and Jurgen J. Fütterer2, 3
(1)
Department of Radiological Sciences, Oncology and Pathology, Sapienza University of Rome, Rome, Italy
(2)
Department of Radiology and Nuclear Medicine, Radboudumc, Nijmegen, The Netherlands
(3)
MIRA Institute for Biomedical Technology and Technical Medicine, University of Twente, Enschede, The Netherlands
Vulvar Cancer
Vulvar carcinoma is a rare disease, which predominantly involves older women.
The prognosis of vulvar carcinoma is related to the extent of the primary tumor and lymph node involvement.
Squamous cell carcinoma accounts for approximately 80–90 % of vaginal malignancies.
The main risk factor is infection with human papillomavirus (HPV).
A clear cell carcinoma of the vagina is a rare cancer and often linked to exposure to diethylstilbestrol (DES). These tumors range from polypoid to infiltrating. Imaging has a limited role in their diagnosis, but MR is useful in assessing spread.
Primary vaginal clear cell carcinoma not associated with DES is very rare.
Vaginal Sarcoma
Vaginal sarcomas account for 2 % of vaginal malignancies.
Vaginal rhabdomyosarcomas are found almost exclusively in young children.
Vaginal leiomyosarcoma is the most common sarcoma in adolescents and women.
MR imaging is limited in the evaluation, except in outlining surrounding anatomy.
Ultrasonography reveals a solid, mostly hypoechoic tumor.
An angiosarcoma infiltrates the surrounding soft tissues. These highly vascular tumors often are amenable to preoperative angiographic embolization.
Vaginal Carcinoma
The current evidence suggests that infection with human papillomavirus (HPV) plays a role in cervical cancer. The HPV DNA is present in most cervical cancers.
Imaging does not have a primary role in cervical carcinoma detection.
Carcinomas in the ectocervix tend to be polypoid and extend into the vagina. Endocervical cancers, on the other hand, infiltrate adjacent soft tissues.
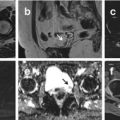
CT: Computed tomography detects a cervical carcinoma as a soft tissue tumor either in the ecto- or endocervix. However, only larger tumors can be detected, and the features of the tumors cannot be distinguished. These tumors enhance less with contrast than do the surrounding soft tissues.
MRI: MRI provides highly accurate information on the morphology and extent of the cervical carcinoma. MRI reveals a cervical tumor as isointense to muscle on T1- and hyperintense on T2-weighted MR images. Most tumors are better defined on T2-weighted images, although smaller ones enhance with contrast and tend to be best seen postcontrast. Cervical tumors demonstrate early and prolonged enhancement compared with poor enhancement of the normal cervical stroma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree