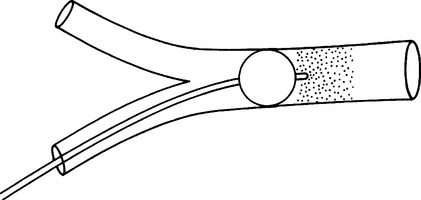
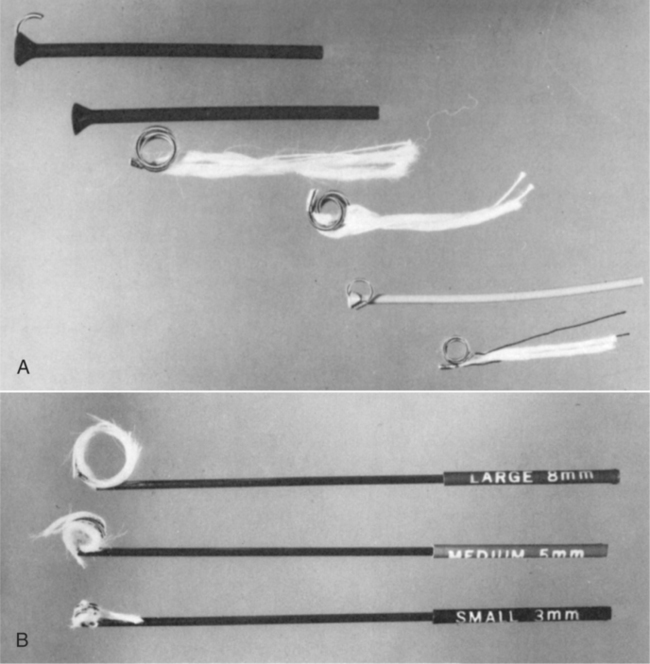
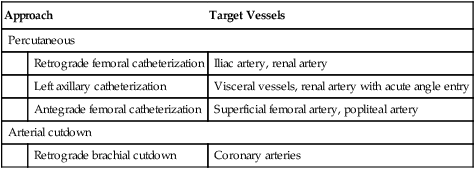
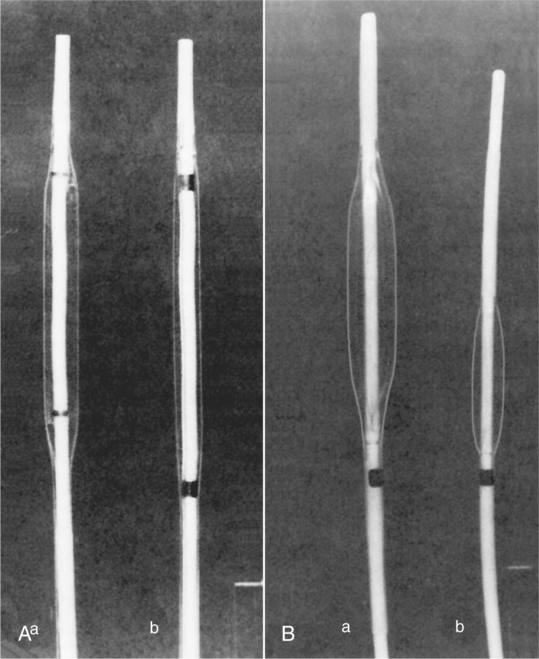
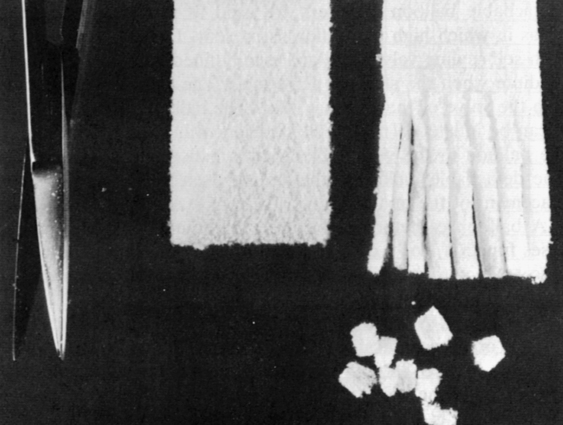
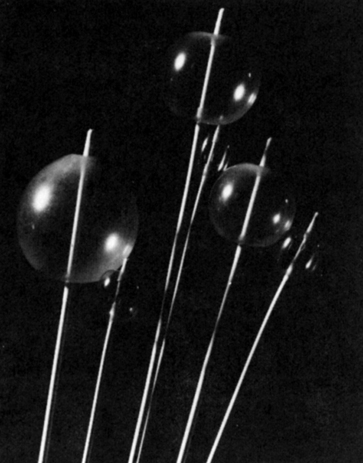
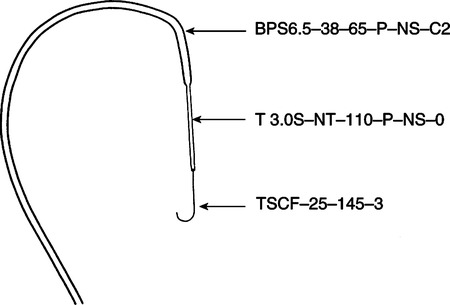
CHAPTER 17 After completing this chapter, the reader will be able to perform the following: Box 17-1 illustrates the present scope of interventional radiography for both vascular and nonvascular procedures. The nonvascular interventional procedures will be discussed in Chapter 19 but are listed here for comparison with the vascular interventions. Vascular interventions can be divided into methods that either reduce or increase blood flow. These techniques are meant to be therapeutic in nature. Vascular interventional radiography procedures use angiography as the primary procedural method for access to the site of the pathologic process. In many cases the percutaneous interventions can save the patient from undergoing a lengthy surgical procedure. These media include microfibrillar collagen,oxidized cellulose, and Gelfoam, which is the most popular. Gelfoam is manufactured in sheets and in powder (Fig. 17-1). It was first used in 1945 to control hemorrhage during neurosurgery, and it has been successfully used in intravascular occlusion. The powdered form consists of particles ranging from 40 to 60 μm in size. When Gelfoam is used, small fragments (pieces) are cut from the sheet and soaked in normal saline solution, a contrast agent, or both to provide radiopacity. These pieces are then placed into the vessel by injection through an angiographic catheter. The size of the inside lumen of the catheter determines the maximum size of the piece to be used. Gelfoam has the disadvantage of being easily refluxed, causing recanalization of the vessel. This type of embolic medium, when injected into the lumen of a vessel, provides a framework for blood clot formation. Intravascular lysing of this type of material can occur in a relatively short period, but it is much more persistent in a vessel than an autologous blood or tissue clot alone. This type of embolic medium lasts from less than 48 hours to 30 days. Balloon catheters provide a safe, temporary method of occluding vessels to control or prevent bleeding, as well as isolating vessels for selective infusion of chemotherapeutic agents or placing other types of embolic media (Fig. 17-2). The advantages of using the balloon catheter are that it is retrievable for removal and the position of the balloon can be changed easily. A balloon catheter can be used in conjunction with embolic material and in such cases function like a cork to prevent reflux of the particulate material from the target vessel. Once the particulate embolic material has been firmly set in place, the balloon can be removed (Fig. 17-3). Occluding springs are mechanical devices of stainless-steel coiled wire about 5 cm long and available in 3-, 5-, 8-, 10-, 12-, and 15-mm diameters. Strands of wool, silk, or Dacron are affixed to the wire to provide a framework for clot formation. The wool-tailed coils are primarily used for larger arteries, whereas the silk- or Dacron-tailed coils are used to occlude smaller arteries. These coils were developed in 1975 by Gianturco, Anderson, and Wallace and are commonly called Gianturco-Anderson-Wallace (GAW) coils (Fig. 17-4). The technique for placement of these liquid emboli substances requires the use of coaxial catheters. These are specially paired catheters comprising a larger outer catheter and a smaller inner catheter. These sets come with a correctly sized guide wire and are complete for use during intravascular embolization procedures (Fig. 17-5). The large outer catheter is passed through the vessel to the approximate site of occlusion. A small amount of sterile silicon grease can be applied to the tip of the small inner catheter, which is then passed through the outer catheter into the specific vessel to be occluded. The application of the silicon grease helps to prevent adhesion of the catheter tip to the vessel wall after injection of the embolic medium. The Guglielmi detachable embolization coil is an example of a device that combines electrocoagulation with a detachable mechanical device to achieve satisfactory results.1 Once in place, the electric current promotes thrombus formation, and detachment of the coil aids in the occlusion process through electrolysis of its soft stainless-steel connector. The procedure time is shortened, and the device can be manufactured in various lengths and coil sizes for use in a variety of vessel lumens. Interventional procedures can also be applied to increase the flow of blood in a particular vessel. Four types of procedures are used: percutaneous transluminal angioplasty (PTA), vascular stent placement, intravascular thrombolysis, and intra-arterial infusion of vasodilators. These procedures provide relatively safe methods of increasing blood flow without the necessity of extensive surgery. These studies are usually done using the percutaneous approach. The arterial cut-down approach is occasionally used, and the necessary sterile tray should be available in the radiography suite. Box 17-2 summarizes some common approaches used for angioplasty. Percutaneous transluminal angioplasty is a nonsurgical procedure defined as the process of accessing a blood vessel through a puncture in the skin and performing a procedure through the blood vessel to reshape or repair the inside diameter of the vessel through balloon inflation. This procedure was first performed in 1964 by Dotter and Judkins; they used a coaxial catheter system (telescoping catheter) to recanalize a stenosed femoral artery. In 1974, Gruntzig developed the double-lumen balloon catheter, which reduced the complication rate at the puncture site. Currently, there are many different balloon lengths and diameters available for use during PTA (Fig. 17-6).
Vascular Interventional Procedures
 Describe the general interventional techniques used to reduce blood flow
Describe the general interventional techniques used to reduce blood flow
 List the specific indications and contraindications for the reduction of blood flow
List the specific indications and contraindications for the reduction of blood flow
 List the various procedures used to reduce blood flow
List the various procedures used to reduce blood flow
 Identify the complications inherent in interventional blood flow reduction
Identify the complications inherent in interventional blood flow reduction
 Identify the general interventional techniques used to increase blood flow
Identify the general interventional techniques used to increase blood flow
 List the specific indications and contraindications for increasing blood flow
List the specific indications and contraindications for increasing blood flow
 List the various procedures used to increase blood flow
List the various procedures used to increase blood flow
 Describe the complications resulting from interventional vessel dilation
Describe the complications resulting from interventional vessel dilation
 Explain the techniques used to remove foreign bodies from the vascular system
Explain the techniques used to remove foreign bodies from the vascular system
 Describe the TIPS (transjugular intrahepatic portosystemic shunting) procedure
Describe the TIPS (transjugular intrahepatic portosystemic shunting) procedure
TECHNIQUES USED TO REDUCE BLOOD FLOW
Procedure
Transcatheter Embolization and Balloon Occlusion
Cellulose Sponge Embolic Media.
Balloon Catheter Occlusion.
Occluding Spring Emboli and Other Mechanical Occluders.
Liquid Embolic Media.
Intravascular Electrocoagulation
TECHNIQUES USED TO INCREASE BLOOD FLOW
Procedure
Percutaneous Transluminal Angioplasty
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Vascular Interventional Procedures