Fig. 2.1
Photograph during cadaver dissection showing the anterior view of the right inguinal region, with the main trunk of the medial femoral circumflex artery (arrow) originating from the deep femoral artery. (Reproduced with permission and copyright © of the British Editorial Society of Bone and Joint Surgery [9])
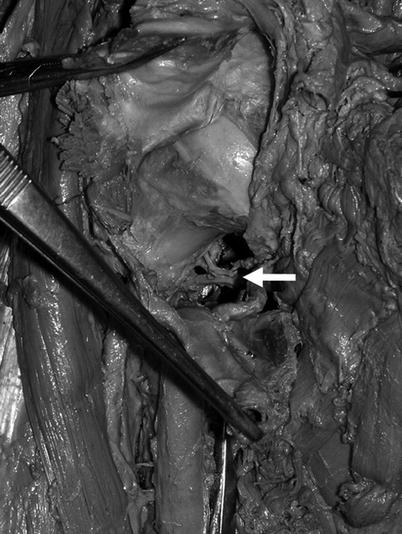
Fig. 2.2
Photograph during cadaver dissection of the anterior view with the right femoral head partly exposed and the femoral neck showing the posterior inferior femoral head nutrient artery (white arrow) (Reproduced with permission and copyright © of the British Editorial Society of Bone and Joint Surgery [9])
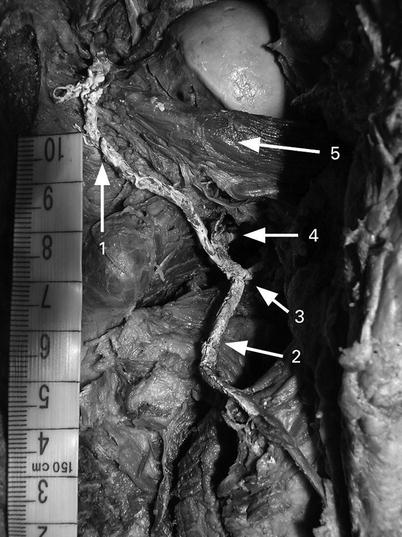
Fig. 2.3
Photograph during cadaver dissection of the posterior view of the left hip joint with the femoral head partly exposed, showing the main branches of the medial femoral circumflex artery (MFCA): 1 deep branch, 2 descending branch, 3 bifurcation of the MFCA, 4 posterior inferior femoral head nutrient artery, and 5 obturator externus muscle (Reproduced with permission and copyright © of the British Editorial Society of Bone and Joint Surgery [9])
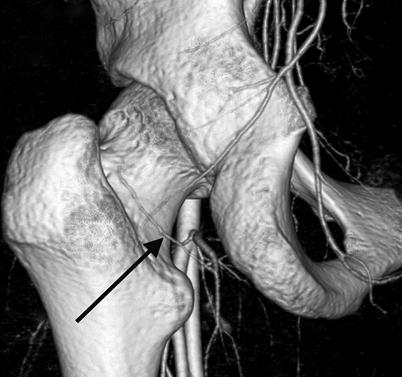
Fig. 2.4
Volume rendering image of the angio-CT scans showing the deep branch of the medial femoral circumflex artery (arrow) from its bifurcation to its division into the posterior superior nutrient arteries (Reproduced with permission and copyright © of the British Editorial Society of Bone and Joint Surgery [14])
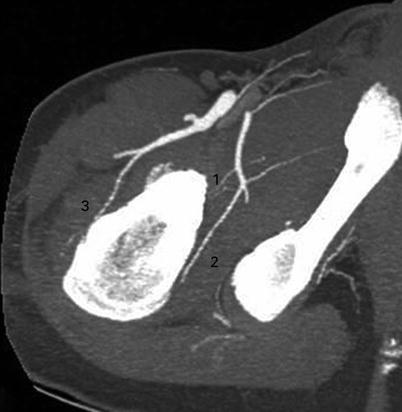
Fig. 2.5
Maximum intensity projection image of the angio-CT scans showing the posterior inferior nutrient artery (1), the deep branch of the medial femoral circumflex artery (2), and the anterior nutrient artery of the femoral neck (3) (Reproduced with permission and copyright © of the British Editorial Society of Bone and Joint Surgery [14])
The main trunk bifurcates into the descending branch, usually single with a diameter of 1.7 mm (0.8–3.6 mm) that divided into two branches, which supply the muscles of the posterior compartment of the thigh. The deep branch, with a diameter of 1.6 mm (1.1–2.7 mm), follows a course directed to the femoral head [7, 9, 14, 19] (Figs. 2.3, 2.4, and 2.5).
2.4.1.1 Posterior Inferior Nutrient Artery
The posterior inferior nutrient artery of the femoral head is not present in all cases. Incidence of appearance depends on the method of visualization used by different authors; it is observed in 11 % of cases by angiographic CT examination [14] compared to 100 % of cases in a classical anatomical study with colored silicone injection [6, 11–13, 15]. Its diameter has been estimated in a microangiographic study to be approximately 0.4 mm (0.1–0.6 mm) [6]. In its intra-articular course, it runs proximally on the medial aspect of the neck toward the femoral head on top of the mobile fold of tissue commonly referred to as the Weitbrecht ligament [12] (Figs. 2.2, 2.3, and 2.5). During the growth phase, the posterior inferior nutrient artery—under the name “inferior metaphyseal artery”—was found to supply approximately two-thirds of the metaphyseal tissue of the femoral head [8]. Almost 18 % of the vascular foramina around the head are located in the posterior inferior aspect of the femoral head in comparison to approximately 80 % located in the posterior superior and anterior superior quadrants of the femoral head [23].
2.4.1.2 The Deep Branch with Posterior Superior Nutrient Arteries
After bifurcation, the deep branch arises proximally, posterior to the obturator externus muscle and anterior to the quadratus femoris muscle. It is easily identifiable in the adipose tissue between these two muscles and is usually closely associated with two veins [9]. In this area, the deep branch of the MFCA can rupture during traumatic hip dislocation when the obturator externus tendon ruptures. The obturator externus muscle and its tendon protects the vessel [10, 24] (Fig. 2.6). In that area, the deep branch is also at risk of iatrogenic damage during posterior exposure of the hip. During the Kocher-Langenbeck approach, division of the tendon of the obturator externus should be avoided. It is also unsafe to divide the distal part of the conjoined tendon comprised of the gemellus inferior and fibers of the obturator internus muscle [10]. After bypassing the obturator externus, the deep branch goes into the trochanteric fossa where it gives off trochanteric branches toward the greater trochanter [2, 10]. In this region, the deep branch of the MFCA anastomoses with the piriformis branch of the IGA. Moving in a cranial direction toward the femoral head, it lies anterior to the conjoined tendon of gemelli and obturator internus and enters the hip joint through a femoral attachment of the posterior capsule, superior to the insertion of gemellus superior and distal to the insertion of the piriformis [2, 9–11, 23]. On this course, it becomes intracapsular, obliquely through the capsule. To protect the deep branch of the vessel, approximately 1.5 cm of the conjoined tendon and capsule should be left undivided from the trochanteric crest during posterior exposure of the hip [10]. During its intracapsular and intra-articular courses, the deep branch is at risk of stretching and increased vessel resistance because of intra-articular pressure [25].
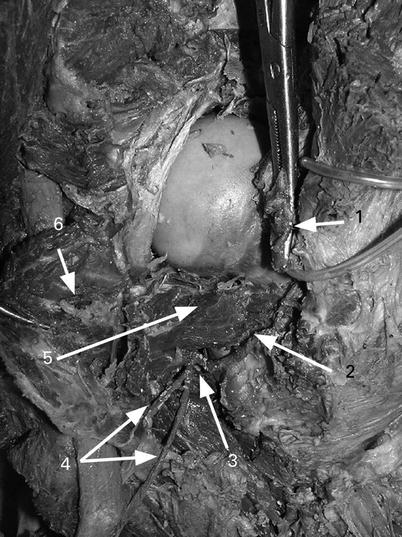
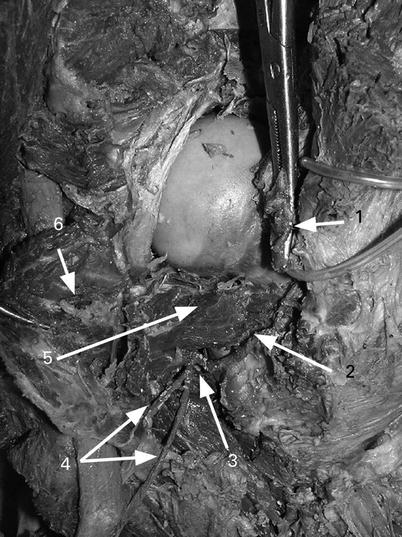
Fig. 2.6
Photograph during cadaver dissection of the posterior view of the right hip joint, showing the topography of the deep branch of the medial femoral circumflex artery (MFCA): 1 conjoined tendon of the gemellus superior, gemellus inferior, and obturator internus muscles (after tenotomy near its femoral attachment), 2 deep branch of the MFCA, 3 bifurcation of the MFCA, 4 descending branches of the MFCA, 5 obturator externus muscle, and 6 quadratus femoris muscle (turned medially) (Reproduced with permission and copyright © of the British Editorial Society of Bone and Joint Surgery [9])
Intra-articularly, it travels subsynovially along the femoral neck within the retinacular fibers.
In its intra-articular course, it divides into 1–5 posterior superior nutrient arteries of the femoral head, continuing within the retinaculum toward the femoral head [9, 10, 12] (Fig. 2.7a, b). Many authors agree that the deep branch divides into the terminal nutrient arteries in all cases [2–15]. Posterior superior nutrient arteries are the most important source of blood supply; they can completely perfuse the femoral head without any other vascular input [15]. The estimated size, via microangiographic studies, of a nutrient artery from the group of posterior superior nutrient arteries of the femoral head in adults is 0.8 mm (0.3–1.6 mm) [6]. Zlotorowicz found that the deep branch was absent in 1/55 cases—the femoral head then being supplied by a well-defined piriformis branch of the IGA—using angiographic CT [14].
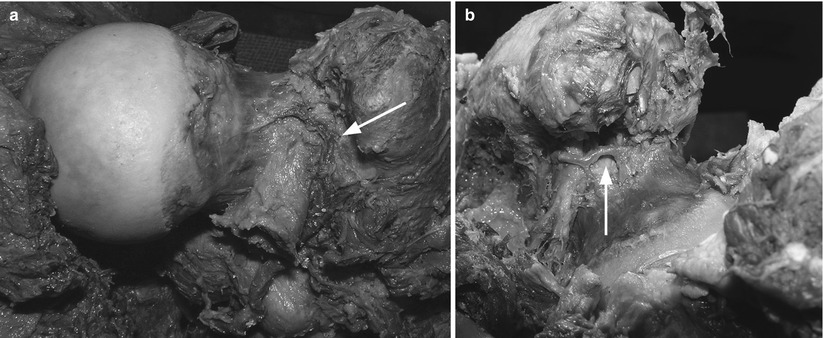
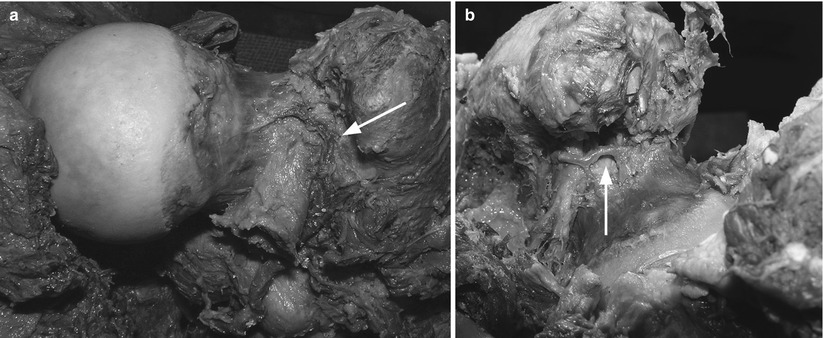
Fig. 2.7




Photographs during cadaver dissection of (a) a posterior view of the right hip joint with the femoral head exposed, showing the terminal branch of the medial femoral circumflex artery (arrow), which we consider to be the posterior superior femoral head nutrient artery, and (b) a posterior view of the left hip joint showing the terminal branches of the medial femoral circumflex artery (arrow), which we consider to be the three posterior superior femoral head nutrient arteries (Reproduced with permission and copyright © of the British Editorial Society of Bone and Joint Surgery [9])
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree