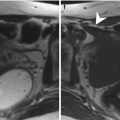
Fig. 3.1
Normal cervical anatomy. (a, b) T2w TSE images in axial (TR 5,130 ms, TE 108 ms) and sagittal (TR 6,040 ms, TE 90 ms) orientation showing the normal appearance of the cervical anatomy at MRI: endocervix (asterisk), inner stromal ring (black arrowhead) and outer cervical stroma (S). Parametrial tissue (P). Urinary bladder (B)
The central endocervical mucosa shows high signal intensity on T2-weighted images, due to the presence of cervical mucus, particularly during the periovulatory phase. During menopausal age, the cervical epithelium atrophies and the production of mucus diminishes; consequently the thickness and the signal intensity of the endocervical mucosa is reduced [4].
The middle layer corresponds to the inner layer of fibromuscular cervical stroma, which is often contiguous to the junctional zone of the uterine corpus. It is characterized by low signal intensity on T2-weighted images, due to the large amount of fibroblasts and smooth muscle cells and less vascularized connective tissue compared to the outer cervical stroma.
The outer layer of the cervix, corresponding to the outer cervical stroma, has low to intermediate signal intensity on T2-weighted images, due to the lower concentration of smooth muscle cells; it is often contiguous to the outer myometrium [5].
On unenhanced T1-weighted images, the cervix appears as a homogeneous cylinder-shaped structure of intermediate signal intensity; the single layers are not distinguishable.
After endovenous administration of contrast agent, both endocervical epithelium and parametrium show rapid contrast enhancement, followed by a progressive increase of the signal intensity of the outer stroma, whereas the compact stroma of the intermediate layer remains hypointense.
The paracervical tissue is composed of less dense stroma; consequently it has moderate to high signal intensity on T2-weighted images, whereas it demonstrates intermediate signal intensity on T1-weighted images.
3.3 Imaging Technique
3.3.1 Patient Preparation
Before scanning it is important to gather the gynaecologic anamnesis of the patient with information about her symptoms, hormonal status, menstrual cycle, eventual hormone therapy, pregnancies, previous surgery or chemoradiotherapy.
A 4-h fasting is required for contrast medium injection and for reduction of bowel peristalsis. Motion artefacts caused by peristalsis are also reduced by the administration of a spasmolytic agent, such as butyl scopolamine bromide (Buscopan) administered preferentially intramuscularly at a dose of 20 mg few minutes before scanning (in alternative: glucagon 2 mg endovenously).
The urinary bladder should be moderately filled in order to straighten an anteflexed uterus.
If vaginal infiltration is suspected, it would be helpful to distend the vagina with gel for better delineation of the fornices.
The application of contrast medium is usually not necessary, apart from selected cases, in which a low molecular paramagnetic gadolinium-based contrast agent is administered at a dose of 0.5–1 mmol/kg body weight.
3.3.2 Patient Positioning, Scan Planes and Sequences
The patient is positioned supine with the arms lying along her sides.
The use of body phased array surface coils, covering from mid symphysis pubis to renal hilum, is important in order to obtain a high signal to noise ratio, high signal homogeneity, high spatial resolution and rapid acquisitions. A relative disadvantage is that subcutaneous fat shows high signal intensity, which may accentuate motion artefacts in sequences obtained without breath hold. Thus, it is important to employ presaturation bands, anteriorly and above to the region of interest, in order to reduce the signal from the moving abdominal wall. Other strategies to reduce motion artefacts are respiratory triggering or breath-hold acquisitions with very fast sequences, large measurements and the correct phase encoding direction.
The imaging area must comprehend not only the pelvis but also the abdomen up to the renal hilum for the evaluation of para-aortic lymph nodes.
The best sequences for the depiction of cervical carcinoma are turbo spin echo (TSE) T2-weighted sequences without fat saturation, which are characterized by high soft tissue contrast. They are first acquired in the sagittal plane, parallel to the long uterine axis (covering the uterus and vagina to the pelvic floor), then parallel to the short axis of the cervical canal (from the fundus uteri to the pelvic floor) and finally perpendicularly to this, parallel to the long axis of the cervical canal (Fig. 3.2).
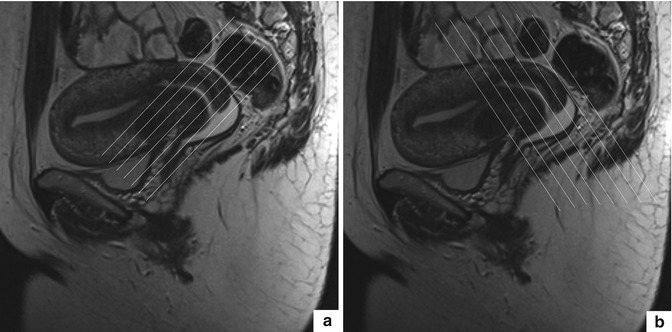
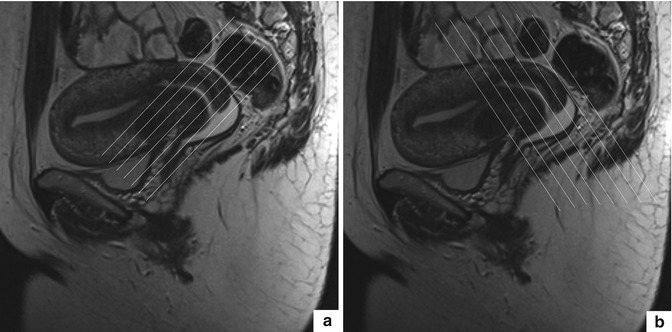
Fig. 3.2
T2w TSE images in sagittal orientation (TR 6,040 ms, TE 90 ms). Example for positioning of the imaging slices in an MRI cervical examination along the short (a) and long (b) axis of the uterine cervix
Angulated images are important for the optimal depiction of the cervical stromal ring (axial planes) and for the evaluation of the relationship of the cervix with contiguous structures: axial and coronal planes and in particular the coronal planes parallel to the long axis of the endocervical canal. Additional angulated images perpendicular to the uterus or vagina may be useful in suspected infiltration of these structures.
Lymph node metastases are best evaluated with high-resolution respiratory-triggered T2 axial sequences, which are also useful in case of ureteral involvement.
DWI-weighted sequences may also be helpful in the detection of the cervical cancer itself, lymph node metastases and the peritoneal dissemination of tumours, as their ADC values are lower than those of normal tissues.
Intravenous contrast medium injection is usually not necessary, neither in benign lesions nor in primary staging of cervical cancer, which, at T2-weighted images, is usually well delineated from the surrounding tissue.
The administration of contrast material agents instead is helpful if cervical cancer is not seen at T2-weighted sequences and in patient candidates to trachelectomy. The injection of contrast agents may be useful even in those conditions, in cases where rectal, urinary bladder or vaginal infiltration by the tumour or endometriosis is suspected or in the differentiation between tumour recurrence and inflammatory, post-actinic or postoperative changes at follow-up examinations.
3.3.3 Standard Protocol for the Cervix Study at 1.5 T
Table 3.1.
Table 3.1
Standard protocol for the cervix study at 1.5 T
Orientation | TR ms | TE ms | ST mm | FOV cm | Matrix px | Imaging area | Rationale | |
|---|---|---|---|---|---|---|---|---|
T2w TSE | True axial (Short cervical axis) | 5,130 | 108 | 4 | 320 | 320 × 85 | Pelvis | Evaluation of stromal ring integrity and cervical infiltration |
T2w TSE | True sagittal (Long uterine axis) | 6,040 | 90 | 3 | 330 | 448 × 80 | Pelvis | Evaluation of vaginal invasion |
T2w TSE | True coronal (Long cervical axis) | 3,870 | 101 | 3 | 320 | 320 × 65 | Pelvis | Evaluation of parametrial pelvic floor infiltration |
T1w SE | Axial | 550 | 9.3 | 4 | 320 | 256 × 80 | Kidneys to pelvis | Evaluation of pelvic floor muscles |
T2w BH | Axial | 5.65 | 2.83 | 3 | 380 | 512 × 80 | Kidneys to pelvis | Evaluation of lymph nodes and ureters |
TRUE-FISP |
3.3.4 Optional Protocol for the Cervix Study at 1.5 T
Table 3.2.
Table 3.2
Optional protocol for the cervix study at 1.5 T
Orientation | TR ms | TE ms | ST mm | FOV cm | Matrix px | Imaging area | Rationale | |
|---|---|---|---|---|---|---|---|---|
T1w SE FS | Axial | 550 | 9.3 | 4 | 320 | 256 × 80 | Kidneys to pelvis | Evaluation of tumour, therapy complications and fistulas |
Pre-post Gd | Coronal | |||||||
Sagittal | ||||||||
T1w 3D GRE FS | Volumetric | 4.89 | 2.4 | 2.5 | 400 | 320 × 80 | Kidneys to pelvis | Evaluation of tumour and therapy complications |
Pre-post Gd | ||||||||
DWI EPI FS | Axial | 2,100 | 81 | 7 | 400 | 144 × 100 | Kidneys to pelvis | Evaluation of tumour |
b 0–500-1,000 (s/mm2) | Sagittal | |||||||
T1w GRE FS | Axial | 822 | 4.93 | 4 | 320 | 256 × 91 | Pelvis | Evaluation of cervical endometriosis |
3.4 Non-neoplastic Diseases
3.4.1 Cervical Pregnancy
Cervical pregnancy is rare, occurring in 0.15 % of ectopic pregnancies [6]. Anyway, its incidence is increasing, probably due to the more frequent abortions. The causative process for cervical pregnancy is still not well comprehended. Well-known risk factors include uterine and cervix surgery, leiomyoma, anatomic malformations such as uterus septate, atrophic endometrium and multiparity. It is a painless condition manifesting as bleeding after a period of amenorrhea. At the physical examination findings consist of an enlarged cervix with a dilated cervical external ostium [7].
At MRI the mass, made of decidua and chorionic villa with variable amount of blood at different stages of degradation, shows heterogeneous signal on both T1- and T2-weighted sequences with a low-signal-intensity margin on T2-weighted images and variable contrast enhancement after administration of gadolinium-based contrast material [3, 8]
3.4.2 Uterine Cervicitis
The ectocervix and the endocervix are, respectively, lined by squamous and columnar (glandular) epithelium and are therefore affected by different pathogens including Trichomonas vaginalis, Candida albicans and herpes simplex virus (mostly HSV type 2), which invade the ectocervical squamous epithelium, and Neisseria gonorrhoeae and Chlamydia trachomatis which affect the glandular endocervical epithelium causing mucopurulent infections [3, 7, 8].
Clinical manifestations of acute cervicitis are tenacious, jelly-like, yellow or turbid vaginal discharge, sensation of pelvic pressure or discomfort. Chronic inflammation instead may be completely asymptomatic but may cause epithelial erosion followed by atypical reparation processes with formation of retention cysts, which are demonstrated at MRI with low signal intensity on T1- and high signal intensity on T2-weighted sequences without enhancement after gadolinium-based contrast material administration [3, 8].
3.4.3 Nabothian Cysts
Nabothian cysts are a common finding in the cervix and represent mucous retention cysts localized in the deep cervical glandular epithelium caused by proliferation of the squamous epithelium in response to chronic flogosis with obstruction of the crypts, which consequently fill with mucus secreted by the columnar epithelium [3, 7, 9].
A subtype of nabothian cysts are the so-called tunnel clusters which are characterized by multicystic dilatation of the endocervical glands. They can be found in about 8 % of adult women, 40 % of whom are pregnant, almost exclusively multigravida and older than 30 years. Therefore, tunnel cluster seems to be the result of a stimulatory process occurring during pregnancy [8, 9].
Nabothian cysts are usually discovered incidentally, measuring from few millimetres to several centimetres and can easily be evaluated by visual inspection. Large cysts in the deeper cervical stroma may cause an unexplained enlargement of the cervix [8].
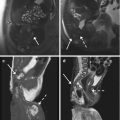
At MRI they appear as single or multiple circumscribed superficial round- to oval-shaped lesions with smooth margins. Their proteinaceous content determines the intermediate or slightly high signal intensity on T1-weighted sequences and the prominent homogeneous high signal intensity on T2-weighted images. There is no enhancement after administration of intravenous contrast material [3, 8–10] (Fig. 3.3).
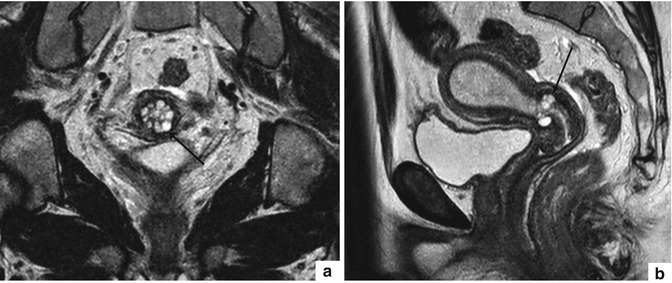
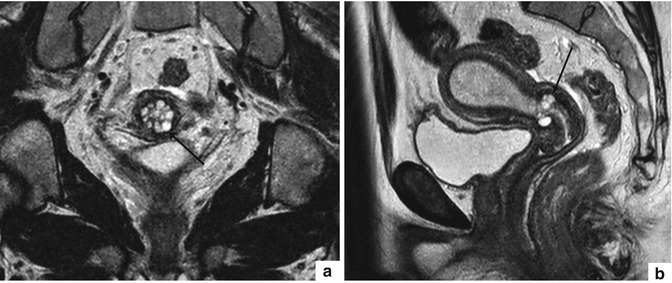
Fig. 3.3
Nabothian cysts. T2w TSE images in coronal (TR 3,870 ms, TE 101 ms) (a) and sagittal (TR 6,040 ms, TE 90 ms) (b) orientation showing multiple, round- to oval-shaped, well-circumscribed, hyperintense cystic formations (arrow)
The most important differential diagnosis consists in adenoma malignum, a well-differentiated adenocarcinoma of the cervix associated with cystic portions. The presence of solid tissue between the cysts suggests the malignant nature of this lesion [3].
3.4.4 Cervical Polyps
Cervical polyps are the most common benign lesions of the cervix and are due to inflammatory and metaplastic processes occurring above all in the endocervical canal. They may range in size from a few millimetre sessile lesions to huge pedicled masses of 5 cm, protruding through the cervical orifice. They are soft masses arising from the mucosa and made of loose fibromyxoid connective stroma, blood vessels and dilated glands. Malignant degeneration is uncommon [3, 7].
They typically occur in perimenopausal women (especially in the fifth decade). The presenting symptoms include menorrhagia, intermenstrual or postmenopausal vaginal bleeding, contact bleeding and vaginal discharge. The diagnosis is made by hysteroscopy [3, 8].
At MRI cervical polyps are depicted as heterogeneous intermediate to high-signal-intensity masses with a hypointense central fibrous core and intratumoural cysts. After contrast medium injection the mass frequently shows a delayed lattice-like enhancement with outlining of the cystic spaces [3, 6, 8].
3.4.5 Endometriosis
Cervical endometriosis is rare and usually affects the endocervical canal or the portio. The retrocervical region and the posterior fornices instead are frequently affected by deeply infiltrating endometriosis with associated alterations of the uterosacral ligaments at their cervical insertions [3, 8].
The solid components of endometriosis, consisting of predominant muscular hyperplasia with associated fibrosis surrounding foci of endometrial tissue, show low signal intensity on both T1- and T2-weighted sequences and show pronounced contrast enhancement after contrast medium injection. These lesions usually contain haemorrhagic material which gives rise to the development of cystic components with high T1-signal intensity and variable T2-signal intensity [3] (Fig. 3.4).
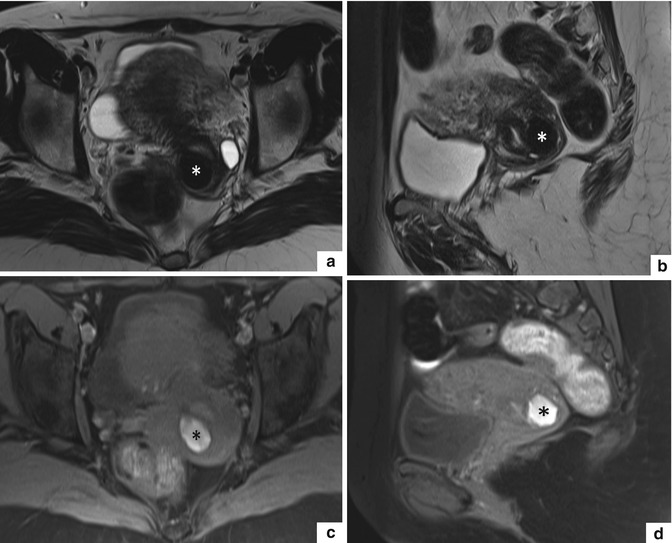
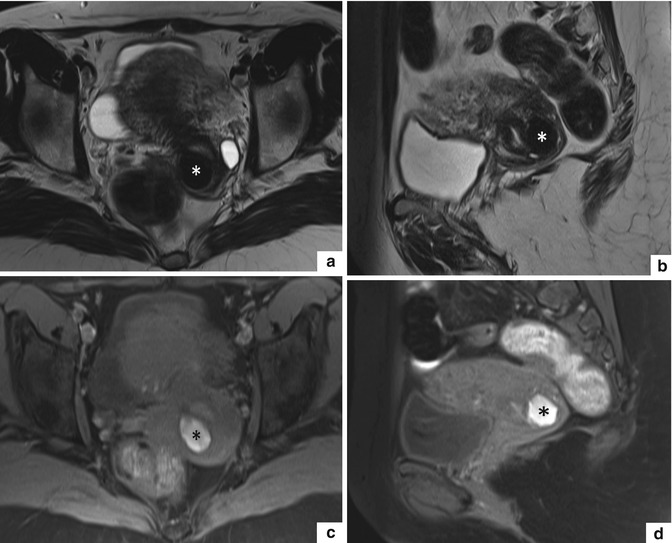
Fig. 3.4
Endometriosic cyst with haemorrhagic content in the posterior outer cervical stroma. T2w TSE images in axial (TR 5,130 ms, TE 108 ms) (a) and sagittal orientation (TR 6,040 ms, TE 90 ms) (b) and T1w TSE FS images in axial (TR 660 TE 9.5) (c) and sagittal orientation (TR 660, TE 9.5) (d) show a round-shaped, well-defined cystic lesion (asterisk) in the posterior outer cervical stroma. Its content shows low signal intensity on T2w TSE images (a, b) and high signal intensity on T1w TSE FS images (c, d), due to the presence of intracystic haemorrhagic material
More often it happens that an adenomyosic polypoid mass of the corpus uterine, covered by endometrial mucosa and smooth muscle layers resembling myometrium, protrudes into the cervical canal; it appears as ill-defined hypointense mass with some hyperintense cystic spots on T2-weighted images [3, 11].
3.5 Epithelial Neoplasms
3.5.1 Cervical Cancer
3.5.1.1 Introduction
Cervical cancer represents the second most common malignancy in women after breast cancer, is the most common malignant pathology affecting the female genital tract and one of the most frequent causes of death in women [4, 8, 12, 13]. The average age at diagnosis is 30–50 years, with a first peak between 35 and 45 years and a second one between 65 and 75 years [14–16].
In most cases, cervical cancer is due to the infection of the cervical epithelium by oncogenic human papillomaviruses (HPV), in particular HPV 16 and 18, which represent the high-risk types. Thus, there are many other risk factors for developing cervical carcinoma, i.e. sex at an early age, many different sexual partners, poor genital hygiene, frequent other genital infections, multiple pregnancies, immunosuppression and long-term use of oral contraceptives [3].
Typically these tumours arise from the unstable transformation zone of the uterine cervix at the junction of the squamous epithelium of the portio and the columnar epithelium of the cervical canal. Eighty to ninety percent of these tumours are squamous cell carcinomas followed by adenocarcinomas (5–10 %). Other rare histologic types of cervical cancer include adenosquamous carcinomas, small cell carcinomas and neuroendocrine tumours [3, 8, 17].
In early stages, cervical carcinomas are frequently asymptomatic. They become evident when the tumour has reached the stage of an invasive ulcerating cancer and are mainly represented by irregular or heavy vaginal bleeding, postcoital bleeding. Some patients present with a watery, mucoid, or purulent and malodorous vaginal discharge, which is a nonspecific finding. Advanced cervical tumour presents with pelvic and back pain due to infiltration of the adjacent anatomic structures, unilateral oedema of the leg caused by disturbance of the lymphatic drainage and increase in body circumference in case of peritoneal seeding [3]. Anyway, nowadays most cervical cancers are discovered in an early stage thanks to screening programmes with Pap test.
The final diagnosis of carcinoma of the uterine cervix is based upon histologic evaluation of a cervical biopsy.
3.5.1.2 Roles of MR Imaging
MRI is the method of choice for pretreatment evaluation of tumour extent in patients with FIGO stage IB or greater (stage 0 and IA cannot be assessed with this imaging method), giving important information about:
Tumour volume
Depth of stromal invasion
Extension into the lower uterine segment
Involvement of other contiguous anatomic structures and lymph nodes
3.5.1.3 General Appearance of Cervical Cancer on MRI
Cervical carcinoma can demonstrate a wide variety of morphologic appearances and may be endocervical with a barrel shape or exophytic infiltrating [19].
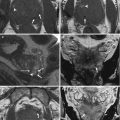
Cervical tumours are best seen on T2-weighted MRI images as they show a high soft tissue contrast resolution and allow better differentiation of the tumour from the normal fibrocervical stroma, the surrounding tissues and organs. In fact, cervical cancer usually develops as a focal lesion from the mucosal layer of the cervix with a higher signal intensity on T2-weighted sequences in comparison to the low-signal-intensity cervical stroma [3, 14, 17, 18] (Fig. 3.5a, b).
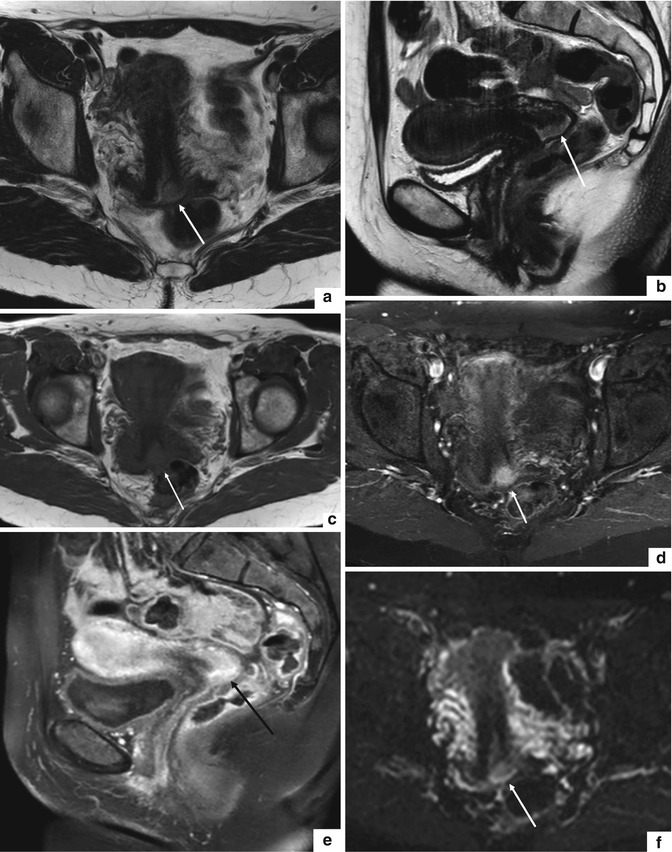
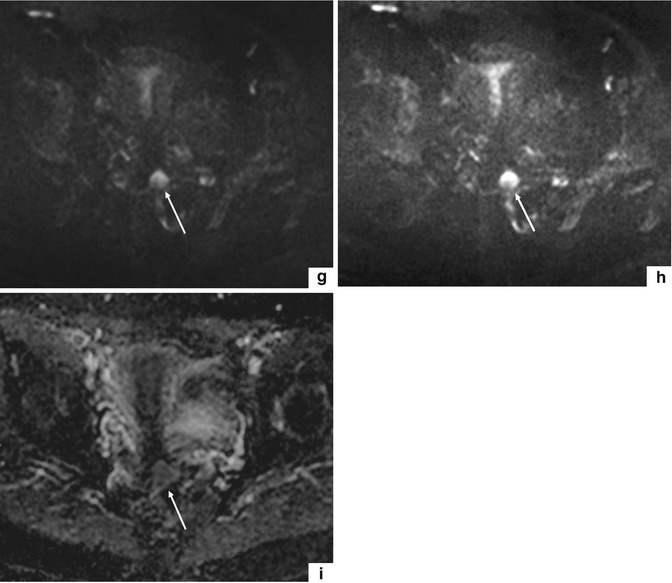
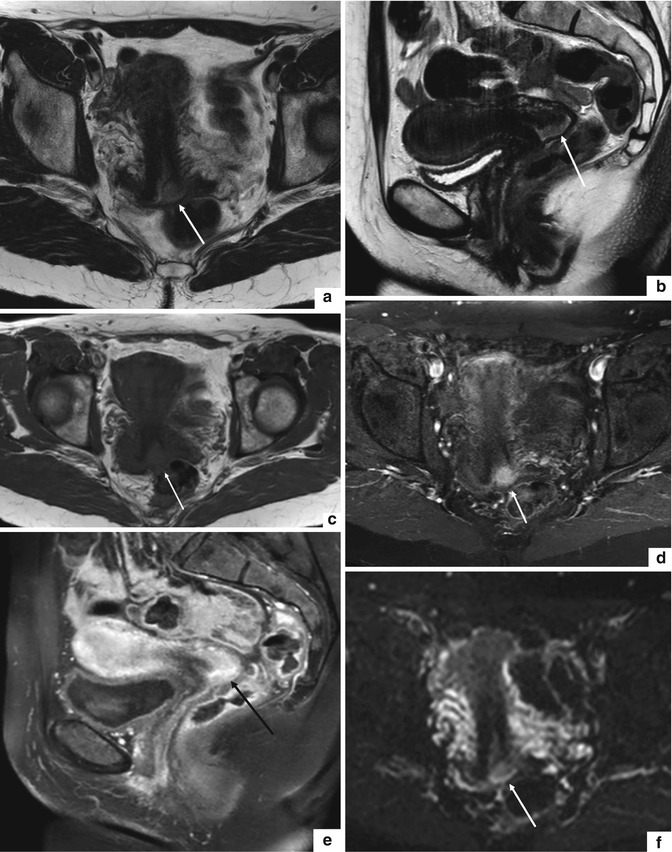
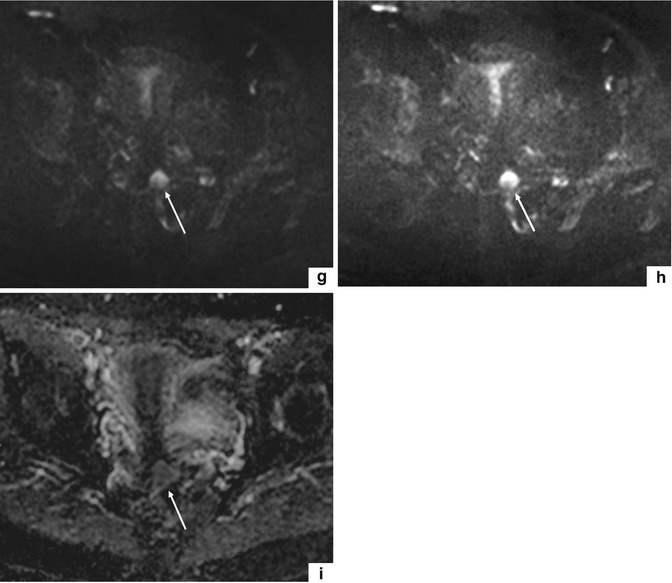
Fig. 3.5
Cervical cancer (FIGO stage IB1). T2w TSE images in axial (TR 5,130 ms, TE 108 ms) (a) and sagittal (TR 6,040 ms, TE 90 ms) (b) orientation show an area of high signal intensity in the left posterior portion of the uterine cervix attributable to cervical cancer (arrows). On T1w TSE image in axial orientation (TR 550 ms, TE 9.3 ms) (c), the tumour (arrow) is represented by an area of altered signal intensity which results nearly isointense to the signal intensity of the outer cervical stroma. T1w TSE FS images after administration of contrast material (TR 4.89 ms, TE 2.4 ms) in axial (d) and sagittal orientation (e) show a marked enhancement of the neoplastic process (arrows). Furthermore, on diffusion-weighted images (TR 2,100 ms, TE 81 ms) with B0 (f), B150 (g) and B300 (h) values, the pathological process demonstrates a progressive increase of signal intensity (arrows). On the ADC map (i), the tumoural process shows low signal intensity
On T1-weighted images, cervical cancer is usually isointense to the cervical stroma, and its identification is much more difficult compared to T2-weighted images. These sequences, instead, permit a better depiction of the parametrial tissue infiltration, since this tissue contains more fat and therefore shows a high signal intensity while the tumour itself presents a low signal intensity. T1-weighted sequences are used furthermore for the staging of lymph nodes [3] (Fig. 3.5c).
In those particular cases where gadolinium-based contrast medium is applied (patients with positive histological outcome for cervical cancer but the tumour is not detectable on T2-weighted images or patients candidate for trachelectomy), cervical carcinomas show an early enhancement within the first 15–30 s. Small tumours enhance homogeneously while large tumours often present necrotic changes and may or may not enhance. Anyway, they are often surrounded by an enhancing rim [3, 14, 17] (Fig. 3.5d, e).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree