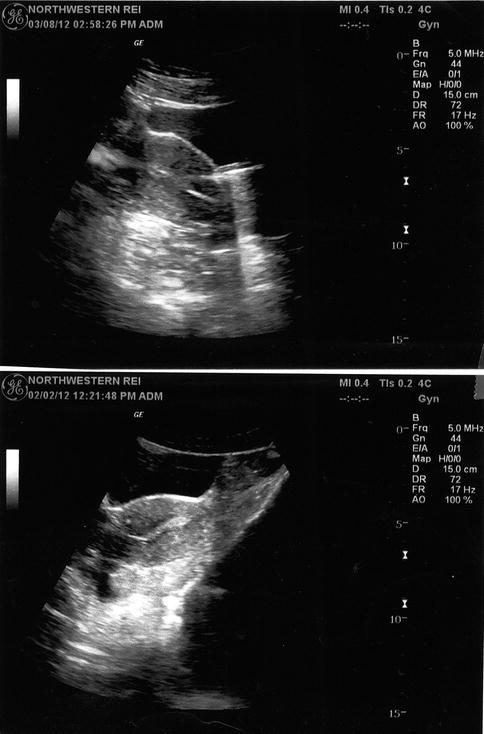
Fig. 22.6
Abdominal US depicts the external coaxial catheter wedged into the endometrium in an anteverted uterus (lower figure). Sliding a rehearsal inner catheter allows proper placement in the lower uterine segment (upper figure)
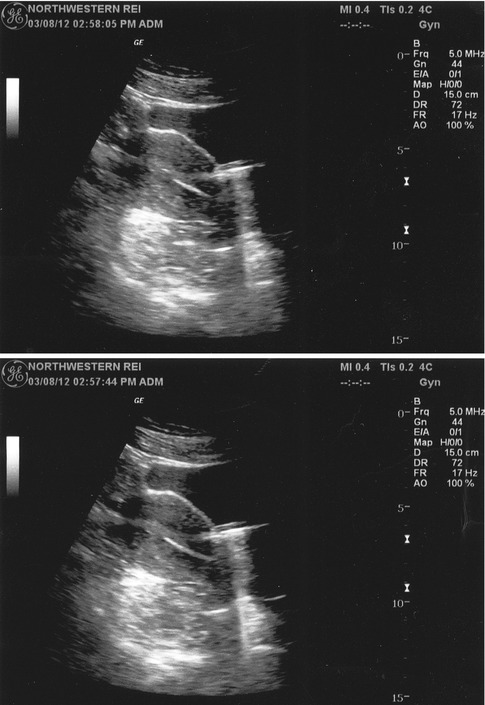
Fig. 22.7
Abdominal US demonstrates that the outer coaxial catheter is withdrawn leaving the inner soft embryo-loaded catheter at one cm from the uterine fundus (lower figure). Under live US observation, the embryo is injected and the marker bubble is observed in mid-cavity (upper figure)
Disadvantages of Ultrasound-Guided ET
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree