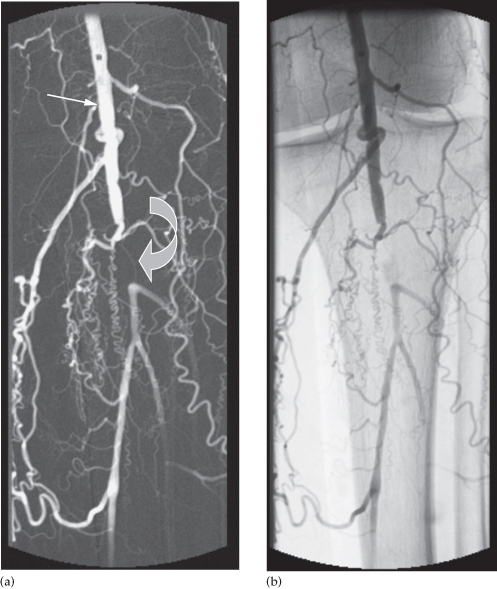
Fig. 17.2 Digital subtraction arteriogram following an intra-arterial injection of contrast medium. On the subtracted image (a) the bones and soft tissues are barely visible compared to the unsubtracted image (b). The angiogram shows a patent popliteal artery (thin arrow) with a short segment occlusion proximal to the trifurcation (curved arrow).
- Diagnosis of vascular diseases (e.g. vascular occlusive disease, aneurysm, arteriovenous fistula, arteriovenous malformation)
- Diagnosis or localization of vascular tumours (e.g. insulinoma, parathyroid adenoma)
- Preoperative definition of vascular anatomy (e.g. organ transplant, local tumour resection, revascularization)
- Diagnosis and treatment of vascular complications of disease, trauma or surgery
- Performance of vascular interventional procedures (e.g. percutaneous transluminal angioplasty, stenting, embolization, transcatheter infusional therapy)
Magnetic Resonance Angiography
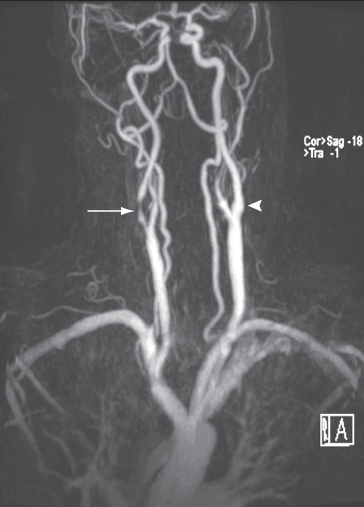
Magnetic resonance angiography is a very useful non-invasive technique, which can demonstrate both arteries and veins. Images of the vascular system can be obtained using special sequences that depend on the signal obtained from flowing blood or via an injection of a contrast agent (gadolinium DTPA (diethylene triamine pentacetic acid)) into a peripheral vein (Fig. 17.3).
Fig. 17.3 MRA of the carotid arteries showing a short stenosis in the right internal carotid artery (long arrow). A normal internal carotid artery is seen on the left (arrowhead).
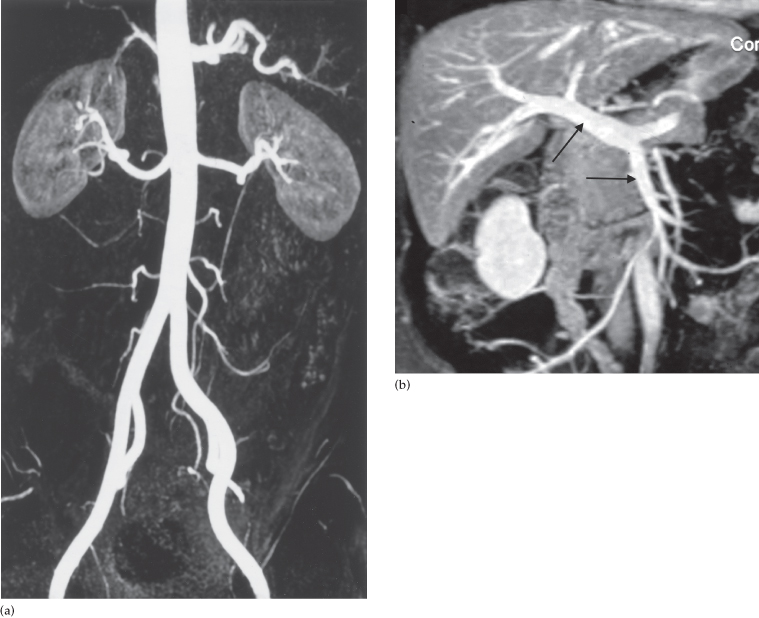
Magnetic resonance angiography is particularly useful for showing the aorta and its branches (Fig. 17.4a), aortic dissection, the portal vein (Fig. 17.4b) and for demonstrating carotid artery disease, peripheral vascular disease and renal and mesenteric artery stenosis. Aneurysms and vascular malformations can also be detected in the intracranial circulation.
Fig. 17.4 MRA. (a) Contrast angiogram showing a normal abdominal aorta and its branches. (b) Contrast angiogram showing the superior mesenteric (horizontal arrow) and portal (upward pointing arrow) veins.
Computed Tomography Angiography
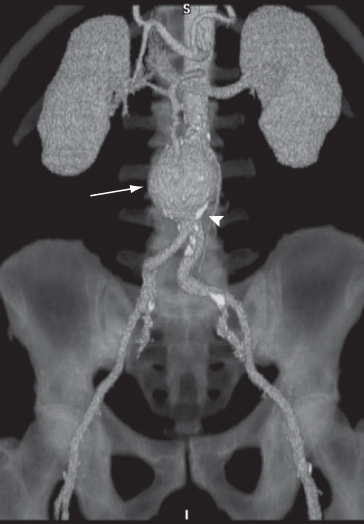
Spiral CT, particularly multidetector CT, enables large areas of the body to be scanned quickly. After an intravenous injection of contrast, many thin sections can be obtained so reconstruction in the coronal and sagittal planes can be performed to give optimum visualization of the vessels.
Computed tomography angiography is particularly useful for visualizing the aorta and its branches for suspected aneurysms (Fig. 17.5) including any rupture or leakage. CT pulmonary angiography demonstrates the pulmonary arteries and can detect pulmonary emboli (see Chapter 2, Fig. 2.102c). The peripheral arteries can also be visualized by CT angiography, as can the cerebral vessels.
Fig. 17.5 CT angiogram. Reconstruction from many thin axial sections following an intravenous injection of contrast demonstrating an aortic aneurysm (arrow). Calcification is seen in the wall of the arteries (arrowhead).
Ultrasound of the Arterial System
Ultrasound has an important role to play in diagnosing arterial disease, both in the carotid arteries and peripheral vessels, and is commonly the primary imaging modality used in assessment. The common, internal and external carotid arteries can be readily visualized in the neck. The location or size of any atheromatous plaques and the severity of any luminal narrowing can be determined. With colour Doppler imaging, a stenosis in the artery can be visualized and an occlusion will show as an absence of flow. Because a stenosis disrupts the normal flow pattern, analysis of the flow–velocity waveform can give further information regarding the degree of stenosis. Imaging of the iliac vessels may be difficult due to overlying bowel gas, but evaluation of the abdominal aorta is invariably successful and can easily be performed during an outpatient assessment.
Ultrasound Venography
Duplex ultrasound has now largely replaced contrast venography for the detection of venous thrombosis. With a venous thrombosis, intraluminal echogenic material is visible and the veins lose their normal compressibility; thrombus-free veins should be compressible by direct pressure using the ultrasound transducer. Colour Doppler scanning shows that there is a lack of spontaneous flow in the affected veins. Ultrasound can readily visualize the external iliac, common femoral and popliteal veins, although it can be sometimes difficult to visualize the calf veins. In practice, this is often not clinically significant as calf vein (i.e. below knee) thrombosis may not be treated.
Contrast Venography
Contrast venography is routinely used for the evaluation of the upper limb veins, as it enables imaging of the central veins with the arm in a neutral and abducted position and allows a functional evaluation. A large volume of contrast medium is injected into a vein on the arm or the hand. The contrast is forced into the deep venous system of the upper limb by means of a tourniquet. Thrombi may be seen as filling defects in the opacified veins, and any stenosis or occlusion in the central veins is well demonstrated.
Venography in the lower limb is seldom used, having been superseded by ultrasound.
Interventional Radiology
Radiologists carry out various percutaneous techniques under imaging control, including dilating stenoses, occluding vessels, draining abscesses and other fluid collections, and obtaining biopsy samples. These procedures greatly assist and may modify surgery, or even replace it altogether. They are carried out with the help of a variety of imaging modalities, notably fluoroscopy, angiography, ultrasound, CT and, more recently, magnetic resonance imaging (MRI). Interventional radiology is usually performed under local anaesthesia, causing only relatively minor discomfort to the patient, allowing many procedures to be performed as ‘day cases’. Only the basic principles of the interventional techniques in widespread use will be described here.
Angioplasty and Stents
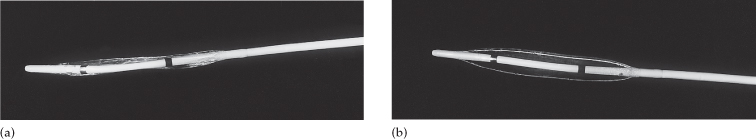
Arterial stenoses and even occlusions may be traversed with a guidewire. A balloon catheter can be passed through the abnormal site, which has been previously determined by arteriography (Fig. 17.6). The stenosis is then dilated by inflating the balloon (angioplasty) (Fig. 17.7). This percutaneous technique, which usually uses the femoral artery as an access route, has been widely employed in peripheral vascular disease and gives results as good as bypass surgery, particularly for iliac and superficial femoral artery disease. Short stenoses are the ideal lesions to treat with angioplasty.
Fig. 17.6 Percutaneous transluminal angioplasty. (a) Preliminary arteriogram showing an occlusion in the left superficial femoral artery (arrow). (b) Following the angioplasty, the lumen has been restored.

Fig. 17.7 Percutaneous angioplasty balloon catheters. (a) The catheter prior to inflating the balloon. (b) The catheter with the balloon distended as it would be if it were inside the artery.
Stents are balloon expandable or self-expanding metal cylinders that can be embedded in plastic and collapsed to enable them to be inserted through an artery or vein (Fig. 17.8). As they ‘reinforce’ the vessel at the site of angioplasty, they have a more durable result. Stents are commonly used in the treatment of arterial stenosis and occlusion in coronary disease, in peripheral vascular disease, and in patients with mesenteric ischaemia secondary to atherosclerotic stenoses in the mesenteric arteries. Their role in the management of renal artery stenosis is debatable following several recent trials, but is still indicated to treat patients with deteriorating renal function, flash pulmonary oedema and occasionally renal vascular hypertension.