Trauma to the shoulder girdle is common throughout life, but the site of injury varies with age. In children and adolescents, fracture of the clavicle sustained during play or athletic activities is a frequent type of skeletal injury. Dislocations of the shoulder and acromioclavicular separation are often seen in the third and fourth decades of life, whereas fracture of the proximal humerus is commonly encountered in the elderly. Most of these traumatic conditions can be diagnosed on the basis of history and clinical examination, with radiographs obtained mainly to define the exact site, type, and extent of the injury. At times, however, as in posterior dislocation in the glenohumeral joint, for example, which is the most commonly missed diagnosis in shoulder trauma, only radiographic examination performed in the proper projections may reveal the abnormality.
Anatomic-Radiologic Considerations
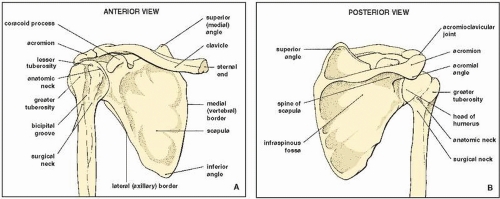
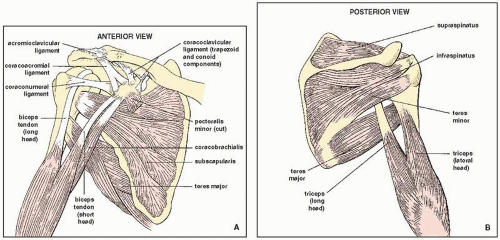
The shoulder girdle consists of osseous components—proximal humerus, scapula, and clavicle, forming the glenohumeral and acromioclavicular joints (
Fig. 5.1)—and various muscles, ligaments, and tendons reinforcing the joint capsule (
Fig. 5.2). The joint capsule inserts along the anatomic neck of the humerus and along the neck of the glenoid. In front, it is reinforced by three glenohumeral ligaments (GHLs) (the superior, middle, and inferior), which converge from the humerus to be attached by the long head of the biceps tendon to the supraglenoid tubercle. The other important ligaments are the acromioclavicular, coracoacromial, and the coracoclavicular (including trapezoid and conoid portions) (see
Fig. 5.2A).
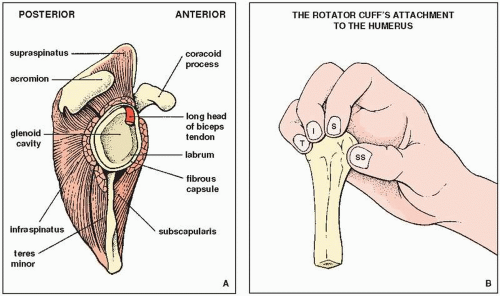
The essential muscles are those that form the rotator cuff (
Fig. 5.3). The term rotator cuff is used to describe the group of muscles that envelop the glenohumeral joint, holding the head of the humerus firmly in the glenoid fossa. They consist of the subscapularis anteriorly, the infraspinatus posterosuperiorly, the teres minor posteriorly, and the supraspinatus superiorly (mnemonic SITS). The subscapularis muscle inserts on the lesser tuberosity anteriorly. The insertions of the supraspinatus, infraspinatus, and teres minor muscles are on the greater tuberosity, posteriorly. The supraspinatus tendon covers the superior aspect of the humeral head, inserting on the superior facet of the greater tuberosity. The infraspinatus tendon covers the superior and posterior aspects of the humeral head and inserts on the middle facet, located distal and more posterior to the superior facet. The teres minor is lower in position and inserts on the posteroinferior facet of the greater tuberosity (
Fig. 5.3B). In addition, the long head of the biceps with its tendon, which in its intracapsular portion runs through the joint, and the triceps muscle, inserting on the infraglenoid tubercle inferiorly, provide additional support to the glenohumeral joint.
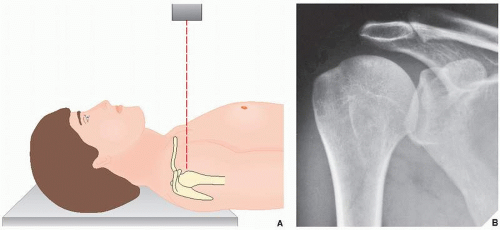
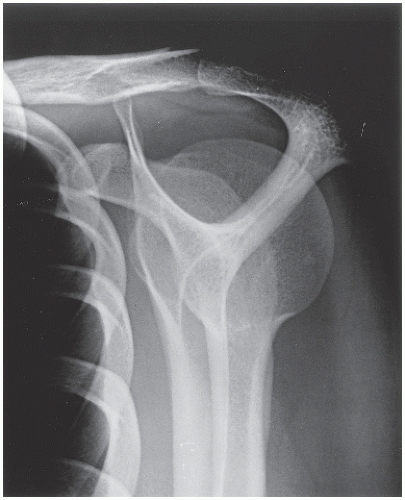
Most trauma to the shoulder area can be sufficiently evaluated on radiographs obtained in the
anteroposterior projection with the arm in the
neutral position (
Fig. 5.4A) or with the arm
internally or
externally rotated to visualize different aspects of the humeral head. The one limitation of these views is that the humeral head is seen overlapping the glenoid, thereby obscuring the glenohumeral joint space (
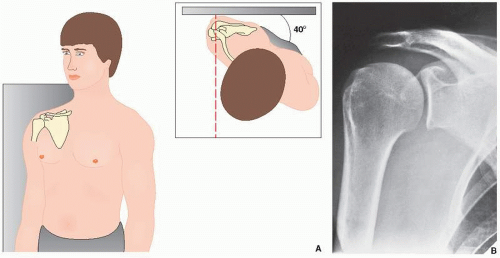
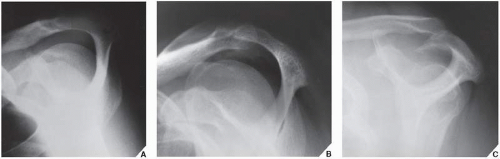
Fig. 5.4B). Eliminating the overlap can be accomplished by rotating the patient approximately 40 degrees toward the affected side. This special posterior oblique view, known as the
Grashey projection, permits the glenoid to be seen in profile (
Fig. 5.5) and is thus particularly effective in demonstrating suspected posterior dislocation. Obliteration of the normally clear space between the humeral head and the glenoid margin on this view confirms the diagnosis (see
Figs. 5.54 and
5.56).
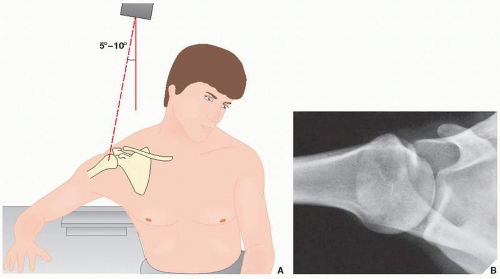
Other special views have proved to be useful in evaluating suspected trauma to various aspects of the shoulder. A superoinferior view of the shoulder, known as the
axillary projection, is helpful in determining the exact relationship of the humeral head and the glenoid fossa (
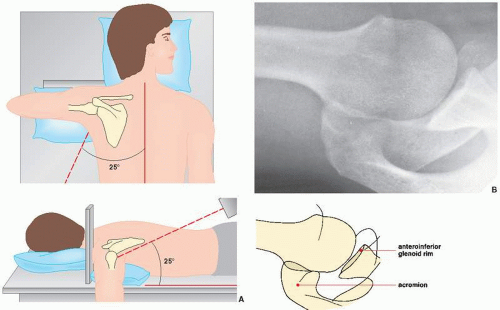
Fig. 5.6), as well as in detecting anterior or posterior dislocation. This view, however, may at times be difficult to obtain, particularly if the patient is unable to abduct the arm, in which case a variant of the axillary projection known as the
West Point view may be similarly effective. In addition to all the benefits of the axillary projection, the West Point view effectively demonstrates the anteroinferior rim of the glenoid (
Fig. 5.7). Another useful variant of the axillary projection is the
Lawrence view. The importance of this projection lies in the fact that it does not require full abduction of the arm, because it can be compensated for by angulation of the radiographic tube (
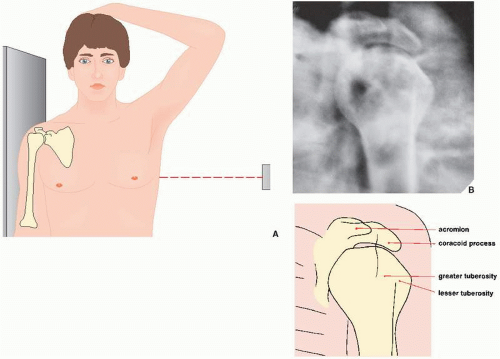
Fig. 5.8). Suspected trauma to the proximal humerus, which can be demonstrated on the anteroposterior or the transscapular projection (see
Fig. 5.12), may require the
transthoracic lateral view for sufficient evaluation (
Fig. 5.9). Because this projection provides a true lateral view of the proximal humerus, it is particularly valuable in determining the degree of displacement or angulation of the osseous fragments (see
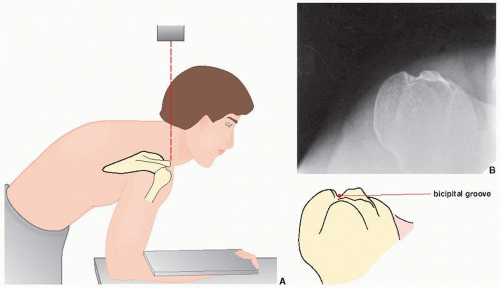
Fig. 5.28B). When trauma to the bicipital groove is suspected, a
tangent radiograph of this structure is required (
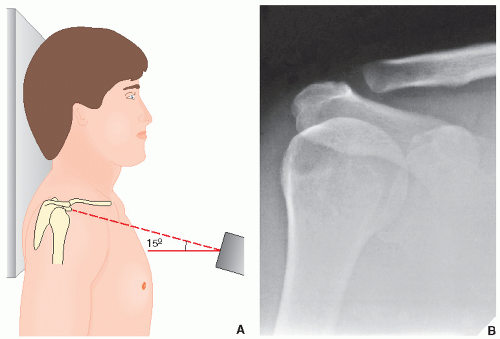
Fig. 5.10). Injury to the acromioclavicular articulation is usually evaluated on the anteroposterior view obtained with a 15-degree cephalad tilt of the radiographic tube (
Fig. 5.11). Stress views in this projection, for which weights are
strapped to the patient’s forearms, are often mandatory, especially in suspected occult acromioclavicular subluxation (see
Fig. 5.78). Fracture of the scapula may require a
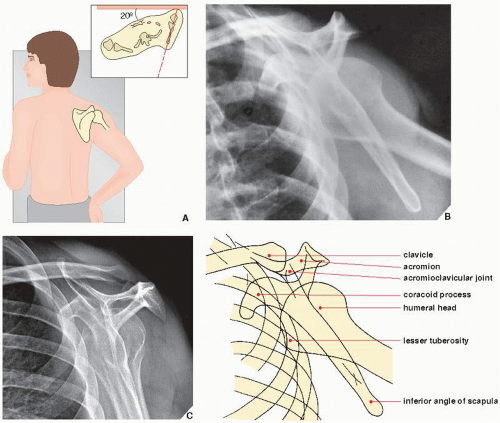
transscapular (or
Y) view for sufficient evaluation (
Fig. 5.12). Fracture of the acromion can be adequately evaluated on the shoulder
outlet view. This projection is obtained similarly to the Y view of the shoulder girdle; however, the central beam is directed toward the superior aspect of the humeral head and is angled approximately 10 to 15 degrees caudad (
Fig. 5.13). This view is also effective in demonstration of morphologic types of the acromion (
Fig. 5.14; see also
Fig. 5.24).
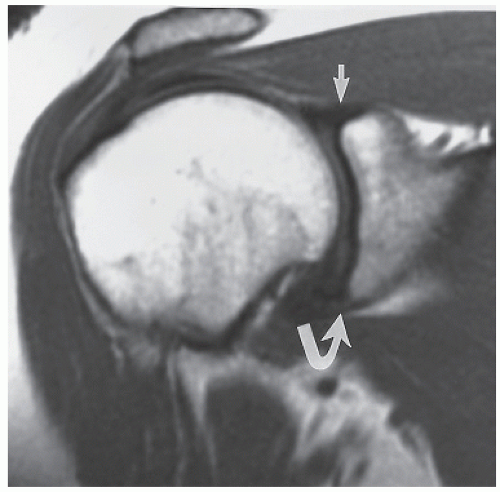
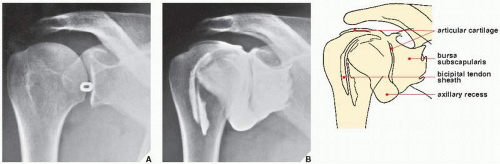
Ancillary imaging techniques are usually used to evaluate injury to the cartilage and soft tissues of the shoulder. The most frequently used modalities are arthrography and magnetic resonance imaging (MRI). Arthrography can be performed using a single- or double-contrast technique (
Fig. 5.15). In cases of suspected tear of the rotator cuff, for example, a single-contrast arthrogram may reveal abnormal communication between the glenohumeral joint cavity and the subacromial-subdeltoid bursae complex, which is diagnostic of this abnormality (see
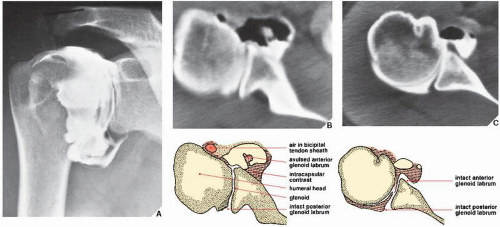
Fig. 5.60C). Although it is difficult to prescribe for which conditions a single- as opposed to a double-contrast study should be chosen, the latter may be better suited to demonstrate abnormalities of the articular cartilage and capsule, as well as the presence of osteochondral bodies in the joint. A double-contrast study, however, is always indicated when arthrography is to be combined with CT scan (computed arthrotomography) for evaluating suspected abnormalities of the fibrocartilaginous glenoid labrum (
Fig. 5.16). The effectiveness of this combination lies in the fact that the injected air outlines the
anterior and posterior labrum for better demonstration of subtle traumatic changes on CT images. For this study, the patient is placed supine in the CT scanner with the arm of the affected side in the neutral position to allow the air to rise and enhance the outline of the anterior labrum. To evaluate the posterior labrum, the arm is externally rotated (or the patient is positioned prone) to force the air to move posteriorly.
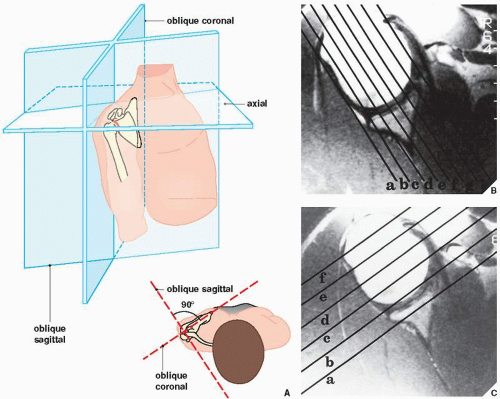
Recent studies have shown the considerable advantage of MRI in the examination of the shoulder. This modality is particularly effective in demonstrating traumatic abnormalities of the soft tissues, such as impingement syndrome, partial and complete rotator cuff tears, biceps tendon rupture, glenoid labrum tears, and demonstration of the traumatic joint effusion. However, the shoulder presents unique difficulties for imaging. Because of space limitations in the magnet, the shoulder frequently cannot be positioned in the center of the magnetic field. This necessitates lateral shift for image centering and scanning a region where the signal-to-noise ratio is relatively low. These problems have been overcome by combining high-resolution scanning with the use of special surface coils. Because the bones and muscles of the shoulder girdle are oriented along multiple nonorthogonal axes, scanning in oblique planes is more effective.
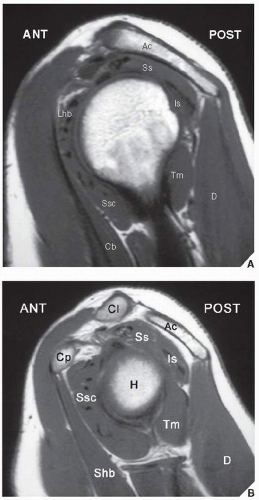
The patient should be positioned in the magnet supine with the arms along the thorax and the affected arm externally rotated. The scanning planes include oblique coronal (along the long axis of the belly of the supraspinatus muscle), oblique sagittal (perpendicular to the course of supraspinatus muscle), and axial (
Fig. 5.17). The first two planes are ideal for evaluating all the structures of the rotator cuff; the axial plane is ideal for evaluating the glenoid labrum, bicipital groove, biceps tendon, and subscapularis tendon. Appropriate pulse sequences are critical in displaying normal anatomy and traumatic abnormalities. T1-weighted pulse sequences sufficiently demonstrate the structural anatomy (
Figs. 5.18 and
5.19). Proton density and T2-weighted pulse sequences provide the information necessary to evaluate pathology of rotator cuff, joint space, and bones (see
Figs. 5.62,
5.63,
5.64B, and
5.65).
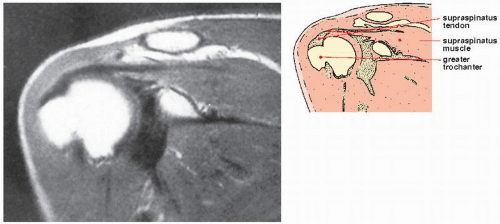
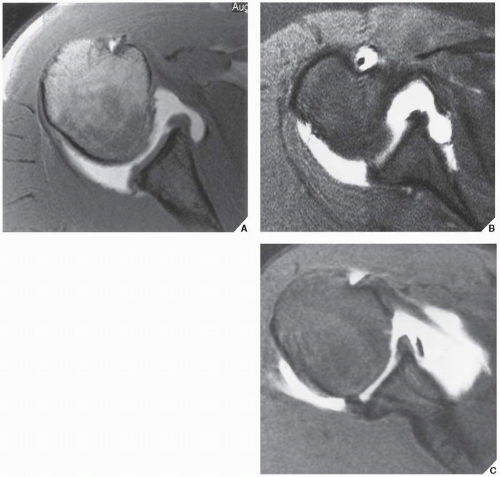
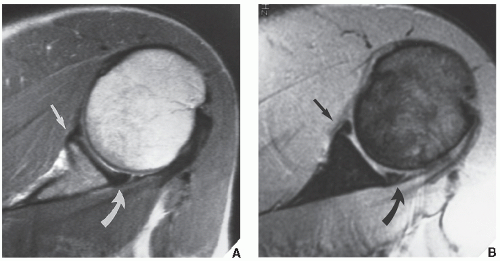
The demonstration of rotator cuff muscles and tendons is greatly facilitated by the use of MRI. The supraspinatus is best demonstrated on oblique coronal and sagittal images, preferably obtained on spin-echo T1-weighted sequences. It is seen as a thick, intermediate-intensity structure, and its tendon inserts on the superolateral aspect of the greater tuberosity of the humerus (
Fig. 5.18, see also
Fig. 5.26). The infraspinatus and subscapularis are best demonstrated on axial images as fusiform, intermediate-intensity structures. The infraspinatus tendon inserts distally and more posterior to the supraspinatus on the greater tuberosity, adjacent to the insertion of teres minor (see
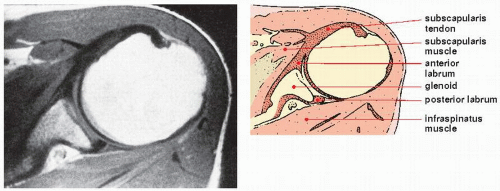
Fig. 5.26). The subscapularis muscle is located anterior to the body of the scapula. It appears on T1-weighted axial images as an intermediate-intensity structure that tapers anteriorly into a low-intensity tendon, where it merges with the anterior aspect of the capsule before inserting on the lesser tuberosity (
Fig. 5.19, see also
Fig. 5.26).
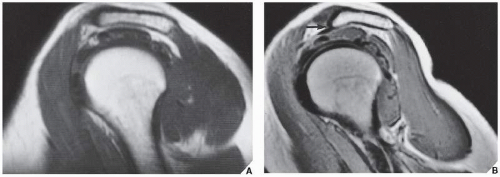
The axial images are effective in demonstration of the joint capsule, which is anteriorly reinforced by the anterior GHLs. The capsular complex provides stabilization of the glenohumeral joint. The anterior capsular complex includes the fibrous capsule, the anterior GHLs, the synovial membrane and its recesses, the fibrous glenoid labrum, the subscapularis muscle and tendon, and the scapular periosteum. Three types of anterior capsular insertion have been identified by Zlatkin and colleagues. They are determined by the proximity of insertion to the glenoid margin (
Fig. 5.20). In type I, the capsule inserts on the glenoid rim in close proximity to the glenoid labrum. In types II and III, the capsular insertion is further away from the glenoid rim and may reach the scapular neck (
Fig. 5.21). The further the anterior capsule inserts from the glenoid margin, the more unstable the glenohumeral joint will be. The posterior portion of the capsule shows no variations and attaches directly to the labrum. The axial images are also effective in the demonstration of anterior and posterior cartilaginous labrum of the glenoid, which are seen as two small triangles of low signal intensity that are located anteriorly and posteriorly to the glenoid margin (
Fig. 5.22). The superior and inferior aspects of the labrum are best demonstrated on
the oblique coronal sections (
Fig. 5.23). There are numerous imaging variations of the morphology of the cartilaginous labrum. The most common shape is triangular as illustrated in
Figure 5.22. The second most common shape is round. The other morphologic variations include the flat labrum and the cleaved or notched labrum. On rare occasions, the anterior and posterior labrum may be absent. Furthermore, there are appearances resembling labral tears, such as undercutting of the labrum by hyaline cartilage, sublabral holes or recesses, and Buford complexes (see
Fig. 5.74).
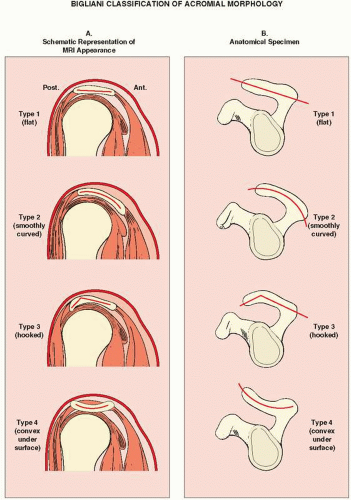
The sagittal images are useful in demonstration of morphologic variations of the acromion. Three types of acromion have been identified by Bigliani and coworkers. Type I shows a flat undersurface, type II a curved undersurface, type III a hooked undersurface, and type IV a convex undersurface (
Figs. 5.24 and
5.25). Type III acromion is considered to be associated with tears of the rotator cuff proximal to the site of insertion of the supraspinatus tendon to the greater tuberosity of the humerus. Sagittal images also effectively demonstrate the muscles of the rotator cuff and their tendons (
Fig. 5.26).
In the past decade, direct MR arthrography (MRa) using injection of contrast solution into the shoulder joint gained worldwide acceptance. This technique is particularly effective for demonstrating labral-ligamentous abnormalities and distinguishing partial-thickness from full-thickness tears of the rotator cuff. A variety of concentrations and mixtures of solutions are used by different radiologists. In our institution, we follow the recommendation reported by Steinbach and colleagues. We add 0.8 mL of gadopentetate dimeglumine (gadolinium with strength 287 mg/mL) to 100 mL of normal saline solution. Subsequently, we mix 10 mL of this solution with 5 mL of 60% meglumine diatrizoate (iodinated contrast) and 5 mL of 1% lidocaine, which gives a final gadolinium dilution ratio of 1:250. From 12 to 15 mL of this mixture is then injected into the shoulder joint using fluoroscopic guidance in a similar fashion as for conventional shoulder arthrography (see
Fig. 5.15). Multiple pre-exercise and postexercise radiographic spot images are obtained in neutral position and in external and internal rotation of the arm. Subsequently, without delay, the patient undergoes MRI examination using similar scanning planes as for a conventional MR study. If glenoid labrum abnormalities are suspected, additional sequences are obtained in so-called ABER (abduction and external rotation) position.
During evaluation of MRI of the shoulder, it is helpful to use a checklist as provided in
Table 5.1.