Introduction
The indications and imaging options for evaluating patients with suspected vertebral trauma have been discussed in earlier chapters. Once a decision is made that imaging is indicated, radiography will generally be the first study performed. It should be noted, however, that the approach to screening for suspected vertebral trauma has undergone a dramatic and sometimes controversial transition.1–5 Newer imaging options include the use of a low-dose digital radiography unit (Lodox Systems North America, South Lyon, MI) developed in South Africa and magnetic resonance imaging (MRI).6–8 In many large medical centers within the United States, multi-detector computed tomography (MDCT) is replacing conventional radiography for evaluation of suspected cervical injury.9,10 CT has been shown to detect more fractures than radiography, in a faster and more cost-efficient manner.1,11–15 Furthermore, our experience in our trauma center with a large trauma patient population, as well as that of other investigators has indicated that the incidence of noncontiguous, multi-level vertebral injuries is approximately 20%.7,16,17 Therefore, once a decision has been made to perform imaging on any segment of the vertebral column for suspected injury, the entire spinal column should be examined. Although at the present time, radiography is the procedure of choice for the thoracic and lumbar regions, the Harvard group at Massachusetts General Hospital report success with MDCT.2 This chapter will cover five areas: indicators of high risk for injury; mechanisms of injury and their imaging “fingerprints”; the ABCS or imaging “footprints” of injury; the determination of stability following injury; and the significance of injuries. The key to understanding this approach lies in the authors’ premise that all injuries due to a particular mechanism produce the same imaging changes regardless of the location. Thus, a burst fracture of the cervical region looks identical to that in the thoracic and lumbar regions (Fig. 6.1). Furthermore, it is necessary for the reader to understand that while many of the principles discussed here are illustrated using radiographs, the same abnormalities may be seen on CT or even MR images.
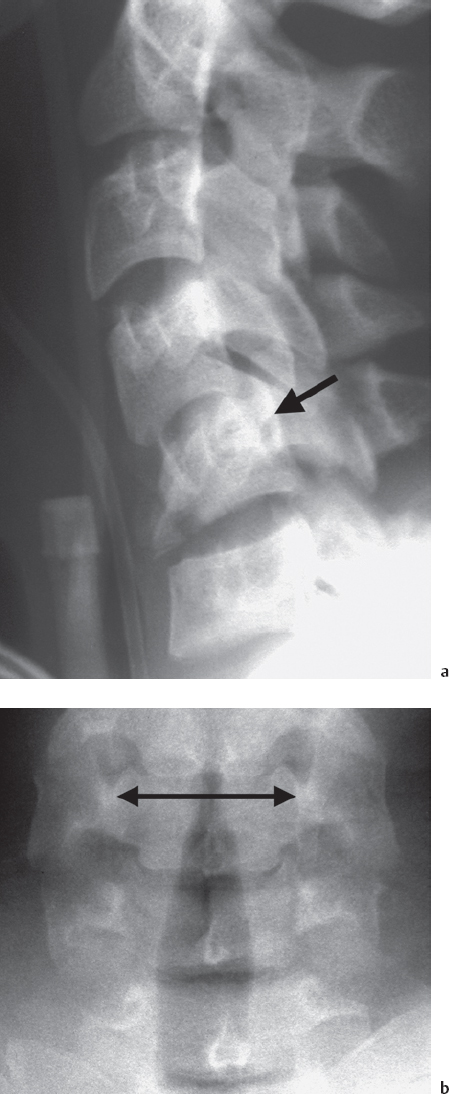
Fig. 6.1 Burst fractures showing similarity between levels. a–c: C5; d–f: L1. a Lateral radiograph shows kyphotic angulation, fragmentation of the body, and posterior displacement of the posterior vertebral line (arrow) of C5. The C4 disk space is narrowed. b Frontal radiograph shows wide interpedicle distance of C5 (double arrow).
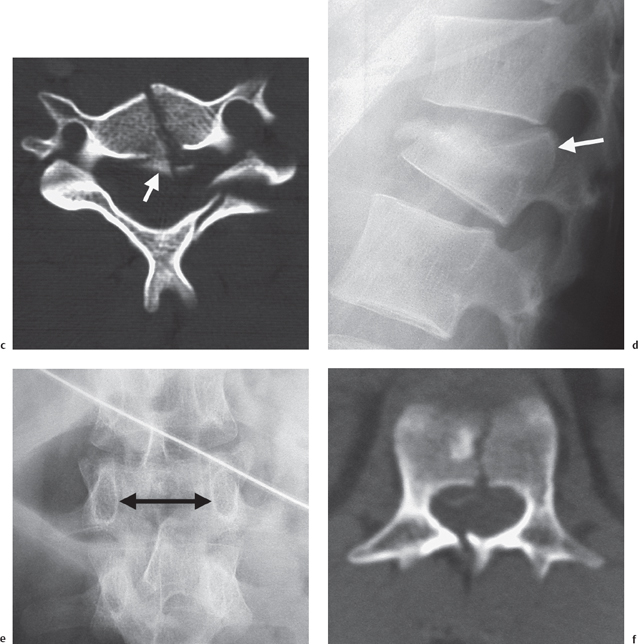
Fig. 6.1 c-f c CT image shows fragmentation of the body of C5 and retropulsion of bone fragments into the vertebral canal (arrow). d Lateral radiograph shows compression of L1, fragmentation, and posterior displacement of the posterior vertebral body line (arrow). Note the narrow T12 disk space. e Frontal radiograph shows wide interpedicle distance of L1 (double arrow). f CT image shows sagittal cleavage of L1. Note the displaced bone fragment in the vertebral canal.
Indicators of High Risk for Injury
No subject has generated more controversy in clinical and radiology circles within the past decade as that of indications for imaging for suspected trauma. In many large medical centers the indications are dictated by trauma protocols. This has led to unnecessary imaging of many patients, with consequent exposure to radiation. Concerns with overuse of radiography and CT as well as attempts at cost-containment have led a number of investigators to assess the indications for imaging in trauma patients. Vandemark, in 1990, published a set of 10 high-risk criteria for indicating the necessity of imaging for possible cervical injury.18 These included high velocity blunt trauma; the presence of multiple fractures; cervical pain, spasm or deformity; altered mental status (of any etiology); drowning or diving accident; a fall of 3 m (10 ft) or greater; any head or facial injury; presence of thoracic and/or lumbar fractures; rigid vertebral disease (ankylosing spondylitis, DISH); and paresthesias or burning in extremities. Blackmore and colleagues investigated fracture risk factors to optimize the use of imaging.19 Ten years later, Hanson and colleagues added mechanism parameters to the clinical findings for determining indications for CT scanning of the cervical spine in trauma patients.20 These included any high-speed crash, defined at over 60 kph (35 mph), or a death at the crash scene. Stiell and colleagues added age over 65 years; crash at over 100 kph or with a rollover or ejection of victims; crash involving motorized recreational vehicles (snowmobiles, wave runners, “quad runners”); or bicycle collision.21 If any of these was present, they recommended radiography.
Two studies looked at low-risk criteria. The first was the National Emergency X-radiography Utilization Study (NEXUS) which identified five criteria that could beused to determine low riskof cervical injury: normal alertness; absence of intoxication; no mid-line cervical tenderness; no painful distracting injuries; and no focal neurological deficits.22,23 Finally, the Canadian group led by Stiell defined additional low risk factors: simple rear-end collision (no rollover, vehicles not pushed into oncoming traffic, not due to being hit by a bus, large truck, or high speed vehicle); and four clinical criteria (patient ambulatory at any time following the crash, patient in sitting position in emergency department, delayedonsetofneck pain, and absenceofmid-line cervical tenderness).21 If these factors were present, they asked the patient to move the neck inflexion, extension, and lateral rotation of 45° to each side.21
Mechanisms of Injury and Their Imaging “Fingerprints”
There are many classifications of vertebral injuries in the medical literature. The authors prefer a simple approach in which there are four main injury mechanisms: flexion, extension, rotary, and shearing. Each of these primary mechanisms may be combined, particularly as the result of secondary impacts that occur, such as when an individual is thrown from a motor vehicle. With the exception of extension injuries, axial loading is frequently a component to the injury. Most important, however, is the fact that when an injury occurs, it produces a series of indelible radiographic changes that allow the informed observer to tell not only the mechanism of the injury, but also to alert him or her to look for subtle findings that represent the full extent of that injury. We call these changes the radiological “fingerprints.”
Flexion injuries are the most frequent types to be encountered in patients who have suffered vertebral trauma. The common thread of all flexion injuries is that forward bending occurs through a fulcrum centered on the posterior third of the intervertebral disks. This produces anterior compression and posterior distraction (Fig. 6.2). This mechanism produces four distinct subtypes of injury: simple, burst, distraction, and dislocation. Simple injuries produce compression of the superior or inferior vertebral endplates of the involved vertebrae. The posterior parts of the vertebral body as well as the posterior elements remain intact. Simple injuries typically produce a wedge-shaped vertebra (Fig. 6.3). The disk space above a simple fracture, as with all flexion injuries, is typically narrowed. These injuries rarely produce neurological deficits.
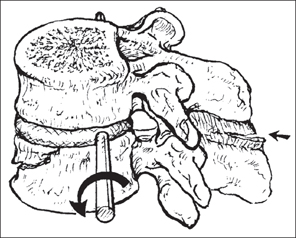
Fig. 6.2 Drawing showing mechanism of flexion. Forward flexion (curved arrow) with the posterior third of the disk space as the fulcrum produces anterior compression. Further force produces posterior distraction (straight arrow).

Fig. 6.3 Simple compression fracture of L1. Lateral radiograph shows anterior compression without disruption of the posterior vertebral body line.
Burst fractures are the result of severe compressive forces that literally explode the vertebra. The vertebral body is comminuted and there is retropulsion of bone fragments that encroach upon the vertebral canal. Typically, the posterior arch of the vertebra is fractured as well. Of particular importance in identifying burst fractures are three radiographic signs: severe compression of the vertebral body, disruption of the posterior body line, and widening of the interpedicle distance. These features may all be seen in Figures 6.1 and 6.4.
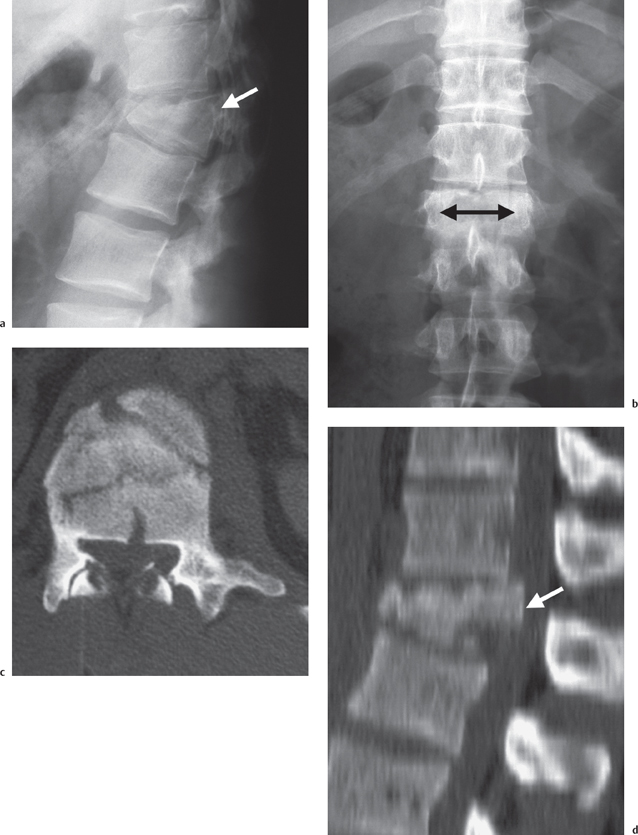
Fig. 6.4 L1 burst fracture. a Lateral radiograph shows compression, fragmentation, and disruption of the posterior vertebral body line of L1 (arrow). b Frontal radiograph shows a compressed vertebra and widening of the interpedicle distance of L1 (double arrow). c CT image through L1 shows comminution and flattening of the posterior vertebral body line. There are bone fragments in the vertebral canal. d Sagittal CT reconstruction shows the degree of canal compromise from retropulsed fragments (arrow).
The posterior vertebral body line is a single uninterrupted structure in the cervical and upper thoracic region. In the lower thoracic and lumbar regions, a nutrient vessel interrupts it centrally. At C2, this line should extend cephalad along the posterior aspect of the dens. Any displacement, duplication, angulation, rotation, or absence of this line is abnormal. In a typical burst fracture, there is posterior displacement of this line on lateral radiographs, and this displacement represents the retropulsed bone fragment within the vertebral canal. CT (and/or MRI) will confirm this (Figs. 6.1–6.4).
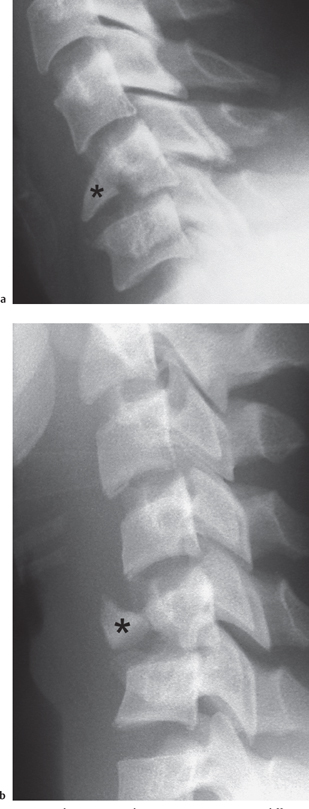
Fig. 6.5 Flexion “teardrop” injuries in two different patients. Forward flexion has produced anterior inferior “teardrop” fragments (*). In both instances there is slight retrolisthesis of the vertebral bodies.
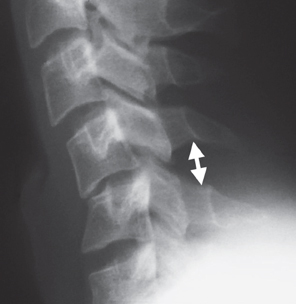
Fig. 6.6 Hyperflexion sprain C4-5. Note kyphotic angulation and widening of the interlaminar space (double arrow).
The interpedicle distance is measured from the medial sclerotic areas of the pedicles on frontal radiographs. The difference in the distance between two contiguous levels should never exceed 2 mm. Burst fractures, particularly those of the sagittal cleavage variety, widen this space, a finding which may be frequently seen on frontal radiographs (Fig. 6.4b). Another manifestation of sagittal cleavage is widening of the facet joints at the involved level(s). The implication of this finding, when encountered on a frontal radiograph, is that the vertebra has been split along the sagittal plane both through the body as well as through the lamina. A variation of the burst fracture is the flexion “teardrop” injury in the cervical spine. In this variant, a triangular fragment of bone is displaced from the anteroinferior margin of the vertebral body. There is slight retrolisthesis of the remainder of the body (Fig. 6.5). When this finding is associated with evidence of posterior distraction, severe neurological deficits result.
Distraction injuries occur primarily in two varieties. The first is primarily a ligamentous and soft tissue type of injury. In the cervical region, this is referred to as the hyperflexion sprain. If fractures occur in association with this injury, they are usually small avulsion fractures. In this injury, the posterior ligaments are torn as well as the posterior longitudinal ligament and the posterior third of the intervertebral disks. This produces widening of the interlaminar or interspinous spaces, widening of the facets, and varying degrees of anterolisthesis (Figs. 6.6, 6.7). Intervertebral disk herniation frequently occurs with distraction injuries.
A pure distraction-type of injury also occurs in the thoracolumbar region where the findings are similar to those in the cervical region. One feature, however, that is fairly unique in the thoracic and lumbar distraction injuries are the so-called “naked facets” (Fig. 6.8).
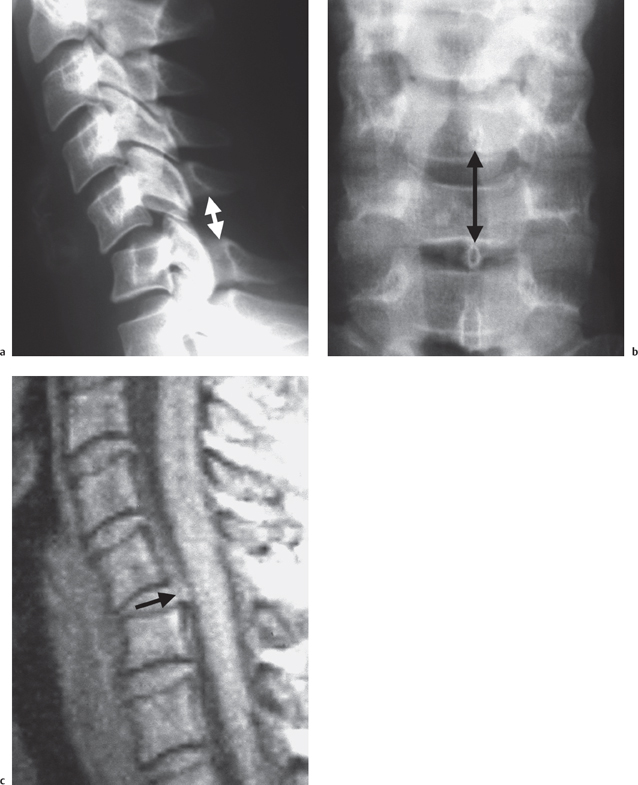
Fig. 6.7 Hyperflexion sprain C5-C6. a Lateral radiograph shows kyphotic angulation, anterolisthesis of C5 on C6, and widening of the interlaminar space (double arrow), and facet joints. b Frontal view shows widening of the interspinous distance (double arrow). c Proton density-weighted MR sagittal image shows rupture of the posterior longitudinal ligament and disk herniation at C5-C6 (arrow).
The second form of distraction injury is one in which there are horizontally oriented fractures through the vertebral body that may continue through the pedicles, articular pillars, laminae, and/or spinous processes. These are better known as the Chance-type injuries and are the result of forward flexion on a lap type seat-belt (Fig. 6.9). While one level appears to be involved from a radiographic standpoint, MRI frequently shows evidence of injury to contiguous levels (Fig. 6.10). Patients with Chance-type fractures frequently suffer abdominal visceral injuries.
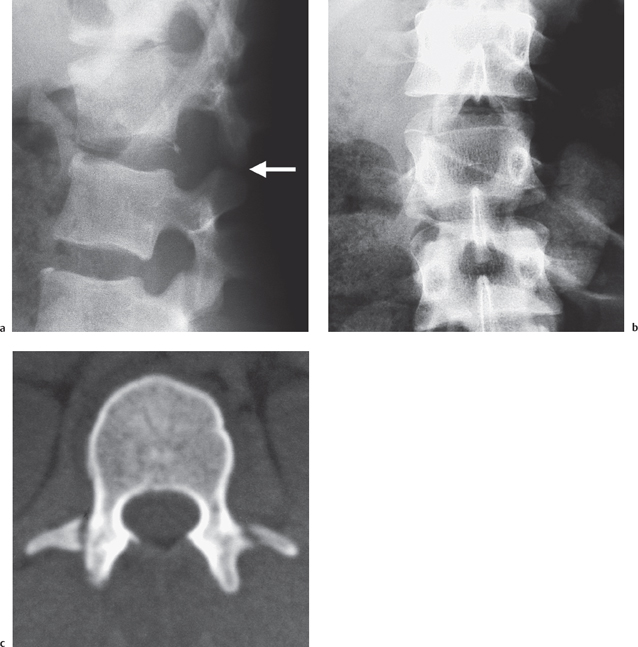
Fig. 6.8 L1-L2 flexion distraction injury with perched facets. a Lateral radiograph shows widening of the L1 disk space and perching of the facets of L1 on L2 (arrow). There is a small avulsion fragment from the posterior inferior margin of L1, as well. b Frontal radiograph shows widening of the interspinous space between L1 and L2 and “naked” facets on the left. c CT image through the injury shows absence of posterior elements from the adjoining vertebra and “naked” facets of L1. There are also bilateral transverse process fractures.
Flexion-dislocation injuries are the result of severe distractive forces. These may or may not be associated with fractures. A prime example of this type of injury is a unilateral (Fig. 6.11) or bilateral jumped and locked facet. These injuries frequently produce severe neurological deficits.
The “fingerprints” of flexion injuries are summarized in Table 6.1.
Extension injuries are much more common in the cervical region than in the thoracic and lumbar regions. The reason for this is the greater mobility of the cervical spine. All extension injuries are the result of varying degrees of backward bending where the fulcrum of motion is at the level of the articular pillars.
The radiographic hallmark of extension injuries is widening of the intervertebral disk space below the level of injury. In the cervical region, widening is frequently accompanied by an avulsion of thesion of the anterosuperior lip of the subjacent vertebral body. If the force is severe enough to disrupt the anterior longitudinal ligament and intervertebral disk, retrolisthesis may occur. In the most severe cases, the articular pillars are crushed since they are the fulcrum of motion.
There are three subtypes of extension injury: simple, distraction, and dislocation. A simple extension injury is usually nothing more than an avulsion of the anterosuperior portion of a vertebral body with minimal or no widening of the disk space above. This injury usually produces no neurological deficits. The distraction injury produces obvious widening of the intervertebral disk space with or without an avulsion fracture of the subjacent vertebra. The most common type of these injuries is the “hangman’s” fracture of C2 (Fig. 6.12). A more severe type of distraction injury is the so-called hyperextension sprain (Fig. 6.13). This variant occurs most commonly in elderly individuals who have suffered an injury to the chin. Hyperextension sprains produce widening of the intervertebral disk space and retrolisthesis (Fig. 6.13). These patients have severe neurological deficits, usually a central cord syndrome, whereas those with a hangman’s fracture usually suffer no neurological deficits (unless the injury occurred during a judicial hanging).
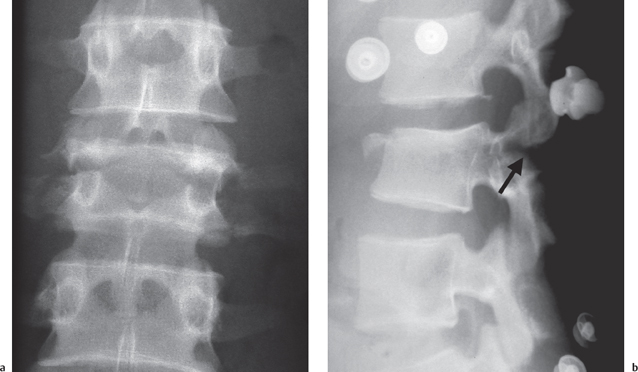
Fig. 6.9 Chance-type fracture of L3 as a result of a lap belt. a Frontal radiograph shows horizontal fractures involving the vertebral body, pedicles, and transverse processes. b Lateral radiograph shows fragmentation of the vertebral body and posterior distraction. Note the fractures through the pedicles (arrow).
| Flexion | Compression, fragmentation, burst of vertebral bodies “Teardrop” fragments Anterolisthesis Disrupted posterior vertebral body line Wide interlaminar (interspinous) space Locked facets Narrow disk space above Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|