Hemangioma
Vascular malformation
Female/male ratio 5:1
Female/male ratio 1:1
Endothelial cell proliferation
Normal endothelial cell grow
Presence at birth (40%)
Presence at birth (90%)
Proliferative phase Involutive phase
Proliferation parallel with child growth
Classification
Vascular malformations are classified according to the predominant vessel abnormality: capillaries, veins, arteries, lymphatic system, or a combination of the above. Moreover, they could be classified according to their hemodynamic characteristics as high-flow or low-flow malformations. The former corresponds to arterial malformations (macrofistulas or microfistulas via the nidus); the latter includes the veins, lymphatic system and capillaries.
Classification according to hemodynamic characteristics makes it possible to plan the best treatment options (Table 15.2).
Table 15.2
Classification and treatment of vascular malformation
Classification | Treatment | ||
Low-flow | Venous | Cavitary | Sclerotization |
Spongious | |||
Dysmorphic | |||
Lymphatic | Macrocystic (>2 cm2) | ||
Microcystic (<2 cm2) | |||
Capillary | |||
High-flow | Arteriovenous malformation | Stage 1: quiescent | Embolization |
Stage 2: expansive | |||
Stage 3: invasive | |||
Stage 4: decompensated | |||
Mixed | Combined | ||
Clinical Findings
The main clinical findings of arteriovenous malformations are: esthetic impairment, compression of vascular and nervous structures, pain, ulceration, decreased function of the affected extremity, venous stasis, ischemia, skeletal abnormalities, localized consumptive coagulopathy and risks of bleeding during surgery. These clinical findings are due to the enlargement of the arteriovenous malformation, and exacerbation can follow trauma, sepsis or hormonal changes.
Diagnosis
Non-invasive imaging modalities, such as Color Doppler UltraSound (CDUS), CT-angiography (CTA), and Magnetic Resonance (MRA), are mainstays in treatment planning. In fact, treatment is planned according to the classification of each patient’s conditions as high-flow or low-flow lesions basing on imaging findings.
High-flow lesions could be treated either with transarterial embolization or surgical excision or a combination of these; low-flow lesions are treated with percutaneous sclerotization or laser therapy.
CDUS is a first-line imaging technique for arteriovenous malformation followed by CTA and/or MRA. Digital subtraction angiography (DSA), due to its invasiveness, is mainly performed to guide treatment.
Imaging and Reporting
Patient Preparation
Patient in a prone or supine position depending on the location of the lesion;
Peripheral venous access (22–20 G), positioned in the contralateral upper arm with respect to the lesion location in order to avoid artifacts;
Removal of movable dental prostheses and all metallic objects;
Surface coil.
Technical Aspects of CTA
Arteriovenous malformations are typical at CTA, being inhomogeneous and hypodense in non-enhanced scans, with typical enhancement after contrast media injection depending on the type of malformation (early, delayed).
CTA enables the evaluation of the extent of the vascular malformation, but with a lower contrast resolution and radiation exposure in comparison with MRA (Fig. 15.1).
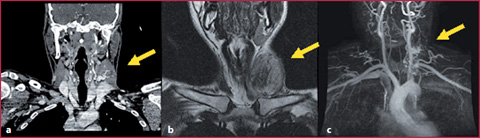
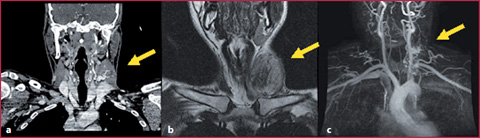
Fig. 15.1
38-year-old male patient complaining of palpable swelling of the left latero-cervical region. a CTA in the coronal plane depicts an intramuscular arteriovenous malformation involving the left sternocleidomastoideus muscle (arrow). b T2 FSE sequence in the coronal plane shows the anatomical relation of the lesion with the surrounding structures (arrow). c MRA demonstrates both the arterial feeders and venous drainage of the lesions (arrow)
Technical Aspects of MRA
MRA is an excellent imaging method for the evaluation of vascular malformations for its capability to define the anatomical relationship between the lesion and surrounding structures (muscles, bones, tendons, nerves, airways).
The examination protocol involves: T1 and T2 weighted Fast Spin-Echo (FSE) sequences with and without fat suppression for anatomical evaluation and 3D T1 weighted time-resolved sequences before and after contrast medium administration (Fig. 15.2).
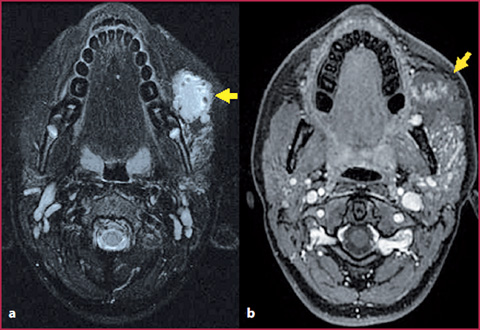
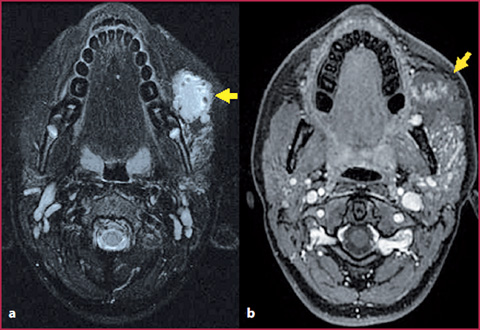
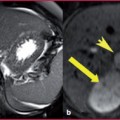
Fig. 15.2
13-year-old female patient with a vascular malformation involving the left parotid space; a T2 FSE weighted sequence with fat suppression depicts hypointense areas inside the lesion suggestive of intralesional thrombosis (arrow). b T1 weighted GRE sequence acquired in the delayed phase shows how the lesion is only partially enhanceing, and thus classified as low-flow
Arteriovenous malformations are usually hypointense or isointense in T1 weighted sequences (with a heterogeneous signal in the case of thrombosis or bleeding), and hyperintense in T2 weighted sequences with hypointense areas usually related to thrombus, internal septa or phlebitis. (Tables 15.3, 15.4). In case of bleeding, the signal in both T1 and T2 weighted sequences changes in relation to the state of hemoglobin degradation (Table 4.7 in chapter 4).




Table 15.3
Signal characteristics of vascular malformations at MRI
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree