Fig. 33.1
Vertebral compression fractures typically occur spontaneously or as a consequence of minimal trauma, resulting from spinal loading during daily activities such as bending, lifting, and climbing stairs [19]. The most common locations are the midthoracic region (T7–T8) and the thoracolumbar junction
Fig. 33.2
When thoracic kyphosis develops, the midthoracic region receives tremendous load during flexion of the spine leading to potential compression fractures. Secondary contributors to osteoporosis include hypercalcemia, abnormal thyroid, and renal functions [18]. Users of oral glucocorticoids have a 2.6-fold increase risk of fracture
Osteolytic metastases and myeloma can cause the destruction of vertebral bodies and fractures, leading to pain and disability. Patients with advanced cancer can present with bone metastases to the vertebral bodies. The incidence of metastatic lesion to the spine depends on the primary cancer: 80% of patients with prostate cancer, 50% with breast cancer, 30% with lung, thyroid, or renal cell cancer [21]. Rarely, benign tumors such as spinal osteoid osteoma and aneurismal bone cysts can lead to instability and painful compression fractures. Vertebral augmentation can be used to reinforce and stabilize fractures related to tumors.
The multiple consequences of vertebral fractures can lead to increased morbidity and mortality. Pain and disability increases with kyphosis and vertebral compression fracture [1]. The physical consequences include pulmonary compromise. Studies suggest that there is decreased lung capacity and reduced pulmonary function with vertebral height loss and decreased lung volume [2]. As the spine changes with significant kyphosis, the downward angulation of the ribs leads to the 12th rib resting on the iliac crest. This results in the abdomen protruding and can lead to symptoms of distension, constipation, early satiety, and eructation (see Fig. 33.3). Above all, the forward position of the thoracic spine leads to strain of the posterior elements of the thoracic spine as the patient attempts to straighten his or her spine.
Fig. 33.3
As the spine changes with significant kyphosis, the downward angulation of the ribs leads to the 12th rib resting on the iliac crest. This results in the abdomen protruding and can lead to symptoms of distension, constipation, early satiety, and eructation
As seen by the author, the forward expansion of the abdomen leads to forward loading of the lumbar sacral spine, thereby exacerbating discogenic pain. The limited ability of the sacrum to flex and extend may load the sacroiliac joint and cause pain. Weakened physical function can lead to restricted daily activities, resulting in required assistance from family or hired help. The psychosocial consequences of the limitation of activities are seen with their reduced ability to fulfill their accustomed social roles and dependency upon others. This leads to poor self-esteem, depression, and social isolation [1, 3, 22]. There is also increased incidence of sleep disturbances. The number of depressive symptoms rises with the increased number of fractures. Studies reveal high mortality and reduced quality of life years (QALY) with vertebral compression fractures [1].
In addition to a detailed history and examination, imaging evaluations are standard in confirming the diagnosis of acute compression fractures. The radiologic findings on plain films may show subtle height loss changes. Comparison films are helpful to determine acute versus chronic fractures. Unfortunately, occult vertebral fractures are common with false-negative rates of 27–45% by radiologists [23].
MRI is the study of choice with T1 and STIR sagittal sequences. Acute vertebral compression fractures are revealed with marrow edema within the vertebral body. Assessment of spinal canal compromise and fractures of the pedicles is important. CT scan may be a useful alternative combined with a nuclear bone scan when the patient is not a good candidate for MRI. Bone scan may be helpful in fractures greater than 3–4 months in age where there is no marrow edema on MRI.
Treatment Goals
The treatment goals of vertebral compression fractures include pain management, rest, rehabilitation, and restoration of mechanical stability. Pain management usually involves use of opioids and nonsteroidal anti-inflammatories (NSAIDS). Medical management may also include treatments for osteoporosis: calcium, vitamin D, bisphosphonates, or nasal Miacalcin.
Prolong bedrest may allow the compression fracture to stabilize but can lead to fatigue and loss of muscle strength and bone density in elderly patients [24]. Other concerns of patients in prolonged bed rest are pressure sores and deep vein thrombosis in older patients. Back braces may offer support and stabilize the vertebral compression fractures. Limited contact orthoses such as the tri-pad Jewett extension brace are commonly used. Many patients do not tolerate the braces, citing discomfort and difficulty when putting on and removing them. Rehabilitation should be planned to strengthen bone density and increase core strength.
Mechanical instability of vertebral fractures with neurologic compromise is possible. Open surgery such as anterior decompression and stabilization may be needed. Stable, painful compression fractures may be treated by vertebral augmentation either vertebroplasty or kyphoplasty.
The mechanism of pain relief associated with vertebroplasty and kyphoplasty is unknown. Fractured vertebral bodies lose both strength and stiffness. Strength is related to the ability of the vertebral body to bear load, and stiffness limits micromotion within the compromised vertebral body. Restoration of stiffness and strength is augmented by placement of PMMA, reducing painful micromotion [25]. Large amounts of cement are needed to restore stiffness and less for strength [25]. Other mechanisms of pain relief may involve the thermal and cytotoxic reaction of PMMA. It has been hypothesized that the heat of polymerization causes thermal necrosis of neural tissue, explaining pain relief in patients. In vivo studies mapping temperatures from polymerization may rise greater than 50 °C leading to potential damage to interosseous nerves, periosteal nerves [26]. Temperature may also play a role in slowing tumor growth and apoptosis in osteoblasts exposed to 48 °C for 10 min or more. The cytotoxicity of PMMA may also have an antitumoral effect and could be potentially neurotoxic [27].
Vertebroplasty is the percutaneous placement of cement in fractured trabecular bone, leading to an “internal cast” [27] (see Fig. 33.4). The standard indication is for painful compression fractures refractory to medical therapy. The typical causes include osteoporosis, metastatic disease, multiple myeloma, and osteonecrosis. The contraindications are systemic and local infection, uncorrectable coagulopathy, retropulsion of vertebral body or tumor, posterior wall destruction, and radicular symptoms. Benefits for the patients are increased range of motion with pain relief. The procedure is typically done under monitored anesthesia care and as an outpatient procedure.
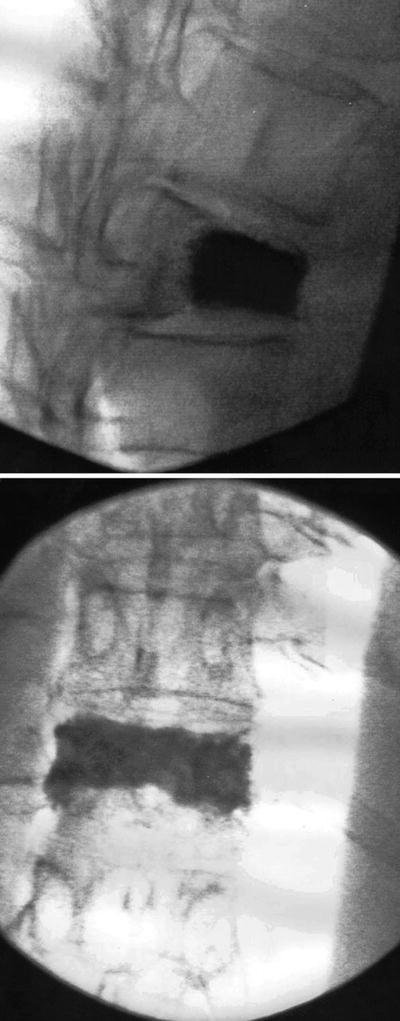
Fig. 33.4
Vertebroplasty is the percutaneous placement of cement in fractured trabecular bone, leading to an “internal cast”
The alternatives are poor. These are conservative medical management, i.e., opioid therapy, physical therapy, bracing, and potential open surgery fixation. The cement is placed through fluoroscopically or CT-guided trocars.
The most common access is the transpedicular approach. Other approaches can be parapedicular, anterolateral (cervical), and posterior (sacral). The complications may include the following: infection, bleeding, pulmonary embolus, local trauma, paralysis, and even death. Fortunately, these complications are rare.
Kyphoplasty has been introduced as an alternative approach [28] (see Fig. 33.5). It is considered a “balloon-assisted vertebroplasty.” This procedure involves percutaneous placement of a balloon in the vertebral body. Through the same large-bore needle, bone cement is placed into the cavity created by the balloon. The balloon is intended to restore vertebral body height in addition to creating the cavity.
Three new modifications on lumbo-thoracic augmentations have been reported. Vertebral body stenting is a new method for vertebral augmentation [29]. Once a compression fracture is reduced with a balloon, a vertebral body stent (VBS) is left in place to maintain the reduction and then stabilized with PMMA. This concept comes from peripheral artery stenting seen in interventional cardiac procedures. So far, it is only reported in human cadaveric specimens [29].
Another similar modification is vesselplasty [30]. The purpose is to obtain control of the volume of void created in the vertebral body, prevent the leakage of bone filler material, and restore vertebral body height. Vesselplasty was designed by Jerry Lin, chairman of A-Spine Holding Group Corporation (Taipei, Taiwan), and was first performed in 2004 by Darwono [30]. A case series of 29 patients who underwent vesselplasty was performed with significant benefits of pain relief, improved mobility, and no complications [30].
Lordoplasty is a modification of vertebroplasty which has been developed as an alternative technique for the treatment of osteoporotic compression fractures [31]. It is known that percutaneous vertebroplasty is successful in producing pain relief but may not reduce the overloading of the anterior column of the spine and the height of the vertebral body. Kyphoplasty can restore the height and lordosis, but kyphotic angle is limited up to 6–9° due to collapse of height after deflating bone temps [31]. In lordoplasty, the vertebral body above and below the compression fracture is accessed with cannulae (see Fig. 33.6) [31]. Through the cannulae, cement is placed and allowed to harden. The compression fracture is also accessed. The fracture is reduced by ligamentotaxis with a lordosing force applied via the cannula in place and using the facet joints as a fulcrum (Fig. 33.7) [31]. The anterior height is reduced and maintained by a cross bolt. The vertebral fracture is augmented with PMMA. Once the cement hardens, the cannulae are removed (Fig. 33.8) [31]. To date, lordoplasty has been reported with successful case reports [31].
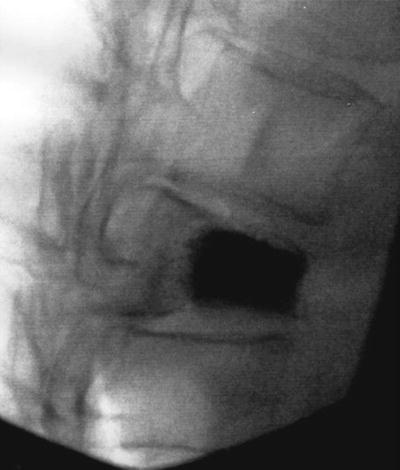


Fig. 33.6
In lordoplasty, the vertebral body above and below the compression fracture is accessed with cannulae

Fig. 33.7
Through the cannulae, cement is placed and allowed to harden. The compression fracture is also accessed. The fracture is reduced by ligamentotaxis with a lordosing force applied via the cannula in place and using the facet joints as a fulcrum

Fig. 33.8
The anterior height is reduced and maintained by a cross bolt. The vertebral fracture is augmented with PMMA. Once the cement hardens, the cannulae are removed
Sacral insufficiency fractures (SIFs) are being identified as a cause of back pain and disability in the elderly population [32]. The mainstay of treatment has been analgesics and physical therapy. Sacroplasty for SIFs evolved from the success of vertebroplasty and kyphoplasty in the treatment of compression fractures of lumbar and thoracic spine. Sacroplasty is the injection of PMMA cement into the fracture zone of the sacral ala with the purpose of pain relief with restoration of mechanical integrity. Using either fluoroscopic and CT guidance, various reported results have been published [32]. A review of the literature reports a multitude of case reports and one prospective observational cohort study [32].
After reviewing published literature, a position statement on percutaneous vertebral augmentation by American Society of Interventional and Therapeutic Neuroradiology, American Association of Neurological Surgeons/Congress of Neurological Surgeons, and American Society of Spine Radiology has determined that the clinical response rate comparing kyphoplasty and vertebroplasty is similar [28]. There is no proven advantage of kyphoplasty compared to vertebroplasty in regard to pain relief, height restoration, and complication rate [28].
Technique
Vertebroplasty and kyphoplasty rely on small incisions to place large-bore needles with radiographic guidance with fluoroscopy or CT guidance. These procedures are either done under general anesthesia or monitored anesthesia care. The procedure itself is not painful especially if local anesthesia is placed, but the duration of the procedure and position of the patient may necessitate at least intravenous sedation. Comorbidities such as poor cardiac dysfunction may need to be monitored. In patients with poor medical condition, medical clearance is advised. Anticoagulations are stopped prior to the procedure. Preoperative antibiotics are usually given as with many surgical implants. Sterile surgical preparation and draping are done.
The critical step is to have an understanding and visualization of the fractured vertebra. Poorly osteoporotic bone, especially in large patients, may offer a challenge. Spinal deformities such as scoliosis may hamper proper visualization of the bone landmarks to perform the procedure successfully. If the bone is not visualized with confidence under fluoroscopy, the case should be aborted. CT guidance is then suggested. The landmarks necessary to perform the procedure under fluoroscopy are the pedicles, vertebral bodies, and disc space in the anterior-posterior, lateral, and oblique views. Real-time three-dimensional fluoroscopic guidance using cone beam CT has been proposed to provide better accuracy and results [33]. A stereotactic guidance system using computer tomography is also proposed to improve accuracy and safety of procedure [34].
There are multiple approaches to access the thoracic and lumbar fractures’ vertebral body [28]. The most common is posterior transpedicular approach. Bipedicular needles are usually placed at each level. Another approach is the parapedicular. For cervical, the anterolateral view is needed, a similar approach to cervical discography. For sacral fracture, a posterior approach is taken.
This author’s approach to lumbar and thoracic fractures is to square the endplates of the fractured vertebral bone on an anterior-posterior view. On the oblique view, the pedicle is identified with clear definition of the medial border. The skin and tissue for the planned entry site are anesthetized with a local anesthetic. The needle will be placed at “eye of the scotty dog” and placed “straight down the barrel.” The needle is gently tapped with a hammer staying lateral to the medial edge of the pedicle. Constant visualization of the needle is needed with fluoroscopy to stay away and lateral to the spinal canal. Needle position is usually anterior to the third of vertebral body on lateral view. PMMA is prepared to allow polymerization in a viscous consistency that still allows passage through the needle. This reduces risk of extravasation. Once confirmed in position on the anterior-posterior and lateral views, the prepared PMMA is injected slowly watching its spread within the vertebral body, under constant fluoroscopy. Once the spread is seen heading to the posterior third, the injection is completed (see Figs. 33.9 and 33.10).
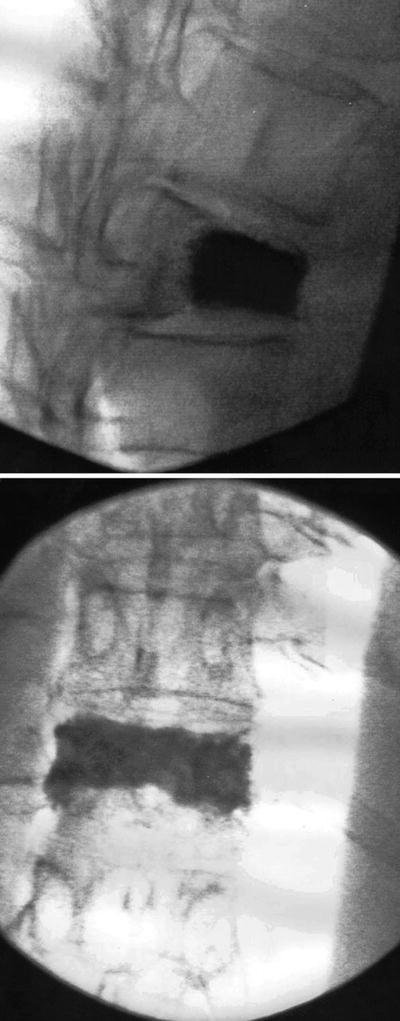
Figs. 33.9 and 33.10
PMMA is prepared to allow polymerization in a viscous consistency that still allows passage through the needle. This reduces risk of extravasation. Once confirmed in position on the ante rior-posterior and lateral views, the prepared PMMA is injected slowly watching its spread within the vertebral body, under constant fluoroscopy. Once the spread is seen heading to the posterior third, the injection is completed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree