This chapter is not intended to replace standard anatomy texts. For the purposes of this chapter, the lower limb is considered to extend from the thigh to the foot. The thigh extends from the base of the femoral triangle at the inguinal ligament anteriorly and the gluteal fold posteriorly to the level of the knee joint. The femoral triangle provides the portal for most angiography and vascular interventional procedures. Additionally, knowledge of the anatomy of the venous system of the lower limb is critical for the treatment of venous disorders, including thrombosis and varicose veins.
The lower limb is encased in a dense layer of connective tissue—the deep fascia—that acts to contain the leg muscles and improve venous flow as the muscles contract. Septae from the deep fascia separate the thigh muscles into three compartments: anterior, medial, and posterior.
In the calf the fascia is called the crural fascia , and it separates the calf into three compartments: anterior (including the extensor compartment), lateral, and posterior (subdivided into superficial and deep compartments). Accumulation of excess fluid or blood in a compartment may lead to compartment syndrome.
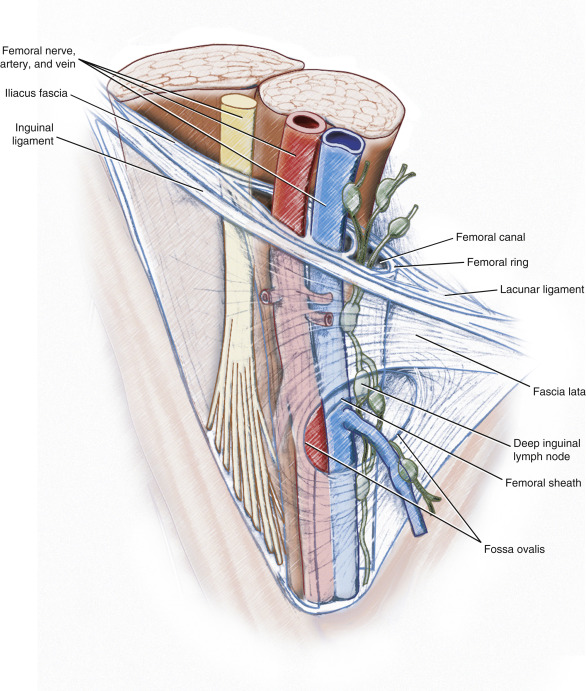
The saphenous opening is a deficiency in the fascia lata inferior to the medial part of the inguinal ligament over the upper portion of the femoral triangle. The opening has a well-defined crescentic margin, except on its medial aspect. A thin connective tissue—the cribriform fascia—covers the opening. The long saphenous vein and lymphatics pass through the fascia and enter the femoral triangle.
The femoral triangle is a space in the upper part of the thigh that is bounded above by the inguinal ligament, medially by the adductor longus, and laterally by the sartorius muscles ( Fig. 10.1 ). The floor of the triangle is formed by the iliopsoas laterally and the pectineus medially. The roof of the triangle is composed of the cribriform fascia and fascia lata, subcutaneous tissue, and skin. The contents of the triangle are, from lateral to medial, the femoral nerve and its branches, the femoral artery and its branches, the femoral vein and its proximal tributaries, including the long saphenous vein and the deep inguinal lymph node, and associated lymphatics.
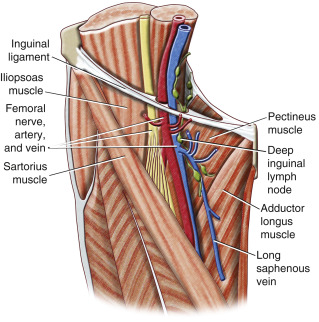
The femoral vein and artery and the lymphatics, but not the femoral nerve, are enclosed in the femoral sheath, which is an extension of the extraperitoneal fascia overlying the iliopsoas and transversalis abdominis. The femoral sheath is further divided into compartments for the femoral artery, femoral vein, and lymphatics. At the inferior extent of the femoral triangle the sheath becomes continuous with the adventitia of the vessels. The medial compartment is called the femoral canal , and its proximal extent under the inguinal ligament is termed the femoral ring . This opening is usually closed by fibrofatty tissue and is the site of a femoral hernia should one develop ( Fig. 10.2 ).
The femoral nerve is the largest branch of the lumbar plexus and is composed of sensory and motor fibers from L2 to L4 . It is formed within the psoas and enters the femoral triangle at about the midpoint of the inguinal ligament. Within the triangle, the femoral nerve divides into multiple branches to the quadriceps, sartorius, and the hip and knee joints. Its largest cutaneous branch—the saphenous nerve—runs obliquely downward in the femoral triangle to lie adjacent to the femoral artery and vein.
The femoral artery arises as a continuation of the external iliac artery beneath the inguinal ligament. In the femoral triangle, it lies centrally between the femoral nerve and vein. The femoral artery gives off the superficial epigastric artery, superficial circumflex iliac artery, and superficial and deep external pudendal arteries in the upper portion of the triangle before it gives off the deep artery of the thigh (profunda femoris) and continues as the (superficial) femoral artery in the adductor canal ( Fig. 10.3 ). Within the canal, the femoral artery gives off several muscular branches and the descending genicular artery. It continues as the popliteal artery. The proximal superficial branches of the femoral artery are important collateral pathways in the event of arterial occlusion.

Branching variations at the origin of the deep artery of the thigh are common, and the length of the (common) femoral artery before the origin of the deep artery of the thigh is variable. Occasionally, the deep artery of the thigh is absent and replaced by direct branches from the femoral artery. Rarely, the anterior division of the internal iliac artery continues from the pelvis as the sciatic artery, which terminates as the popliteal artery. In such cases, the femoral artery is small and supplies only the upper part of the thigh.
The deep artery of the thigh lies posterior to the femoral artery and passes deeply between the pectineus and adductor longus. Proximally, the deep artery of the thigh gives off medial and lateral circumflex femoral branches that form the cruciate anastomosis with obturator branches of the inferior gluteal and superficial circumflex femoral arteries. The cruciate anastomosis often supplies a branch to the sciatic nerve.
The adductor canal is a narrow space deep to the sartorius and bounded anteriorly and laterally by the posterior aspect of the vastus medialis and posteriorly by the adductor longus and adductor magnus. It contains the saphenous nerve, the (superficial) femoral artery, and the femoral vein. The adductor hiatus is an opening between the distal attachments of the adductor magnus immediately above the adductor tubercle of the femur.
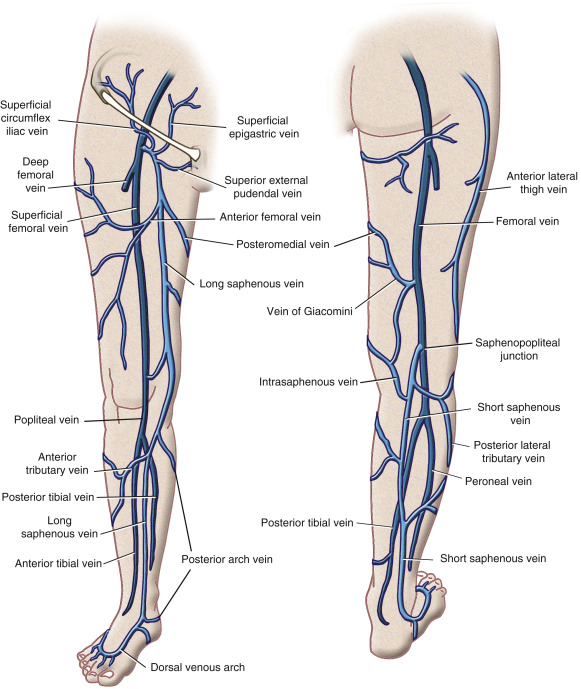
The femoral vein begins as a continuation of the popliteal vein at the adductor hiatus and runs superiorly within the adductor canal medial and deep to the femoral artery. There are numerous valves within the femoral vein that aid venous flow up the limb. The deep femoral vein accompanies the deep artery of the thigh and may be multiple. Unlike the arteries, there is significant variation in the number and position of the smaller veins. Numerous perforating veins connect the femoral vein with the superficial veins and drain blood from the thigh muscles. At the apex of the femoral triangle, the femoral vein passes in a posterior-to-medial direction with respect to the femoral artery. Puncture of the femoral artery low in the femoral triangle may result in damage to the saphenous nerve and unintentional puncture of the femoral vein. Low punctures are also more often associated with an arteriovenous fistula when both the artery and vein are simultaneously punctured.
The long saphenous vein arises in the foot from the dorsal venous arch and ascends anterior to the medial malleolus up the medial aspect of the calf, accompanied by the saphenous nerve to the knee, where it lies approximately one handbreadth posterior to the medial femoral condyle. The saphenous nerve separates from the vein above the knee joint, and it is at this point that the long saphenous vein is usually punctured for thermal ablation. Several perforating veins connect the long saphenous vein to the deep femoral veins. They are grouped above the ankle, below and just above the knee, and along the lower half of the adductor canal. These perforating veins also contain valves that direct flow to the deep system through the fascia lata. The oblique course of these veins through the fascia causes mechanical compression during muscle contraction ( Fig. 10.4 ). The long saphenous vein also receives large cutaneous veins from the lateral and anterior aspect of the thigh just before it passes through the cribriform fascia. Within the femoral opening, the long saphenous vein receives the superficial circumflex iliac, superficial epigastric, and external pudendal veins. These veins provide connection between the saphenous vein and the deep pelvic veins. Ovarian vein reflux may cause an increase in pressure in these tributaries of the long saphenous vein at the femoral opening.