Fig. 43.1
Superselective angiography. The deep circumflex iliac (DCI) artery is shown
The external diameter of the DCIA is usually around 2–2.5 mm and can be easily handled without microscopic magnification. The artery runs along the inner lip of the iliac crest and diverts away from the upmost point of the iliac crest to give off multiple intramuscular branches to the iliacus and anastomoses with the iliolumbar and superior gluteal artery. From the origin of the external iliac artery to the iliac crest, the vascular pedicle can be 8–10 cm in length which provides a versatile radius to swing around the proximal femur. All along its course, the DCIA is accompanied by its venae commitantes that drain into the external iliac vein or femoral vein.
Most of the surgeries use the DCIA as the vascular pedicle because the constant position and diameter of the vessels make it very suitable for harvest and transplantation. In addition to the DCIA, some surgeons used the superficial circumflex iliac artery that travels between the fatty tissue and fascia in the inguinal region [9, 10]. It is noted that the vessels of the superficial circumflex iliac artery are smaller in size and more difficult to harvest.
43.3 Surgical Technique
Under general anesthesia, patient is put in the supine position with a sandbag behind the operated side of the pelvis. A long and curve skin incision is made on the iliac crest 8 cm pass the anterior superior iliac spine (ASIS), along the inguinal ligament, with the distal limb extended medially to the hip joint (Fig. 43.2). The femoral artery and the vein are looped to identify the external iliac artery. By gentle traction on the external iliac artery, tributaries of the external iliac artery can be exposed. The superficial circumflex iliac vessels and the deep circumflex iliac vessels are usually arising from the external iliac vessels just opposite to the origin of the inferior epigastric artery and could be easily traced to the inner lip of the iliac crest, into which feeding branches were sent (Fig. 43.3a). The external and internal oblique abdominal muscles are cut from its insertion on iliac crest. Dissection of the vascular pedicle should be carefully performed after opening the inguinal ligament and the transversalis fascia. The first few tributaries behind the inguinal ligament can be ligated. Beyond the point of ASIA, a sleeve of iliacus muscles should be left on the inner lip of the iliac bone that encases the vascular pedicle to avoid overzealous dissection and inadvertent tear of the feeding vessels. A suitable-size bone graft is harvested with its attached vascular bundle and muscle sleeve (Fig. 43.3b).
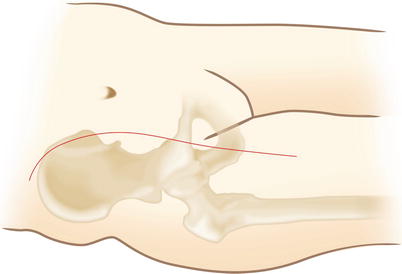
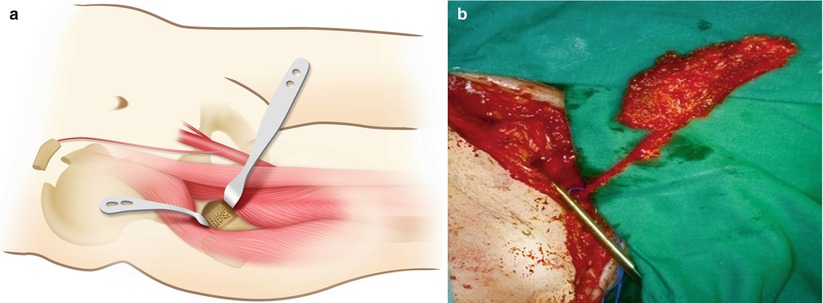
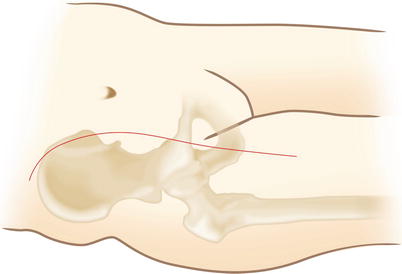
Fig. 43.2
Skin incision for VIBG surgery
Fig. 43.3
Deep dissection. (a) The DCIA can be found opposite to the inferior epigastric artery. Two Hohmann retractors are put intra-articularly for exposure. A bone trough is made on the femoral neck. (b) VIBG with vascular pedicle
The hip joint is exposed by using the inferior limb of the skin incision. Between the sartorius muscle and the tensor fascia latae (Smith-Petersen’s interval), the anterior hip joint capsule is exposed by retracting the rectus femoris medially and the hip abductors laterally. The anterior joint capsule is incised in an H-shape manner to expose the head-neck junction of the hip joint. Rotation and manipulation of the hip will bring the femoral head into view. A bone trough about 1.5 cm × 3 cm is made in the femoral neck leading into the head using sharp narrow osteotomies (Fig. 43.3a). Repeated sharp cuts along the top end of the trough open into the ischemia area of the femoral head. The hard and sclerotic avascular bone is removed using high-speed burrs as thoroughly as possible. If the cartilage is cracked that can been seen directly from the inside, careful out-pushing of the cartilage shell from inside the femoral head can correct the indentation and make it more congruent with the acetabulum.
The void and cavity after debridement is filled with bone chips by gentle impaction of a layer of cancellous bone to the subchondral level. The remaining space is to be filled in with a tailored piece of iliac crest bone with its intact blood supply of DCIA. A tunnel below the iliopsoas is made by blunt dissection with the hip in flexion. A large-size Penrose drain is passed beneath the inguinal ligament along the tunnel as a channel to transfer the graft to the anterior aspect of the femoral neck. The entire graft is slid into the Penrose drain and wrapped by it. By carefully pushing of the graft from the inside of the iliopsoas, the graft can be transferred to the anterior hip with intact pedicle. The Penrose drain is then incised completely with scissor to bring out the graft. As long as the graft is transferred to the anterior hip joint, it can be trimmed to a suitable size to be inserted through the bone trough into the femoral head. The graft can be pushed into the trough to produce a locked-in position and additional holding implant is unnecessary.
Postoperatively, the surgically treated hip is put in a position with 30° flexion and neutral rotation. This posture is advised for approximately 1 week to relax the tension of the vascular pedicle. Hip motion is encouraged as tolerated. The patients are instructed to use double crutches to avoid full weight bearing on the involved limb for 6 weeks. During the following weeks, the amount of weight bearing can be gradually increased by using a single crutch and progresses to a fully unassisted weight bearing by 6 months.
43.4 Indication
The indications for VIBG have not been well established in the literature. The factors affecting treatment results include staging (demonstration of the lesion by radiograph or magnetic resonance imaging, size of the necrotic segment, location of lesion relative to the weight-bearing area, the amount of femoral head depression, and the acetabular involvement), risk factors (use of steroid, medical comorbidities, or systemic disease), and patient-specific factors (age, activity level, or body mass).
In a survey of treatment modalities in the North America, total hip replacement is the most commonly selected treatment of postcollapse ONFH, and core decompression is the most frequently offered treatment for symptomatic precollapse ONFH [11]. Vascularized bone grafting is suggested by only 3–10 % of the responders who are active members of the professional society. It is generally agreed that a symptomatic case with the lesion size more than 30 % of the femoral head needs operative treatment to prevent early collapse of the femoral head. For asymptomatic necrotic lesions with an area smaller than 30 % of the femoral head, close follow-up without treatment appears to be adequate in most of the cases [3, 4, 12].
In the literature, most of the studies of VIBG reported a mix group of hips ranging from precollapse stage to early postcollapse stage. In a study of 33 segmental collapse hips, 26 ARCO stage IIIA and 7 ARCO stage IIIB, only 24 % of the hips treated with VIBG survived without converting to total hip replacement with a mean survival of 74 months. The authors concluded that VIBG is not indicated for the treatment of ONFH with segmental collapse [13]. Other studies also reported similar results in postcollapse hips with a relatively low successful rates [9, 10, 14, 15]. As a contrast, Babhulkar reported a clinical success rate of 95 % in 22 ARCO III hips with a follow-up period of 5–8 years by using vascularized iliac pedicle grafting [16]. However, by looking at the illustrated cases in that report, many of the clinically successful cases showed radiographic collapse of the femoral head. Based on the findings, the rational indication for VIBG should be ONFH without collapse in a young active patient with the lesion more than 30 % of the femoral head. Contraindications include a segmental collapse hip, preexisting thromboembolic disease, a risk of bleeding or thrombocytopenia, a questionable vascular supply to the iliac graft due to factors such as surgery or trauma, multifocal osteonecrosis involving the ilium, untreated inguinal or femoral hernia, and asymptomatic hips [13].
43.5 Clinical Results
Between 1994 and 1999, the author had performed 100 cases of VIBG in 86 patients at the author’s institute. Thirty-nine hips in 33 patients with a minimal follow-up of 2 years were reported [17]. The overall clinical success rate was 82 % and the radiographic success rate was 56 %. The rate of conversion to replacement arthroplasty was 10.3 %. We had further followed up 33 hips with preoperative segmental collapse lesions for 7.1 years. VIBG by using the technique described in this chapter had delayed the conversion to total hip arthroplasty by an average of 7 years in ARCO stage IIIA hips and by 2.9 years in ARCO stage IIIB hips [13].
Eisenschenk et al. had performed VIBG in 102 hips and achieved 87 % clinical success rate and 56.1 % radiographic success rate [18]. Many other reports have been published by using similar technique as described in this chapter [14–23]. The clinical success rate in precollapse hips ranged from 43 to 100 % with an average success rate around 72 % (Table 43.1). Iwata and Hasegawa had used superficial circumflex iliac vessels as the pedicle in their patients and had achieved a 52–74 % success rate [9, 10].
Table 43.1
Summary of success rate
Authors | Case no. | Success rate | Follow-up (years) | |
|---|---|---|---|---|
Precollapse | Postcollapse | |||
Iwata et al. [9] | 23 | 17/20 | 0/3 | 1–6 |
Leung [19] | 21 | 4/5 | 4/16 | 5–12 |
Wassenaar et al. [20] | 12 | 3/5 | 2/7 | 4.1 |
Ishizaka [21] | 31 | 9/18 | 7/13 | 2–11 |
Hasegawa et al. [10] | 31 | 12/27 | 2/4 | 8 |
Feng et al. [22] | 17 | 7/12 | 3/5
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |





